What Services Are Included In The Consolidated Billing Of The Snf Pps?
Start Preamble Start Printed Page 42424
AGENCY:
Centers for Medicare & Medicaid Services (CMS), HHS.
ACTION:
Final rule.
SUMMARY:
This final rule updates the payment rates used under the prospective payment system (PPS) for skilled nursing facilities (SNFs) for fiscal year (FY) 2022. In addition, the final rule includes a forecast error adjustment for FY 2022, updates the diagnosis code mappings used under the Patient Driven Payment Model (PDPM), rebases and revises the SNF market basket, implements a recently-enacted SNF consolidated billing exclusion along with the required proportional reduction in the SNF PPS base rates, and includes a discussion of a PDPM parity adjustment. In addition, the final rule includes updates for the SNF Quality Reporting Program (QRP) and the SNF Value-Based Purchasing (VBP) Program, including a policy to suppress the use of the SNF readmission measure for scoring and payment adjustment purposes in the FY 2022 SNF VBP Program because we have determined that circumstances caused by the public health emergency for COVID-19 have significantly affected the validity and reliability of the measure and resulting performance scores. We are also finalizing a technical correction to the physical environment requirements that Long-Term Care facilities must meet in order to participate in the Medicare and Medicaid programs.
DATES:
These regulations are effective on October 1, 2021.
Start Further Info
FOR FURTHER INFORMATION CONTACT:
Penny Gershman, (410) 786-6643, for information related to SNF PPS clinical issues.
Anthony Hodge, (410) 786-6645, for information related to consolidated billing, and payment for SNF-level swing-bed services.
John Kane, (410) 786-0557, for information related to the development of the payment rates and case-mix indexes, and general information.
Kia Burwell, (410) 786-7816, for information related to the wage index.
Heidi Magladry, (410) 786-6034, for information related to the skilled nursing facility quality reporting program.
Lang Le, (410) 786-5693, for information related to the skilled nursing facility value-based purchasing program.
Kristin Shifflett, (410) 786-4133, for information related to the long-term care conditions of participation.
End Further Info End Preamble
SUPPLEMENTARY INFORMATION:
Availability of Certain Tables Exclusively Through the Internet on the CMS Website
As discussed in the FY 2014 SNF PPS final rule (78 FR 47936), tables setting forth the Wage Index for Urban Areas Based on CBSA Labor Market Areas and the Wage Index Based on CBSA Labor Market Areas for Rural Areas are no longer published in the Federal Register. Instead, these tables are available exclusively through the internet on the CMS website. The wage index tables for this final rule can be accessed on the SNF PPS Wage Index home page, at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/SNFPPS/WageIndex.html.
Readers who experience any problems accessing any of these online SNF PPS wage index tables should contact Kia Burwell at (410) 786-7816.
To assist readers in referencing sections contained in this document, we are providing the following Table of Contents.
Table of Contents
I. Executive Summary
A. Purpose
B. Summary of Major Provisions
C. Summary of Cost and Benefits
D. Advancing Health Information Exchange
II. Background on SNF PPS
A. Statutory Basis and Scope
B. Initial Transition for the SNF PPS
C. Required Annual Rate Updates
III. Analysis and Responses to Public Comments on the FY 2022 SNF PPS Proposed Rule
A. General Comments on the FY 2022 SNF PPS Proposed Rule
IV. SNF PPS Rate Setting Methodology and FY 2022 Update
A. Federal Base Rates
B. SNF Market Basket Update
C. Case-Mix Adjustment
D. Wage Index Adjustment
E. SNF Value-Based Purchasing Program
F. Adjusted Rate Computation Example
V. Additional Aspects of the SNF PPS
A. SNF Level of Care—Administrative Presumption
B. Consolidated Billing
C. Payment for SNF-Level Swing-Bed Services
D. Revisions to the Regulation Text
VI. Other SNF PPS Issues
A. Changes to SNF PPS Wage Index
B. Technical Updates to PDPM ICD-10 Mappings
C. Recalibrating the PDPM Parity Adjustment
VII. Skilled Nursing Facility (SNF) Quality Reporting Program (QRP)
VIII. Skilled Nursing Facility Value-Based Purchasing Program (SNF VBP)
IX. Long-Term Care Facilities: Physical Environment Requirements
X. Collection of Information Requirements
XI. Economic Analyses
A. Regulatory Impact Analysis
B. Regulatory Flexibility Act Analysis
C. Unfunded Mandates Reform Act Analysis
D. Federalism Analysis
E. Reducing Regulation and Controlling Regulatory Costs
F. Congressional Review Act
G. Regulatory Review Costs
I. Executive Summary
A. Purpose
This final rule updates the SNF prospective payment rates for fiscal year (FY) 2022 as required under section 1888(e)(4)(E) of the Social Security Act (the Act). It also responds to section 1888(e)(4)(H) of the Act, which requires the Secretary to provide for publication of certain specified information relating to the payment update (see section II.C. of this final rule) in the Federal Register, before the August 1 that precedes the start of each FY. As discussed in section VI.A. of this final rule, it will also rebase and revise the SNF market basket index, including updating the base year from 2014 to 2018. As discussed in section V.D. of this final rule, it also makes revisions in the regulation text to exclude from SNF consolidated billing certain blood clotting factors and items and services related to the furnishing of such factors effective for items and services furnished on or after October 1, 2021, as required by the Consolidated Appropriations Act, 2021 (Pub. L. 116-260, enacted December 27, 2020), as well as certain other conforming revisions. In addition, as required under section 1888(e)(4)(G)(iii) of the Act, as added by section 103(b) of the BBRA 1999, we provide for a proportional reduction in the Part A SNF PPS base rates to account for this exclusion, as described in section IV.B.6. of this final rule. We also make changes to the code mappings used under the SNF PPS for classifying patients into case-mix Start Printed Page 42425 groups. Additionally, this final rule includes a forecast error adjustment for FY 2022. This final rule also includes a discussion of a PDPM parity adjustment. Finally, this final rule also updates requirements for the Skilled Nursing Facility Quality Reporting Program (SNF QRP) and the Skilled Nursing Facility Value-Based Purchasing Program (SNF VBP), including a policy to suppress the use of the SNF readmission measure for scoring and payment adjustment purposes in the FY 2022 SNF VBP Program because we have determined that circumstances caused by the public health emergency for COVID-19 have significantly affected the validity and reliability of the measure and resulting performance scores.
B. Summary of Major Provisions
In accordance with sections 1888(e)(4)(E)(ii)(IV) and (e)(5) of the Act, the Federal rates in this final rule reflect an update to the rates that we published in the SNF PPS final rule for FY 2021 (85 FR 47594, August 5, 2020). We are also rebasing and revising the SNF market basket index, including updating the base year from 2014 to 2018. This final rule includes revisions to the regulation text to exclude from SNF consolidated billing certain blood clotting factors and items and services related to the furnishing of such factors effective for items and services furnished on or after October 1, 2021, as required by the Consolidated Appropriations Act, 2021, as well as certain conforming revisions. We are also making a required reduction in the SNF PPS base rates to account for this new exclusion. This final rule includes revisions to the International Classification of Diseases, Version 10 (ICD-10) code mappings used under PDPM to classify patients into case-mix groups. Additionally, this final rule includes a forecast error adjustment for FY 2022. This final rule also includes a discussion of a PDPM parity adjustment, used to implement PDPM in a budget neutral manner.
This final rule updates requirements for the SNF QRP, including the adoption of two new measures beginning with the FY 2023 SNF QRP: The SNF Healthcare Associated Infections (HAI) Requiring Hospitalization measure; and the COVID-19 Vaccination Coverage among Healthcare Personnel (HCP) measure. The COVID-19 Vaccination Coverage among HCP measure requires that SNFs use the Centers for Disease Control and Prevention (CDC)/National Healthcare Safety Network (NHSN) to submit data on the measure. We are also finalizing our proposal to modify the denominator for the Transfer of Health Information to the Patient—Post Acute Care (PAC) measure. Finally, we are finalizing our proposal to revise the number of quarters used for publicly reporting certain SNF QRP measures due to the public health emergency (PHE).
Additionally, we are finalizing several updates for the SNF VBP Program including a policy to suppress the Skilled Nursing Facility 30-Day All-Cause Readmission Measure (SNFRM) for the FY 2022 SNF VBP Program Year for scoring, adjusting and codifying the policy at § 413.338(g). We are also updating the Phase One Review and Corrections policy to implement a claims "snapshot" policy which aligns the review and corrections policy for the SNF VBP Program with the review and corrections policy we use in other value-based purchasing programs and codifying the policy at § 413.338(e)(1) of our regulations. We are also making a technical update to the instructions for a SNF to request an extraordinary circumstances exception and codifying that update at § 413.338(d)(4)(ii) of our regulations. In addition, we are finalizing a technical correction to the physical environment requirements for LTC facilities by revising § 483.90(d)(1) and adding § 483.90(d)(3).
C. Summary of Cost and Benefits

D. Advancing Health Information Exchange
The Department of Health and Human Services (HHS) has a number of initiatives designed to encourage and support the adoption of interoperable health information technology and to promote nationwide health information exchange to improve health care and patient access to their health information.
To further interoperability in post-acute care settings, CMS and the Office of the National Coordinator for Health Information Technology (ONC) participate in the Post-Acute Care Interoperability Workgroup (PACIO) (https://pacioproject.org/) to facilitate collaboration with industry stakeholders to develop FHIR standards. These standards could support the exchange and reuse of patient assessment data derived from the minimum data set (MDS), inpatient rehabilitation facility patient assessment instrument (IRF-PAI), long term care hospital continuity assessment record and evaluation (LCDS), outcome and assessment information set (OASIS), and other sources. The PACIO Project has focused on FHIR implementation guides for functional status, cognitive status and new use cases on advance directives and speech, and language pathology. We encourage post-acute care (PAC) provider and health information technology (IT) vendor participation as these efforts advance.
The CMS Data Element Library (DEL) continues to be updated and serves as the authoritative resource for PAC assessment data elements and their associated mappings to health IT standards such as Logical Observation Identifiers Names and Codes (LOINC) and Systematized Nomenclature of Medicine Clinical Terms (SNOMED). The DEL furthers CMS' goal of data standardization and interoperability. When combined with digital information systems that capture and maintain these coded elements, their standardized clinical content can reduce Start Printed Page 42426 provider burden by supporting the exchange of standardized healthcare data; supporting provider exchange of electronic health information for care coordination, person-centered care; and supporting real-time, data driven, clinical decision making. Standards in the Data Element Library (https://del.cms.gov/DELWeb/pubHome) can be referenced on the CMS website and in the ONC Interoperability Standards Advisory (ISA). The 2021 ISA is available at https://www.healthit.gov/isa.
The 21st Century Cures Act (Cures Act) (Pub. L. 114-255, enacted December 13, 2016) requires HHS to take new steps to enable the electronic sharing of health information ensuring interoperability for providers and settings across the care continuum. The Cures Act includes a trusted exchange framework and common agreement (TEFCA) provision[1] that will enable the nationwide exchange of electronic health information across health information networks and provide an important way to enable bi-directional health information exchange in the future. For more information on current developments related to TEFCA, we refer readers to https://www.healthit.gov/topic/interoperability/trusted-exchange-framework-and-common-agreement and https://rce.sequoiaproject.org/.
The ONC final rule entitled "21st Century Cures Act: Interoperability, Information Blocking, and the ONC Health IT Certification Program" (85 FR 25642) published in the May 1, 2020, Federal Register (hereinafter referred to as "ONC Cures Act Final Rule") established policies related to information blocking as authorized under section 4004 of the 21st Century Cures Act. Information blocking is generally defined as a practice by a health IT developer of certified health IT, health information network, health information exchange, or health care provider that, except as required by law or specified by the HHS Secretary as a reasonable and necessary activity, is likely to interfere with access, exchange, or use of electronic health information. The definition of information blocking includes a knowledge standard, which is different for health care providers than for health IT developers of certified health IT and health information networks or health information exchanges. A healthcare provider must know that the practice is unreasonable, as well as likely to interfere with access, exchange, or use of electronic health information. To deter information blocking, health IT developers of certified health IT, health information networks and health information exchanges whom the HHS Inspector General determines, following an investigation, have committed information blocking, are subject to civil monetary penalties of up to $1 million per violation. Appropriate disincentives for health care providers are expected to be established by the Secretary through future rulemaking. Stakeholders can learn more about information blocking at https://www.healthit.gov/curesrule/final-rule-policy/information-blocking. ONC has posted information resources including fact sheets (https://www.healthit.gov/curesrule/resources/fact-sheets), frequently asked questions (https://www.healthit.gov/curesrule/resources/information-blocking-faqs), and recorded webinars (https://www.healthit.gov/curesrule/resources/webinars).
We invite providers to learn more about these important developments and how they are likely to affect SNFs.
II. Background on SNF PPS
A. Statutory Basis and Scope
As amended by section 4432 of the Balanced Budget Act of 1997 (BBA 1997) (Pub. L. 105-33, enacted August 5, 1997), section 1888(e) of the Act provides for the implementation of a PPS for SNFs. This methodology uses prospective, case-mix adjusted per diem payment rates applicable to all covered SNF services defined in section 1888(e)(2)(A) of the Act. The SNF PPS is effective for cost reporting periods beginning on or after July 1, 1998, and covers all costs of furnishing covered SNF services (routine, ancillary, and capital-related costs) other than costs associated with approved educational activities and bad debts. Under section 1888(e)(2)(A)(i) of the Act, covered SNF services include post-hospital extended care services for which benefits are provided under Part A, as well as those items and services (other than a small number of excluded services, such as physicians' services) for which payment may otherwise be made under Part B and which are furnished to Medicare beneficiaries who are residents in a SNF during a covered Part A stay. A comprehensive discussion of these provisions appears in the May 12, 1998 interim final rule (63 FR 26252). In addition, a detailed discussion of the legislative history of the SNF PPS is available online at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/SNFPPS/Downloads/Legislative_History_2018-10-01.pdf.
Section 215(a) of the Protecting Access to Medicare Act of 2014 (PAMA) (Pub. L. 113-93, enacted April 1, 2014) added section 1888(g) to the Act requiring the Secretary to specify an all-cause all-condition hospital readmission measure and an all-condition risk-adjusted potentially preventable hospital readmission measure for the SNF setting. Additionally, section 215(b) of PAMA added section 1888(h) to the Act requiring the Secretary to implement a VBP program for SNFs. Finally, section 2(c)(4) of the IMPACT Act amended section 1888(e)(6) of the Act, which requires the Secretary to implement a QRP for SNFs under which SNFs report data on measures and resident assessment data.
B. Initial Transition for the SNF PPS
Under sections 1888(e)(1)(A) and (e)(11) of the Act, the SNF PPS included an initial, three-phase transition that blended a facility-specific rate (reflecting the individual facility's historical cost experience) with the Federal case-mix adjusted rate. The transition extended through the facility's first 3 cost reporting periods under the PPS, up to and including the one that began in FY 2001. Thus, the SNF PPS is no longer operating under the transition, as all facilities have been paid at the full Federal rate effective with cost reporting periods beginning in FY 2002. As we now base payments for SNFs entirely on the adjusted Federal per diem rates, we no longer include adjustment factors under the transition related to facility-specific rates for the upcoming FY.
C. Required Annual Rate Updates
Section 1888(e)(4)(E) of the Act requires the SNF PPS payment rates to be updated annually. The most recent annual update occurred in a final rule that set forth updates to the SNF PPS payment rates for FY 2021 (85 FR 47594, August 5, 2020).
Section 1888(e)(4)(H) of the Act specifies that we provide for publication annually in the Federal Register the following:
- The unadjusted Federal per diem rates to be applied to days of covered SNF services furnished during the upcoming FY.
- The case-mix classification system to be applied for these services during the upcoming FY.
- The factors to be applied in making the area wage adjustment for these services. Start Printed Page 42427
Along with other revisions discussed later in this preamble, this final rule provides the required annual updates to the per diem payment rates for SNFs for FY 2022.
III. Analysis and Responses to Public Comments on the FY 2022 SNF PPS Proposed Rule
In response to the publication of the FY 2022 SNF PPS proposed rule, we received 338 public comments from individuals, providers, corporations, government agencies, private citizens, trade associations, and major organizations. The following are brief summaries of each proposed provision, a summary of the public comments that we received related to that proposal, and our responses to the comments.
A. General Comments on the FY 2022 SNF PPS Proposed Rule
In addition to the comments we received on specific proposals contained within the proposed rule (which we address later in this final rule), commenters also submitted the following, more general, observations on the SNF PPS and SNF care generally. A discussion of these comments, along with our responses, appears below.
Comment: Commenters submitted numerous comments and recommendations that are outside the scope of the proposed rule addressing a number of different policies, including the Coronavirus disease 2019 (COVID-19) pandemic. This included comments on the flexibilities provided to SNFs during the PHE, specifically through the waivers issued under sections 1135 and 1812(f) of the Act. Commenters also expressed concerns about the substantial additional costs due to the PHE that would be permanent due to changes in patient care, infection control staff and equipment, personal protective equipment (PPE), reporting requirements, increased wages, increased food prices, and other necessary costs. Some commenters who received CARES Act Provider Relief funds indicated that those funds were not enough to cover these costs. Additionally, a few commenters from rural areas stated that their facilities were heavily impacted from the additional costs, particularly the need to raise wages, and that this could affect patients' access to care.
Response: We greatly appreciate these comments and suggestions for revisions to policies under the SNF PPS. However, because these comments are outside the scope of the current rulemaking, we are not addressing them in this final rule. We may take them under consideration in future rulemaking.
IV. SNF PPS Rate Setting Methodology and FY 2022 Update
A. Federal Base Rates
Under section 1888(e)(4) of the Act, the SNF PPS uses per diem Federal payment rates based on mean SNF costs in a base year (FY 1995) updated for inflation to the first effective period of the PPS. We developed the Federal payment rates using allowable costs from hospital-based and freestanding SNF cost reports for reporting periods beginning in FY 1995. The data used in developing the Federal rates also incorporated a Part B add-on, which is an estimate of the amounts that, prior to the SNF PPS, would be payable under Part B for covered SNF services furnished to individuals during the course of a covered Part A stay in a SNF.
In developing the rates for the initial period, we updated costs to the first effective year of the PPS (the 15-month period beginning July 1, 1998) using a SNF market basket index, and then standardized for geographic variations in wages and for the costs of facility differences in case mix. In compiling the database used to compute the Federal payment rates, we excluded those providers that received new provider exemptions from the routine cost limits, as well as costs related to payments for exceptions to the routine cost limits. Using the formula that the BBA 1997 prescribed, we set the Federal rates at a level equal to the weighted mean of freestanding costs plus 50 percent of the difference between the freestanding mean and weighted mean of all SNF costs (hospital-based and freestanding) combined. We computed and applied separately the payment rates for facilities located in urban and rural areas, and adjusted the portion of the Federal rate attributable to wage-related costs by a wage index to reflect geographic variations in wages.
B. SNF Market Basket Update
1. SNF Market Basket Index
Section 1888(e)(5)(A) of the Act requires us to establish a SNF market basket index that reflects changes over time in the prices of an appropriate mix of goods and services included in covered SNF services. Accordingly, we have developed a SNF market basket index that encompasses the most commonly used cost categories for SNF routine services, ancillary services, and capital-related expenses. In the SNF PPS final rule for FY 2018 (82 FR 36548 through 36566), we rebased and revised the market basket index, which included updating the base year from FY 2010 to 2014. In the proposed rule, we proposed to rebase and revise the market basket index and update the base year from 2014 to 2018. See section VI.A. of this final rule for more information.
The SNF market basket index is used to compute the market basket percentage change that is used to update the SNF Federal rates on an annual basis, as required by section 1888(e)(4)(E)(ii)(IV) of the Act. This market basket percentage update is adjusted by a forecast error correction, if applicable, and then further adjusted by the application of a productivity adjustment as required by section 1888(e)(5)(B)(ii) of the Act and described in section IV.B.2.d. of this final rule.
We proposed a FY 2022 SNF market basket percentage of 2.3 percent based on IGI's fourth quarter 2020 forecast of the proposed 2018-based SNF market basket (before application of the forecast error adjustment and productivity adjustment). We also proposed that if more recent data subsequently become available (for example, a more recent estimate of the market basket and/or the productivity adjustment), we would use such data, if appropriate, to determine the FY 2022 SNF market basket percentage change, labor-related share relative importance, forecast error adjustment, or productivity adjustment in the SNF PPS final rule.
Since the proposed rule, we have updated the FY 2022 market basket percentage increase based on IGI's second quarter 2021 forecast with historical data through the first quarter of 2021. The FY 2022 growth rate of the 2018-based SNF market basket is estimated to be 2.7 percent.
In section IV.B.2.e. of this final rule, we discuss the 2 percent reduction applied to the market basket update for those SNFs that fail to submit measures data as required by section 1888(e)(6)(A) of the Act.
2. Use of the SNF Market Basket Percentage
Section 1888(e)(5)(B) of the Act defines the SNF market basket percentage as the percentage change in the SNF market basket index from the midpoint of the previous FY to the midpoint of the current FY. For the Federal rates set forth in this final rule, we use the percentage change in the SNF market basket index to compute the update factor for FY 2022. This factor is based on the FY 2022 percentage increase in the 2018-based SNF market basket index reflecting routine, ancillary, and capital-related expenses. Start Printed Page 42428 As stated previously, in the proposed rule, the SNF market basket percentage update was estimated to be 2.3 percent for FY 2022 based on IGI's fourth quarter 2020 forecast. For this final rule, based on IGI's second quarter 2021 forecast with historical data through the first quarter of 2021, the FY 2022 growth rate of the 2018-based SNF market basket is estimated to be 2.7 percent.
A discussion of the comments received on applying the FY 2022 SNF market basket percentage increase to the SNF PPS rates, along with our responses, may be found below.
Comment: Several commenters stated their support for the proposed FY 2022 payment update of 1.3 percent reflecting the proposed market basket update, the productivity adjustment, and the forecast error adjustment. A few commenters, while noting appreciation for the 1.3 percent update, also noted that it is very low in comparison to the increased costs they are facing as a result of the COVID-19 pandemic and that many facilities are already operating on thin margins.
Response: The proposed FY 2022 SNF payment update of 1.3 percent reflected the forecast available at that time of the market basket update, productivity adjustment, and forecast error. As stated in the proposed rule, we proposed to use the most recent forecast of data available to determine the final FY 2022 SNF payment update. The current estimate of final FY 2022 SNF payment update is 1.2 percent based on the IGI second quarter 2021 forecast of the 2018-based SNF market basket update (2.7 percent), reduced by the productivity adjustment (0.7 percentage point), and the application of the FY 2020 forecast error adjustment (−0.8 percentage point). For this final rule, we have incorporated the most recent historical data and forecasts provided by IHS Global Inc., including experience during the PHE, in order to capture the price and wage pressures facing SNFs in FY 2022. By incorporating the most recent estimates available of the market basket update and productivity adjustment, we believe these data reflect the best available projection of input price inflation faced by SNFs for FY 2022, adjusted for economy-wide productivity, which is required by statute.
Comment: The Medicare Payment Advisory Commission (MedPAC) commented that they recommend that the Congress eliminate the update to SNF payments for FY 2022. Moreover, MedPAC stated that the aggregate Medicare margin for freestanding SNFs in 2019 was 11.3 percent, the 20th consecutive year that this margin has exceeded 10 percent. MedPAC further stated that the projected margin for FY 2022 indicated that while payments might need to be reduced to more closely align them with the cost to treat beneficiaries, they also understand that the lasting impacts of COVID-19 on SNFs are uncertain which is why they proceeded cautiously in recommending no update rather than reductions to payments.
Response: We appreciate MedPAC's recommendation on the SNF annual update factor and the uncertainty for SNFs posed by the PHE. However, we are required to update SNF PPS payments by the market basket update, as required by section 1888(e)(4)(E)(ii)(IV) of the Act, and then further adjust the market basket update by the application of a productivity adjustment, as required by section 1888(e)(5)(B)(ii) of the Act. This productivity-adjusted market basket percentage update is further adjusted by a forecast error correction, if applicable.
After considering the comments received on the FY 2022 SNF market basket update factor, we are finalizing the update factor of 2.7 percent to the SNF PPS base rates for FY 2022 (prior to the application of the forecast error adjustment and productivity adjustment, which are discussed below).
3. Forecast Error Adjustment
As discussed in the June 10, 2003 supplemental proposed rule (68 FR 34768) and finalized in the August 4, 2003 final rule (68 FR 46057 through 46059), § 413.337(d)(2) provides for an adjustment to account for market basket forecast error. The initial adjustment for market basket forecast error applied to the update of the FY 2003 rate for FY 2004, and took into account the cumulative forecast error for the period from FY 2000 through FY 2002, resulting in an increase of 3.26 percent to the FY 2004 update. Subsequent adjustments in succeeding FYs take into account the forecast error from the most recently available FY for which there is final data, and apply the difference between the forecasted and actual change in the market basket when the difference exceeds a specified threshold. We originally used a 0.25 percentage point threshold for this purpose; however, for the reasons specified in the FY 2008 SNF PPS final rule (72 FR 43425), we adopted a 0.5 percentage point threshold effective for FY 2008 and subsequent FYs. As we stated in the final rule for FY 2004 that first issued the market basket forecast error adjustment (68 FR 46058), the adjustment will reflect both upward and downward adjustments, as appropriate.
For FY 2020 (the most recently available FY for which there is final data), the forecasted or estimated increase in the SNF market basket index was 2.8 percent, and the actual increase for FY 2020 is 2.0 percent, resulting in the actual increase being 0.8 percentage point lower than the estimated increase. Accordingly, as the difference between the estimated and actual amount of change in the market basket index exceeds the 0.5 percentage point threshold, under the policy previously described (comparing the forecasted and actual increase in the market basket), the FY 2022 market basket percentage change of 2.7 percent, based on the IGI second quarter 2021 forecast, would be adjusted downward to account for the forecast error correction of 0.8 percentage point, resulting in a SNF market basket percentage change of 1.2 percent after reducing the market basket update by the productivity adjustment of 0.7 percentage point, discussed below.
In the FY 2022 SNF PPS proposed rule, we noted that we may consider modifying this forecast error methodology in future rulemaking. We invited comments and feedback on this issue, in particular on the possibility of, in future rulemaking, either eliminating the forecast error adjustment, or raising the threshold for the forecast error from 0.5 percent to 1.0 percent.
Table 2 shows the forecasted and actual market basket increases for FY 2020.
Start Printed Page 42429

The following is a summary of the public comments received on the potential revisions to the forecast error adjustment and our responses:
Comment: Several commenters provided feedback on potentially modifying the SNF forecast error threshold in future rulemaking. Some commenters requested that the forecast error threshold remain the same at 0.5 percentage point. Other commenters requested that the forecast error threshold be increased to 1.0 percentage point in order to provide greater stability and certainty for year-to-year payments, while others requested that it be eliminated. One commenter recommended retaining the forecast error adjustment for the next three fiscal years at 0.5 percentage point and to then move to an alternative approach that would use a cumulative rolling projected forecast error calculation before triggering the forecast error threshold.
Response: We appreciate the commenters' responses and viewpoints on the forecast error threshold and will take them into consideration for future rulemaking.
Comment: Some commenters further stated that while they generally support the forecast error concept for the SNF PPS, given the scale of the COVID-19 disruption that occurred in FY 2020 and the associated atypical claims, they have concerns about the reliability and timing of the proposed 0.8 percentage point forecast error adjustment. Commenters stated that they believe CMS did not provide transparency in what is driving the variance between the estimated and actual 2020 market basket update and, therefore, they did not have an opportunity to comment on the data used to explain the variance. They stated that the industry experience in 2020 was that labor costs in particular were much higher than expected. A few commenters specifically requested that CMS eliminate the forecast error adjustment for FY 2022.
Response: The PHE presented many challenges to SNFs and as more complete data covering the full impact of the PHE become available we plan to monitor the information as it pertains to future rate updates and forecast error adjustments.
Pertaining to the forecast error, CMS publishes the forecasts of the market baskets (including SNF) on the CMS website (https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MedicareProgramRatesStats/MarketBasketData) on a quarterly basis. Additionally, as stated on the CMS website, providers can also email DNHS@cms.hhs.gov for further information on the market baskets. For the FY 2020 SNF market basket forecast error, this quarterly information was indicating that the error was likely to exceed the threshold of 0.5 percentage point. The final FY 2020 forecast error was only recently able to be computed using historical data through the third quarter of 2020, and this information was provided in the proposed rule. In response to commenters, we are providing a detailed breakdown of the contribution of the major market basket categories to the 0.8-percentage point forecast error: 0.4 percentage point is due to lower compensation price growth, 0.2 percentage point is due to lower Fuel, Oil, and Gas prices, and 0.2 percentage point is due to lower pharmaceutical prices. As stated in section VI.A. of this final rule, the SNF market basket is a Laspeyres-type price index that measures the prices associated with providing skilled nursing care services to Medicare beneficiaries. Cost growth is a function of price (such as the growth in average hourly wages) and quantity (such as increases in labor hours). Any changes in the quantity or mix of goods and services (that is, intensity) purchased over time relative to a base period are not measured annually, these are reflected when the market basket is rebased (such as our proposal to rebase the SNF market basket to 2018). Commenters interested in the detailed 2014-based SNF market basket methodology and its underlying public data sources may refer to the FY 2018 SNF PPS final rule (82 FR 36548 through 36565).
After consideration of the comments discussed above, we are finalizing the application of the proposed forecast error adjustment without modification. As stated above, based on IGI's second quarter 2021 forecast with historical data through the first quarter of 2021, the updated FY 2022 growth rate of the 2018-based SNF market basket is estimated to be 2.7 percent. Applying the forecast error adjustment for FY 2022 results in an adjusted FY 2022 market basket update factor of 1.9 percent, which is then further reduced by the productivity adjustment discussed below.
4. Productivity Adjustment
Section 1888(e)(5)(B)(ii) of the Act, as added by section 3401(b) of the Patient Protection and Affordable Care Act (Affordable Care Act) (Pub. L. 111-148, enacted March 23, 2010) requires that, in FY 2012 and in subsequent FYs, the market basket percentage under the SNF payment system (as described in section 1888(e)(5)(B)(i) of the Act) is to be reduced annually by the productivity adjustment described in section 1886(b)(3)(B)(xi)(II) of the Act. Section 1886(b)(3)(B)(xi)(II) of the Act, in turn, defines the productivity adjustment to be equal to the 10-year moving average of changes in annual economy-wide, private nonfarm business multifactor productivity (MFP) (as projected by the Secretary for the 10-year period ending with the applicable FY, year, cost-reporting period, or other annual period). The U.S. Department of Labor's Bureau of Labor Statistics (BLS) publishes the official measure of private nonfarm business MFP. We refer readers to the BLS website at http://www.bls.gov/mfp for the BLS historical published MFP data.
A complete description of the MFP projection methodology is available on our website at http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MedicareProgramRatesStats/MarketBasketResearch.html. We note that, effective with FY 2022 and forward, we are changing the name of this adjustment to refer to it as the Start Printed Page 42430 "productivity adjustment," rather than the "MFP adjustment." This change in terminology results in a title more consistent with the statutory language described in section 1886(b)(3)(B)(xi)(II) of the Act.
a. Incorporating the Productivity Adjustment Into the Market Basket Update
Per section 1888(e)(5)(A) of the Act, the Secretary shall establish a SNF market basket index that reflects changes over time in the prices of an appropriate mix of goods and services included in covered SNF services. Section 1888(e)(5)(B)(ii) of the Act, added by section 3401(b) of the Affordable Care Act, requires that for FY 2012 and each subsequent FY, after determining the market basket percentage described in section 1888(e)(5)(B)(i) of the Act, the Secretary shall reduce such percentage by the productivity adjustment described in section 1886(b)(3)(B)(xi)(II) of the Act. Section 1888(e)(5)(B)(ii) of the Act further states that the reduction of the market basket percentage by the productivity adjustment may result in the market basket percentage being less than zero for a FY, and may result in payment rates under section 1888(e) of the Act being less than such payment rates for the preceding fiscal year. Thus, if the application of the productivity adjustment to the market basket percentage calculated under section 1888(e)(5)(B)(i) of the Act results in a productivity-adjusted market basket percentage that is less than zero, then the annual update to the unadjusted Federal per diem rates under section 1888(e)(4)(E)(ii) of the Act would be negative, and such rates would decrease relative to the prior FY.
Based on the data available for the FY 2022 SNF PPS proposed rule, the estimated 10-year moving average of changes in MFP for the period ending September 30, 2022 was 0.2 percentage point. However, for this final rule, based on IGI's second quarter 2021 forecast, the estimated 10-year moving average of changes in MFP for the period ending September 30, 2022 is 0.7 percentage point.
Consistent with section 1888(e)(5)(B)(i) of the Act and § 413.337(d)(2), as discussed previously, the market basket percentage for FY 2022 for the SNF PPS is based on IGI's second quarter 2021 forecast of the SNF market basket percentage, which is estimated to be 2.7 percent. This market basket percentage is then lowered by 0.8 percentage point, due to application of the forecast error adjustment discussed above. Finally, as discussed above, we are applying a 0.7 percentage point productivity adjustment to the FY 2022 SNF market basket percentage. The resulting productivity-adjusted FY 2022 SNF market basket update is, therefore, equal to 1.2 percent, or 2.7 percent less 0.8 percentage point to account for forecast error and less 0.7 percentage point to account for the productivity adjustment.
5. Market Basket Update Factor for FY 2022
Sections 1888(e)(4)(E)(ii)(IV) and (e)(5)(i) of the Act require that the update factor used to establish the FY 2022 unadjusted Federal rates be at a level equal to the market basket index percentage change. Accordingly, we determined the total growth from the average market basket level for the period of October 1, 2020 through September 30, 2021 to the average market basket level for the period of October 1, 2021 through September 30, 2022. This process yields a percentage change in the 2018-based SNF market basket of 2.7 percent.
As further explained in section IV.B.2.c. of this final rule, as applicable, we adjust the market basket percentage change by the forecast error from the most recently available FY for which there is final data and apply this adjustment whenever the difference between the forecasted and actual percentage change in the market basket exceeds a 0.5 percentage point threshold in absolute terms. Since the forecasted FY 2020 SNF market basket percentage change exceeded the actual FY 2020 SNF market basket percentage change (FY 2020 is the most recently available FY for which there is historical data) by more than the 0.5 percentage point threshold, we proposed to adjust the FY 2022 market basket percentage change downward by the forecast error correction. Applying the −0.8 percentage point forecast error correction results in an adjusted FY 2022 SNF market basket percentage change of 1.9 percent (2.7 percent market basket update less 0.8 percentage point forecast error adjustment).
Section 1888(e)(5)(B)(ii) of the Act requires us to reduce the market basket percentage change by the productivity adjustment (10-year moving average of changes in MFP for the period ending September 30, 2022) which is estimated to be 0.7 percentage point, as described in section IV.B.2.d. of this final rule. Thus, we apply a net SNF market basket update factor of 1.2 percent in our determination of the FY 2022 SNF PPS unadjusted Federal per diem rates, which reflects a market basket increase factor of 2.7 percent, less the 0.8 percent forecast error correction and less the 0.7 percentage point productivity adjustment.
In the proposed rule, we noted that if more recent data become available (for example, a more recent estimate of the SNF market basket and/or MFP), we would use such data, if appropriate, to determine the FY 2022 SNF market basket percentage change, labor-related share relative importance, forecast error adjustment, or productivity adjustment in the FY 2022 SNF PPS final rule. Since more recent data did become available since the proposed rule, as outlined above, we have updated the various adjustment factors described through this section accordingly.
We also noted that section 1888(e)(6)(A)(i) of the Act provides that, beginning with FY 2018, SNFs that fail to submit data, as applicable, in accordance with sections 1888(e)(6)(B)(i)(II) and (III) of the Act for a fiscal year will receive a 2.0 percentage point reduction to their market basket update for the fiscal year involved, after application of section 1888(e)(5)(B)(ii) of the Act (the productivity adjustment) and section 1888(e)(5)(B)(iii) of the Act (the 1 percent market basket increase for FY 2018). In addition, section 1888(e)(6)(A)(ii) of the Act states that application of the 2.0 percentage point reduction (after application of section 1888(e)(5)(B)(ii) and (iii) of the Act) may result in the market basket index percentage change being less than zero for a fiscal year, and may result in payment rates for a fiscal year being less than such payment rates for the preceding fiscal year. Section 1888(e)(6)(A)(iii) of the Act further specifies that the 2.0 percentage point reduction is applied in a noncumulative manner, so that any reduction made under section 1888(e)(6)(A)(i) of the Act applies only to the fiscal year involved, and that the reduction cannot be taken into account in computing the payment amount for a subsequent fiscal year.
6. Unadjusted Federal Per Diem Rates for FY 2022
As discussed in the FY 2019 SNF PPS final rule (83 FR 39162), in FY 2020 we implemented a new case-mix classification system to classify SNF patients under the SNF PPS, the PDPM. As discussed in section V.B.1. of that final rule (83 FR 39189), under PDPM, the unadjusted Federal per diem rates are divided into six components, five of which are case-mix adjusted components (Physical Therapy (PT), Occupational Therapy (OT), Speech-Language Pathology (SLP), Nursing, and Non-Therapy Ancillaries (NTA)), and Start Printed Page 42431 one of which is a non-case-mix component, as existed under the previous RUG-IV model. We proposed to use the SNF market basket, adjusted as described previously, to adjust each per diem component of the Federal rates forward to reflect the change in the average prices for FY 2022 from the average prices for FY 2021. We proposed to further adjust the rates by a wage index budget neutrality factor, described later in this section. Further, in the past, we used the revised OMB delineations adopted in the FY 2015 SNF PPS final rule (79 FR 45632, 45634), with updates as reflected in OMB Bulletin Nos. 15-01 and 17-01, to identify a facility's urban or rural status for the purpose of determining which set of rate tables would apply to the facility. As discussed in the FY 2021 SNF PPS proposed and final rules, we adopted the revised OMB delineations identified in OMB Bulletin No. 18-04 (available at https://www.whitehouse.gov/wp-content/uploads/2018/09/Bulletin-18-04.pdf) to identify a facility's urban or rural status effective beginning with FY 2021.
For FY 2022, we note there is an additional adjustment to the unadjusted per diem base rates. Specifically, section 134 in Division CC of the Consolidated Appropriations Act, 2021 included a provision amending section 1888(e)(2)(A)(iii) of the Act so as to add "blood clotting factors indicated for the treatment of patients with hemophilia and other bleeding disorders . . . and items and services related to the furnishing of such factors under section 1842(o)(5)(C)" to the list of items and services excludable from the Part A SNF PPS per diem payment, effective for items and services furnished on or after October 1, 2021. We discuss this provision further in section V.B. of this final rule.
Section 1888(e)(4)(G)(iii) of the Act further requires that the Secretary "provide for an appropriate proportional reduction in payments so that . . . the aggregate amount of such reductions is equal to the aggregate increase in payments attributable to the exclusion" of the services from the Part A PPS per diem rates under section 1888(e)(2)(A)(iii) of the Act.
In the FY 2001 rulemaking cycle (65 FR 19202 and 46792), we established a methodology for computing such offsets in response to similar targeted consolidated billing exclusions added to section 1888(e)(2)(A)(iii) Act by section 103 of BBRA 1999. This methodology resulted in a reduction of 5 cents ($0.05) in the unadjusted urban and rural rates, using the identical data as used to establish the Part B add-on for a sample of approximately 1,500 SNFs from the 1995 base period. However, because this methodology relied on data from 1995, we proposed a new methodology based on updated data (as discussed below) to apply the offsets required for the exclusion of the blood clotting factors and items and services related to the furnishing of such factors under section 1842(o)(5)(C) of the Act (referred to collectively as the blood clotting factor exclusion), as specified under the Consolidated Appropriations Act, 2021. As we noted in the proposed rule, we believe the use of the updated data will more accurately capture the actual cost of these factors, as using updated utilization data would reflect new types of blood clotting factors introduced in recent years and changes in utilization patterns of blood clotting factors since 1995.
The methodology for calculating the blood clotting factor exclusion offset as set forth in the proposed rule consists of five steps. In the first step, we begin with the total number of SNF utilization days for beneficiaries who have any amount of blood clotting factor (BCF) use in FY 2020. While we recognize the potential effects of the PHE for COVID-19 on SNF utilization during 2020, we believe we should use FY 2020 data because it is the most recent data available, and thus would best reflect the latest types of blood clotting factors and the most recent changes in utilization patterns; also, the FY 2020 data is the only data available that reflects utilization under the PDPM model rather than the RUG-IV model. However, in light of the potential impact of the PHE for COVID-19 on SNF utilization, particularly as it relates to those patients admitted with COVID-19 or whose stays utilized a PHE-related waiver (for example, the waiver which removes the requirement for a three-day prior inpatient hospital stay in order to receive SNF Part A coverage), we believe it is appropriate to use a subset of the full FY 2020 SNF population which excludes patients diagnosed with COVID-19 and those stays which utilized a PHE-related waiver. We discuss this concept in more detail in relation to the recalibration of the PDPM parity adjustment, discussed in section VI.C. of this final rule. As further explained below, we would note that using this subset population has very little impact on the result of the methodology described below. Throughout the discussion below, the term "SNF beneficiary" refers to beneficiaries in the FY 2020 subset population described above.
Since BCF use has historically been subject to SNF consolidated billing and its usage cannot be observed on billed SNF claims, this methodology resorts to claims from other settings to approximate BCF utilization in SNFs. Specifically, BCF use as well as items and services related to the furnishing of such factors under section 1842(o)(5)(C) of the Act are identified by checking if any of the Healthcare Common Procedure Coding System (HCPCS) codes listed in the Act, including J7170, J7175, J7177-J7183, J7185-J7190, J7192-J7195, J7198-J7203, J7205, and J7207-J7211, are recorded on outpatient claims, which are claims submitted by institutional outpatient providers (such as a hospital outpatient department), or carrier claims, which are fee-for-service claims submitted by professional practitioners, such as physicians, physician assistants, clinical social workers, and nurse practitioners, and by some organizational providers, such as free-standing facilities. A SNF beneficiary with any BCF use is defined as a SNF beneficiary with at least one matched outpatient or carrier claim for blood clotting factors in FY 2020. To calculate the number of SNF utilization days for beneficiaries who have any amount of BCF use in FY 2020, we sum up the corresponding SNF utilization days of SNF beneficiaries with BCF use in FY 2020 (84 beneficiaries), which is 3,317 total utilization days.
In the second step, we estimate the BCF payment per day per SNF beneficiary with any BCF use in FY 2020, which would include payment for the BCFs and items and services related to the furnishing of such factors under section 1842(o)(5)(C) of the Act. There are no direct payment data to track BCF use in SNFs since BCF use currently is bundled within the Part A per diem payment. Therefore, we rely on payment in outpatient and carrier claims as a proxy for this step. Instead of calculating BCF payment per day for SNF beneficiaries in a SNF stay, we estimate the BCF payment per day for SNF beneficiaries outside of their SNF and inpatient stays, under the assumption that BCF payment per day for SNF beneficiaries is similar during and outside of SNF stays. Outpatient or carrier claims for BCF use that overlap with a SNF stay or an inpatient stay of a SNF beneficiary are excluded to ensure that BCF-related payment is fully captured in Part B claims instead of partially paid through Part A. Overlapping claims are identified when the outpatient claim "From" date or the carrier claim expense date fall within a SNF or inpatient stay's admission and discharge date window. The total BCF payment for SNF beneficiaries' BCF use Start Printed Page 42432 observed through Part B claims in FY 2020 was $4,843,551. Next, to determine the corresponding utilizations days for SNF beneficiaries' BCF use, we need to carve out their utilization days in a SNF or inpatient setting for these target beneficiaries. We first determine the total SNF and inpatient utilization days for these beneficiaries in FY 2020, which totals 5,408. Next, we determine the total days that the beneficiaries with BCF use were not in a SNF or inpatient stay, which is 365 (for days in the year) multiplied by the number of SNF beneficiaries with BCF use (84), less the total SNF and inpatient utilization days for these beneficiaries (5,408), which is 20,142. Finally, we estimated the BCF payment per day, which is the total BCF payment observed in outpatient and carrier claims ($4,843,551) divided by the total days the beneficiaries were not in a SNF or inpatient setting (20,142). Thus, we calculate the BCF payment per day per SNF beneficiary to be $240.
In the third step, we calculate the percentage of SNF payment associated with BCF usage. We multiply the estimated BCF payment per day ($240 as determined in step 2) by the total SNF utilization days for SNF beneficiaries with BCF use in FY 2020 (3,317 as determined in step 1). This yields an estimated BCF payment for SNF beneficiaries in the study population of $797,640. Next, we divide this by the total SNF payment for the study population during FY 2020 ($22,636,345,868) to yield the percentage of SNF payment associated with BCF use, which we estimate to be 0.00352 percent.
In the fourth step, we calculate the urban and rural base rate reductions, by multiplying the proposed FY 2022 urban/rural base rates by the percentage of SNF payment associated with clotting factor use determined in step 3 (0.00352 percent). In the case of the proposed urban base rate of $434.95, this yields an urban base rate deduction of $0.02, which we would apply as a $0.01 reduction to the proposed FY 2022 NTA base rate and a $0.01 reduction to the proposed FY 2022 nursing base rate. In the case of the proposed rural base rate of $450.37, this yields a rural base rate deduction of $0.02, which we would apply as a $0.01 reduction to the proposed FY 2022 NTA base rates and a $0.01 reduction to the proposed FY 2022 nursing base rate. We would apply the reduction to the NTA and nursing base rates because BCF is a type of NTA and nursing resources are required to furnish this medication.
In step five, for purposes of impact analysis, we calculate the budget impact of the base rate reductions to be $782,785. We estimate the budget impact by multiplying the total FY2022 SNF baseline ($34,211,000,000) by the percentage of SNF payment for clotting factor (0.00352 percent). This results in a total reduction in SNF spending of $1.2 million. To compare the result of this methodology to that which would have resulted from using the full FY 2020 SNF population, we note that if we had used the full FY 2020 SNF population, the resultant impact would be a reduction in SNF spending of $1.5 million, which represents 0.004551 percent of total payments made under the SNF PPS. Given that these figures are so close as to result in the same two cent reduction in the FY 2022 SNF PPS unadjusted per diem rates, and given the reasons for using the subset population discussed in section VI.C. of this final rule, we believe it is appropriate to use this subset population as the basis for the calculations described throughout this section.
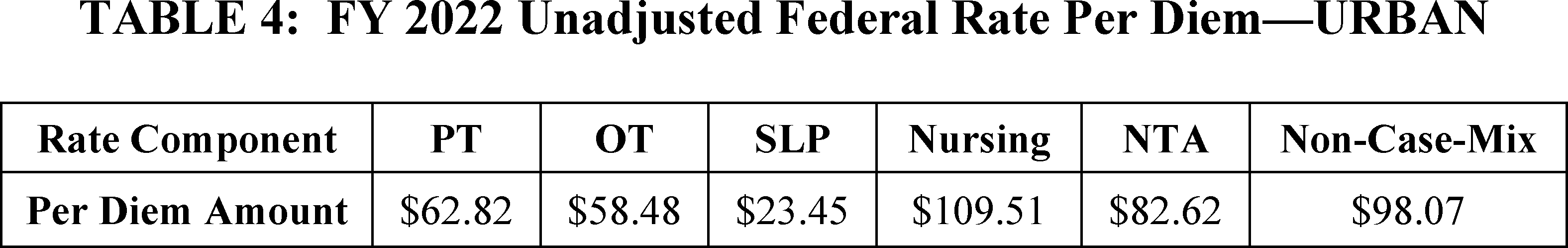
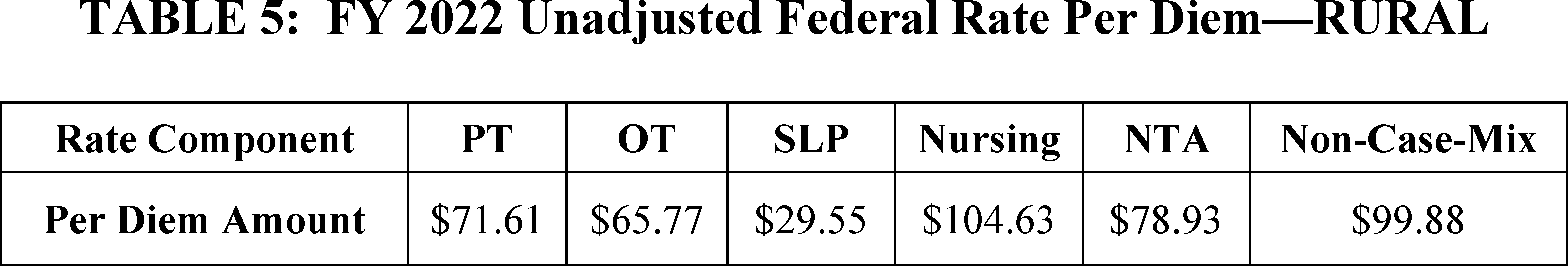
We apply these rate reductions to the NTA and nursing components of the unadjusted Federal urban and rural per diem rate as shown in Tables 4 and 5.
Table 3 displays the methodology and figures used to calculate these rate reductions.
Start Printed Page 42433

The comments we received on the proposed methodology to adjust the SNF PPS base rates in response to the recent blood clotting factor exclusion, along with our responses, appear below.
Comment: Several commenters noted support for the proposed methodology for adjusting the base rates to remove the costs associated with Blood Clotting Factor (BCF)-related services from the Part A consolidated billing per diem payment that resulted in a proposed 0.00352 percent adjustment. A commenter noted that this methodology is preferable to the alternative methodology that would result in a 0.004551 percent adjustment.
Response: We thank the commenters for their support. Accordingly, we are finalizing, as proposed, the methodology for reducing the base rates to remove the costs associated with Blood Clotting Factor (BCF)-related services.
Tables 4 and 5 reflect the updated unadjusted Federal rates for FY 2022, prior to adjustment for case-mix. The rates in Tables 4 and 5 include the reductions calculated in Table 3 for blood clotting factor use.
Start Printed Page 42434
C. Case-Mix Adjustment
Under section 1888(e)(4)(G)(i) of the Act, the Federal rate also incorporates an adjustment to account for facility case-mix, using a classification system that accounts for the relative resource utilization of different patient types. The statute specifies that the adjustment is to reflect both a resident classification system that the Secretary establishes to account for the relative resource use of different patient types, as well as resident assessment data and other data that the Secretary considers appropriate. In the FY 2019 final rule (83 FR 39162, August 8, 2018), we finalized a new case-mix classification model, the PDPM, which took effect beginning October 1, 2019. The previous RUG-IV model classified most patients into a therapy payment group and primarily used the volume of therapy services provided to the patient as the basis for payment classification, thus creating an incentive for SNFs to furnish therapy regardless of the individual patient's unique characteristics, goals, or needs. PDPM eliminates this incentive and improves the overall accuracy and appropriateness of SNF payments by classifying patients into payment groups based on specific, data-driven patient characteristics, while simultaneously reducing the administrative burden on SNFs.
As we noted in the FY 2021 SNF PPS final rule (85 FR 47600), we continue to monitor the impact of PDPM implementation on patient outcomes and program outlays. We hope to release information in the future that relates to these issues, though we provide some of this information in section VI.C. of this final rule. We also continue to monitor the impact of PDPM implementation as it relates to our intention to ensure that PDPM is implemented in a budget neutral manner, as discussed in the FY 2020 SNF PPS final rule (84 FR 38734). In section VI.C. of this final rule, we discuss the methodology to recalibrate the PDPM parity adjustment as appropriate to ensure budget neutrality, as we did after the implementation of RUG-IV in FY 2011.
The PDPM uses clinical data from the MDS to assign case-mix classifiers to each patient that are then used to calculate a per diem payment under the SNF PPS, consistent with the provisions of section 1888(e)(4)(G)(i) of the Act. As discussed in section V.A. of this final rule, the clinical orientation of the case-mix classification system supports the SNF PPS's use of an administrative presumption that considers a beneficiary's initial case-mix classification to assist in making certain SNF level of care determinations. Further, because the MDS is used as a basis for payment, as well as a clinical assessment, we have provided extensive training on proper coding and the timeframes for MDS completion in our Resident Assessment Instrument (RAI) Manual. As we have stated in prior rules, for an MDS to be considered valid for use in determining payment, the MDS assessment should be completed in compliance with the instructions in the RAI Manual in effect at the time the assessment is completed. For payment and quality monitoring purposes, the RAI Manual consists of both the Manual instructions and the interpretive guidance and policy clarifications posted on the appropriate MDS website at http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/MDS30RAIManual.html.
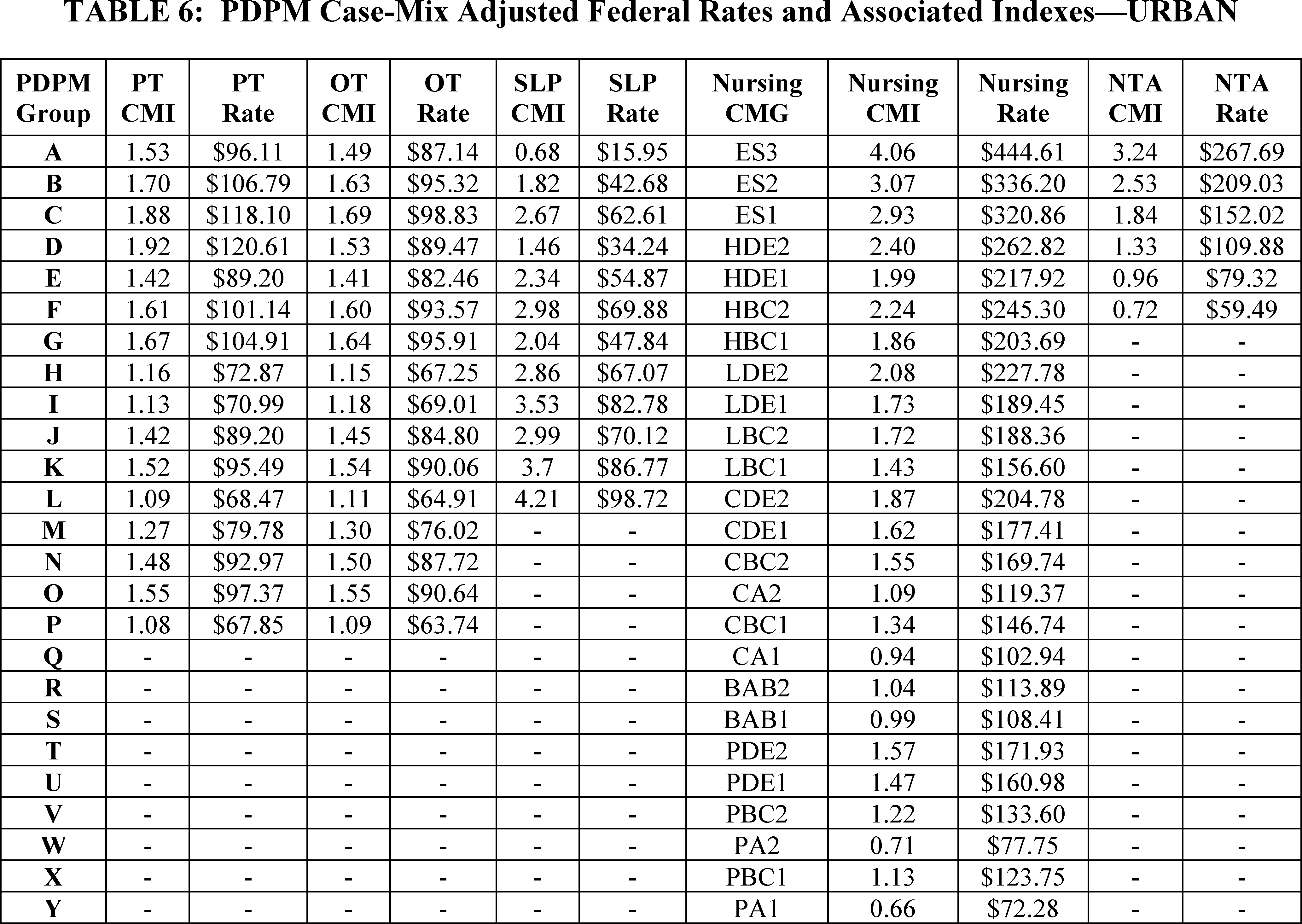
Under section 1888(e)(4)(H) of the Act, each update of the payment rates must include the case-mix classification methodology applicable for the upcoming FY. The FY 2022 payment rates set forth in this final rule reflect the use of the PDPM case-mix classification system from October 1, 2021, through September 30, 2022. The case-mix adjusted PDPM payment rates for FY 2022 are listed separately for urban and rural SNFs, in Tables 6 and 7 with corresponding case-mix values.
Given the differences between the previous RUG-IV model and PDPM in terms of patient classification and billing, it was important that the format of Tables 6 and 7 reflect these differences. More specifically, under both RUG-IV and PDPM, providers use a Health Insurance Prospective Payment System (HIPPS) code on a claim to bill for covered SNF services. Under RUG-IV, the HIPPS code included the three-character RUG-IV group into which the patient classified as well as a two-character assessment indicator code that represented the assessment used to generate this code. Under PDPM, while providers still use a HIPPS code, the characters in that code represent different things. For example, the first character represents the PT and OT group into which the patient classifies. If the patient is classified into the PT and OT group "TA", then the first character in the patient's HIPPS code would be an A. Similarly, if the patient is classified into the SLP group "SB", then the second character in the patient's HIPPS code would be a B. The third character represents the Nursing group into which the patient classifies. The fourth character represents the NTA group into which the patient classifies. Finally, the fifth character represents the assessment used to generate the HIPPS code.
Tables 6 and 7 reflect the PDPM's structure. Accordingly, Column 1 of Tables 6 and 7 represents the character in the HIPPS code associated with a given PDPM component. Columns 2 and 3 provide the case-mix index and associated case-mix adjusted component rate, respectively, for the relevant PT group. Columns 4 and 5 provide the case-mix index and associated case-mix adjusted component rate, respectively, for the relevant OT group. Columns 6 and 7 provide the case-mix index and associated case-mix adjusted component rate, respectively, for the relevant SLP group. Column 8 provides the nursing case-mix group (CMG) that is connected with a given PDPM HIPPS character. For example, if the patient qualified for the nursing group CBC1, then the third character in the patient's HIPPS code would be a "P." Columns 9 and 10 provide the case-mix index and associated case-mix adjusted component rate, respectively, for the relevant nursing group. Finally, columns 11 and 12 provide the case-mix index and associated case-mix adjusted component rate, respectively, for the relevant NTA group.
Tables 6 and 7 do not reflect adjustments which may be made to the SNF PPS rates as a result of the SNF VBP Program, discussed in section IV.D. of this final rule, or other adjustments, such as the variable per diem adjustment. Further, in the past, we used the revised OMB delineations adopted in the FY 2015 SNF PPS final rule (79 FR 45632, 45634), with updates as reflected in OMB Bulletin Nos, 15-01 and 17-01, to identify a facility's urban or rural status for the purpose of determining which set of rate tables would apply to the facility. As discussed in the FY 2021 SNF PPS final rule (85 FR 47594), we adopted the revised OMB delineations identified in OMB Bulletin No. 18-04 (available at https://www.whitehouse.gov/wp-content/uploads/2018/09/Bulletin-18-04.pdf) to identify a facility's urban or rural status effective beginning with FY 2021.
Start Printed Page 42435
Start Printed Page 42436

D. Wage Index Adjustment
Section 1888(e)(4)(G)(ii) of the Act requires that we adjust the Federal rates to account for differences in area wage levels, using a wage index that the Secretary determines appropriate. Since the inception of the SNF PPS, we have used hospital inpatient wage data in developing a wage index to be applied to SNFs. We continue this practice for FY 2022, as we continue to believe that in the absence of SNF-specific wage data, using the hospital inpatient wage index data is appropriate and reasonable for the SNF PPS. As explained in the update notice for FY 2005 (69 FR 45786), the SNF PPS does not use the hospital area wage index's occupational mix adjustment, as this adjustment serves specifically to define the occupational categories more clearly in a hospital setting; moreover, the collection of the occupational wage data under the inpatient prospective payment system (IPPS) also excludes any wage data related to SNFs. Therefore, we believe that using the updated wage data exclusive of the occupational mix adjustment continues to be appropriate for SNF payments. As in previous years, we would continue to use the pre-reclassified IPPS hospital wage data, without applying the occupational mix, rural floor, or outmigration adjustment, as the basis for the SNF PPS wage index. For FY 2022, the updated wage data are for hospital cost reporting periods beginning on or after October 1, 2017 and before October 1, 2018 (FY 2018 cost report data).
We note that section 315 of the Medicare, Medicaid, and SCHIP Benefits Improvement and Protection Act of 2000 (BIPA) (Pub. L. 106-554, enacted December 21, 2000) authorized us to establish a geographic reclassification procedure that is specific to SNFs, but only after collecting the data necessary to establish a SNF PPS wage index that is based on wage data from nursing homes. However, to date, this has proven to be unfeasible due to the volatility of existing SNF wage data and the significant amount of resources that would be required to improve the quality of the data. More specifically, auditing all SNF cost reports, similar to the process used to audit inpatient hospital cost reports for purposes of the IPPS wage index, would place a burden on providers in terms of recordkeeping and completion of the cost report worksheet. In addition, adopting such an approach would require a significant commitment of resources by CMS and the Medicare Administrative Contractors, potentially far in excess of those required under the IPPS given that there are nearly five times as many SNFs as there are inpatient hospitals. Therefore, while we continue to believe that the development of such an audit process could improve SNF cost reports in such a manner as to permit us to establish a SNF-specific wage index, we do not believe this undertaking is feasible at this time.
In the proposed rule, we proposed to continue using the same methodology discussed in the SNF PPS final rule for FY 2008 (72 FR 43423) to address those geographic areas in which there are no hospitals, and thus, no hospital wage index data on which to base the calculation of the FY 2022 SNF PPS wage index. For rural geographic areas that do not have hospitals and, therefore, lack hospital wage data on which to base an area wage adjustment, we proposed to continue using the average wage index from all contiguous Start Printed Page 42437 Core-Based Statistical Areas (CBSAs) as a reasonable proxy. For FY 2022, there are no rural geographic areas that do not have hospitals, and thus, this methodology will not be applied. For rural Puerto Rico, we proposed not to apply this methodology due to the distinct economic circumstances that exist there (for example, due to the close proximity to one another of almost all of Puerto Rico's various urban and non-urban areas, this methodology would produce a wage index for rural Puerto Rico that is higher than that in half of its urban areas); instead, we would continue using the most recent wage index previously available for that area. For urban areas without specific hospital wage index data, we proposed that we would use the average wage indexes of all of the urban areas within the state to serve as a reasonable proxy for the wage index of that urban CBSA. For FY 2022, the only urban area without wage index data available is CBSA 25980, Hinesville-Fort Stewart, GA.
The wage index applicable to FY 2022 is set forth in Tables A and B available on the CMS website at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/SNFPPS/WageIndex.html.
In the SNF PPS final rule for FY 2006 (70 FR 45026, August 4, 2005), we adopted the changes discussed in OMB Bulletin No. 03-04 (June 6, 2003), which announced revised definitions for MSAs and the creation of micropolitan statistical areas and combined statistical areas. In adopting the CBSA geographic designations, we provided for a 1-year transition in FY 2006 with a blended wage index for all providers. For FY 2006, the wage index for each provider consisted of a blend of 50 percent of the FY 2006 MSA-based wage index and 50 percent of the FY 2006 CBSA-based wage index (both using FY 2002 hospital data). We referred to the blended wage index as the FY 2006 SNF PPS transition wage index. As discussed in the SNF PPS final rule for FY 2006 (70 FR 45041), after the expiration of this 1-year transition on September 30, 2006, we used the full CBSA-based wage index values.
In the FY 2015 SNF PPS final rule (79 FR 45644 through 45646), we finalized changes to the SNF PPS wage index based on the newest OMB delineations, as described in OMB Bulletin No. 13-01, beginning in FY 2015, including a1-year transition with a blended wage index for FY 2015. OMB Bulletin No. 13-01 established revised delineations for Metropolitan Statistical Areas, Micropolitan Statistical Areas, and Combined Statistical Areas in the United States and Puerto Rico based on the 2010 Census, and provided guidance on the use of the delineations of these statistical areas using standards published in the June 28, 2010 Federal Register (75 FR 37246 through 37252). Subsequently, on July 15, 2015, OMB issued OMB Bulletin No. 15-01, which provided minor updates to and superseded OMB Bulletin No. 13-01 that was issued on February 28, 2013. The attachment to OMB Bulletin No. 15-01 provided detailed information on the update to statistical areas since February 28, 2013. The updates provided in OMB Bulletin No. 15-01 were based on the application of the 2010 Standards for Delineating Metropolitan and Micropolitan Statistical Areas to Census Bureau population estimates for July 1, 2012 and July 1, 2013 and were adopted under the SNF PPS in the FY 2017 SNF PPS final rule (81 FR 51983, August 5, 2016). In addition, on August 15, 2017, OMB issued Bulletin No. 17-01 which announced a new urban CBSA, Twin Falls, Idaho (CBSA 46300) which was adopted in the SNF PPS final rule for FY 2019 (83 FR 39173, August 8, 2018).
As discussed in the FY 2021 SNF PPS final rule (85 FR 47594), we adopted the revised OMB delineations identified in OMB Bulletin No. 18-04 (available at https://www.whitehouse.gov/wp-content/uploads/2018/09/Bulletin-18-04.pdf) beginning October 1, 2020, including a 1-year transition for FY 2021 under which we applied a 5 percent cap on any decrease in a hospital's wage index compared to its wage index for the prior fiscal year (FY 2020). The updated OMB delineations more accurately reflect the contemporary urban and rural nature of areas across the country, and the use of such delineations allows us to determine more accurately the appropriate wage index and rate tables to apply under the SNF PPS.
As we previously stated in the FY 2008 SNF PPS proposed and final rules (72 FR 25538 through 25539, and 72 FR 43423), this and all subsequent SNF PPS rules and notices are considered to incorporate any updates and revisions set forth in the most recent OMB bulletin that applies to the hospital wage data used to determine the current SNF PPS wage index. We note that on March 6, 2020, OMB issued Bulletin No. 20-01, which provided updates to and superseded OMB Bulletin No. 18-04 that was issued on September 14, 2018. The attachments to OMB Bulletin No. 20-01 provided detailed information on the updates (available on the web at https://www.whitehouse.gov/wp-content/uploads/2020/03/Bulletin-20-01.pdf). In the FY 2021 SNF PPS final rule (85 FR 47611), we stated that we intended to propose any updates from OMB Bulletin No. 20-01 in the FY 2022 SNF PPS proposed rule. After reviewing OMB Bulletin No. 20-01, we have determined that the changes in OMB Bulletin 20-01 encompassed delineation changes that do not impact the CBSA-based labor market area delineations adopted in FY 2021. Therefore, while we proposed to adopt the updates set forth in OMB Bulletin No. 20-01 consistent with our longstanding policy of adopting OMB delineation updates, we noted that specific wage index updates would not be necessary for FY 2022 as a result of adopting these OMB updates.
The proposed wage index applicable to FY 2022 is set forth in Tables A and B and is available on the CMS website at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/SNFPPS/WageIndex.html.
Once calculated, we would apply the wage index adjustment to the labor-related portion of the Federal rate. Each year, we calculate a revised labor-related share, based on the relative importance of labor-related cost categories (that is, those cost categories that are labor-intensive and vary with the local labor market) in the input price index. In the SNF PPS final rule for FY 2018 (82 FR 36548 through 36566), we finalized a proposal to revise the labor-related share to reflect the relative importance of the 2014-based SNF market basket cost weights for the following cost categories: Wages and Salaries; Employee Benefits; Professional Fees: Labor-Related; Administrative and Facilities Support Services; Installation, Maintenance, and Repair Services; All Other: Labor-Related Services; and a proportion of Capital-Related expenses. Effective beginning FY 2022, as discussed in section VI.A.4. of this final rule, for FY 2022, we are rebasing and revising the labor-related share to reflect the relative importance of the 2018-based SNF market basket cost weights for the following cost categories: Wages and Salaries; Employee Benefits; Professional fees: Labor-related; Administrative and Facilities Support services; Installation, Maintenance, and Repair services; All Other: Labor-Related Services; and a proportion of Capital-Related expenses. The methodology for calculating the labor-related portion for FY 2022 is discussed in section VI.A. of this final rule.
We calculate the labor-related relative importance from the SNF market basket, and it approximates the labor-related Start Printed Page 42438 portion of the total costs after taking into account historical and projected price changes between the base year and FY 2022. The price proxies that move the different cost categories in the market basket do not necessarily change at the same rate, and the relative importance captures these changes. Accordingly, the relative importance figure more closely reflects the cost share weights for FY 2022 than the base year weights from the SNF market basket. We calculate the labor-related relative importance for FY 2022 in four steps. First, we compute the FY 2022 price index level for the total market basket and each cost category of the market basket. Second, we calculate a ratio for each cost category by dividing the FY 2022 price index level for that cost category by the total market basket price index level. Third, we determine the FY 2022 relative importance for each cost category by multiplying this ratio by the base year (2018) weight. Finally, we add the FY 2022 relative importance for each of the labor-related cost categories (Wages and Salaries; Employee Benefits; Professional Fees: Labor-Related; Administrative and Facilities Support Services; Installation, Maintenance, and Repair Services; All Other: Labor-related services; and a portion of Capital-Related expenses) to produce the FY 2022 labor-related relative importance.
For the proposed rule, the labor-related share for FY 2022 was based on IGI's fourth quarter 2020 forecast of the proposed 2018-based SNF market basket with historical data through third quarter 2020. For this final rule, we based the labor-related share for FY 2022 on IGI's second quarter 2021 forecast, with historical data through the first quarter 2021. Table 8 summarizes the labor-related share for FY 2022, based on IGI's second quarter 2021 forecast of the 2018-based SNF market basket with historical data through first quarter 2021, compared to the labor-related share that was used for the FY 2021 SNF PPS final rule.
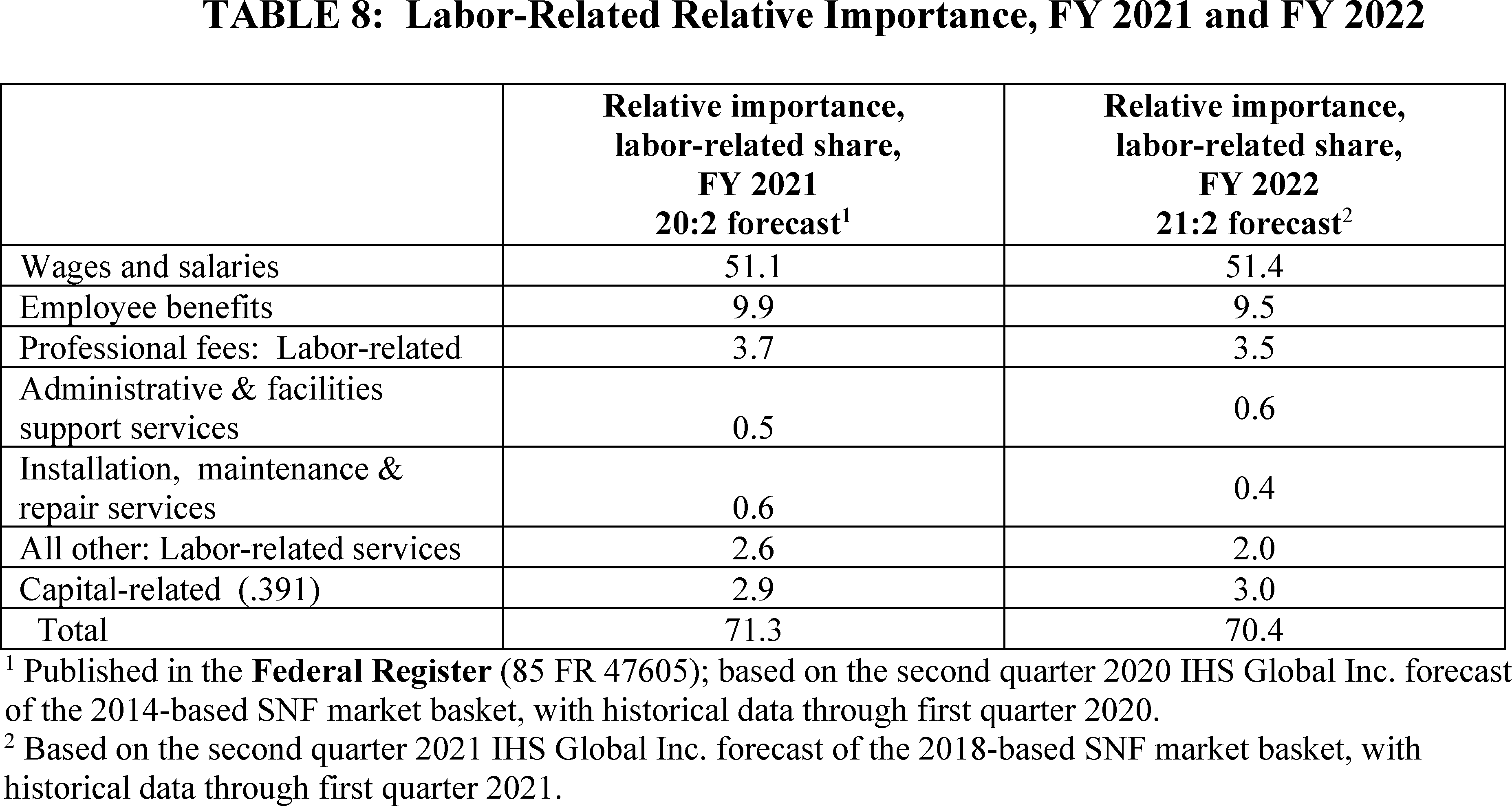
To calculate the labor portion of the case-mix adjusted per diem rate, we would multiply the total case-mix adjusted per diem rate, which is the sum of all five case-mix adjusted components into which a patient classifies, and the non-case-mix component rate, by the FY 2022 labor-related share percentage provided in Table 8. The remaining portion of the rate would be the non-labor portion. Under the previous RUG-IV model, we included tables which provided the case-mix adjusted RUG-IV rates, by RUG-IV group, broken out by total rate, labor portion and non-labor portion, such as Table 9 of the FY 2019 SNF PPS final rule (83 FR 39175). However, as we discussed in the FY 2020 final rule (84 FR 38738), under PDPM, as the total rate is calculated as a combination of six different component rates, five of which are case-mix adjusted, and given the sheer volume of possible combinations of these five case-mix adjusted components, it is not feasible to provide tables similar to those that existed in the prior rulemaking.
Therefore, to aid stakeholders in understanding the effect of the wage index on the calculation of the SNF per diem rate, we have included a hypothetical rate calculation in Table 9.
Section 1888(e)(4)(G)(ii) of the Act also requires that we apply this wage index in a manner that does not result in aggregate payments under the SNF PPS that are greater or less than would otherwise be made if the wage adjustment had not been made. For FY 2022 (Federal rates effective October 1, 2021), we apply an adjustment to fulfill the budget neutrality requirement. We meet this requirement by multiplying each of the components of the unadjusted Federal rates by a budget neutrality factor, equal to the ratio of the weighted average wage adjustment factor for FY 2021 to the weighted average wage adjustment factor for FY 2022. For this calculation, we would use the same FY 2020 claims utilization data for both the numerator and denominator of this ratio. We define the wage adjustment factor used in this calculation as the labor portion of the rate component multiplied by the wage index plus the non-labor portion of the rate component. The proposed budget neutrality factor for FY 2022 as set forth in the proposed rule was 0.9999.
In the proposed rule, we noted that if more recent data become available (for example, revised wage data), we would use such data, as appropriate, to determine the wage index budget neutrality factor in the SNF PPS final rule. Since the proposed rule, we have updated the weighted average wage Start Printed Page 42439 adjustment factor for FY 2022. Based on this updated information, the budget neutrality factor for FY 2022 is 1.0006.
The following is a summary of the public comments received on the proposed revisions to the Wage Index Adjustment and our responses:
Comment: Several commenters recommended that we consider creating a SNF-specific wage index utilizing the SNF cost report, as opposed to continuing to rely on hospital data as the basis for the SNF wage index. Commenters requested the SNF wage data analysis and access to needed hospital and SNF cost report wage data to conduct their own analysis towards assisting us in refining the current SNF wage index methodology. Additionally, one commenter requested to meet with CMS to discuss these ideas, while another commenter would like to provide more feedback.
Response: We appreciate the commenter's suggestion as to the development of a SNF specific wage index. However, to date, the development of a SNF-specific wage index has proven to be unfeasible due to the volatility of existing SNF wage data and the significant amount of resources that would be required to improve the quality of that data. We note that, consistent with the preceding discussion in this final rule as well as our previous responses to these recurring SNF-specific wage index comments (most recently published in the FY 2019 SNF PPS final rule (83 FR 39172 through 39173)), developing such a wage index would require a resource-intensive audit process similar to that used for IPPS hospital data, to improve the quality of the SNF cost report data in order for it to be used as part of this analysis. We also discussed in the FY 2019 SNF PPS why utilizing concepts such as trimming methods, BLS data, occupational mix, Payroll Based Journal, and rural floor are unfeasible or not applicable to SNF policy. We continue to believe that in the absence of the appropriate SNF-specific wage data, using the pre-reclassified, pre-rural floor hospital inpatient wage data (without the occupational mix adjustment) is appropriate and reasonable for the SNF PPS.
Regarding the request for data, we will consider the comments and examine what data could be released that would assist stakeholders in understanding both the volatility of the SNF wage data and the issues with using this data to develop a SNF-specific wage index. As always, we encourage and welcome dialogue with stakeholders regarding this, or any other, issues related to SNF payments under Medicare.
Comment: We received several comments that were outside the scope of the FY 2022 SNF PPS proposed rule. Specifically, commenters appreciated that, in the SNF PPS final rule for FY 2021, CMS recognized the need for a transitional policy in the form of a 5 percent cap on any decease in a SNF's wage index in adopting the OMB delineations updated in OMB Bulletin 18-04. However, these commenters also expressed that a 1-year cap is not sufficient to offset the enormous cuts scheduled for FY 2022, thus requesting an extension to the 5 percent cap transition.
Response: We thank the commenters for bringing this issue to our attention. We note that at times when changes to the wage index occur, those changes may result in large and potentially unpredictable impacts on Medicare payments that impact providers. These changes may arise from changes to wage index areas due to updates related to decennial census data, changes to wage index areas due to updates related to revised OMB delineations. While we consider how best to address these potential scenarios in a consistent and thoughtful manner, we reiterate that our policy principles with regard to the wage index are to use the most updated data and information available and provide that data and information, as well as any approaches to addressing these potential scenarios, through notice and comment rulemaking.
After considering the comments received, for the reasons set forth in this final rule and in the FY 2022 SNF PPS proposed rule, we are finalizing our proposal to adopt the revised OMB delineations contained in OMB Bulletin 18-04 as proposed, without modification.
E. SNF Value-Based Purchasing Program
Beginning with payment for services furnished on October 1, 2018, section 1888(h) of the Act requires the Secretary to reduce the adjusted Federal per diem rate determined under section 1888(e)(4)(G) of the Act otherwise applicable to a SNF for services furnished during a fiscal year by 2 percent, and to adjust the resulting rate for a SNF by the value-based incentive payment amount earned by the SNF based on the SNF's performance score for that fiscal year under the SNF VBP Program. To implement these requirements, we finalized in the FY 2019 SNF PPS final rule the addition of § 413.337(f) to our regulations (83 FR 39178).
Please see section VIII. of this final rule for a further discussion of our policies for the SNF VBP Program.
F. Adjusted Rate Computation Example
Tables 9, 10, and 11 provide examples generally illustrating payment calculations during FY 2022 under PDPM for a hypothetical 30-day SNF stay, involving the hypothetical SNF XYZ, located in Frederick, MD (Urban CBSA 23244), for a hypothetical patient who is classified into such groups that the patient's HIPPS code is NHNC1. Table 9 shows the adjustments made to the Federal per diem rates (prior to application of any adjustments under the SNF VBP Program as discussed previously) to compute the provider's case-mix adjusted per diem rate for FY 2022, based on the patient's PDPM classification, as well as how the variable per diem (VPD) adjustment factor affects calculation of the per diem rate for a given day of the stay. Table 10 shows the adjustments made to the case-mix adjusted per diem rate from Table 9 to account for the provider's wage index. The wage index used in this example is based on the FY 2022 SNF PPS wage index that appears in Table A available on the CMS website at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/SNFPPS/WageIndex.html. Finally, Table 11 provides the case-mix and wage index adjusted per-diem rate for this patient for each day of the 30-day stay, as well as the total payment for this stay. Table 11 also includes the VPD adjustment factors for each day of the patient's stay, to clarify why the patient's per diem rate changes for certain days of the stay. As illustrated in Table 9, SNF XYZ's total PPS payment for this particular patient's stay would equal $20,532.52.
Start Printed Page 42440

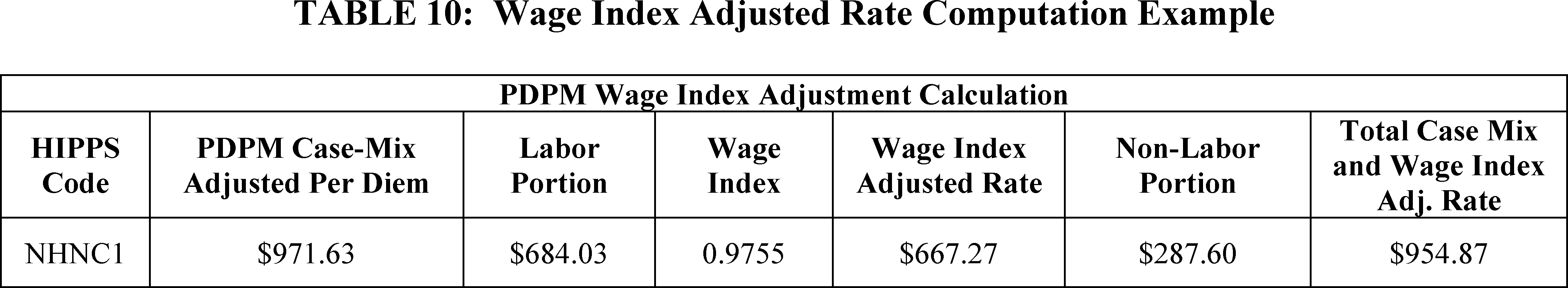
Start Printed Page 42441
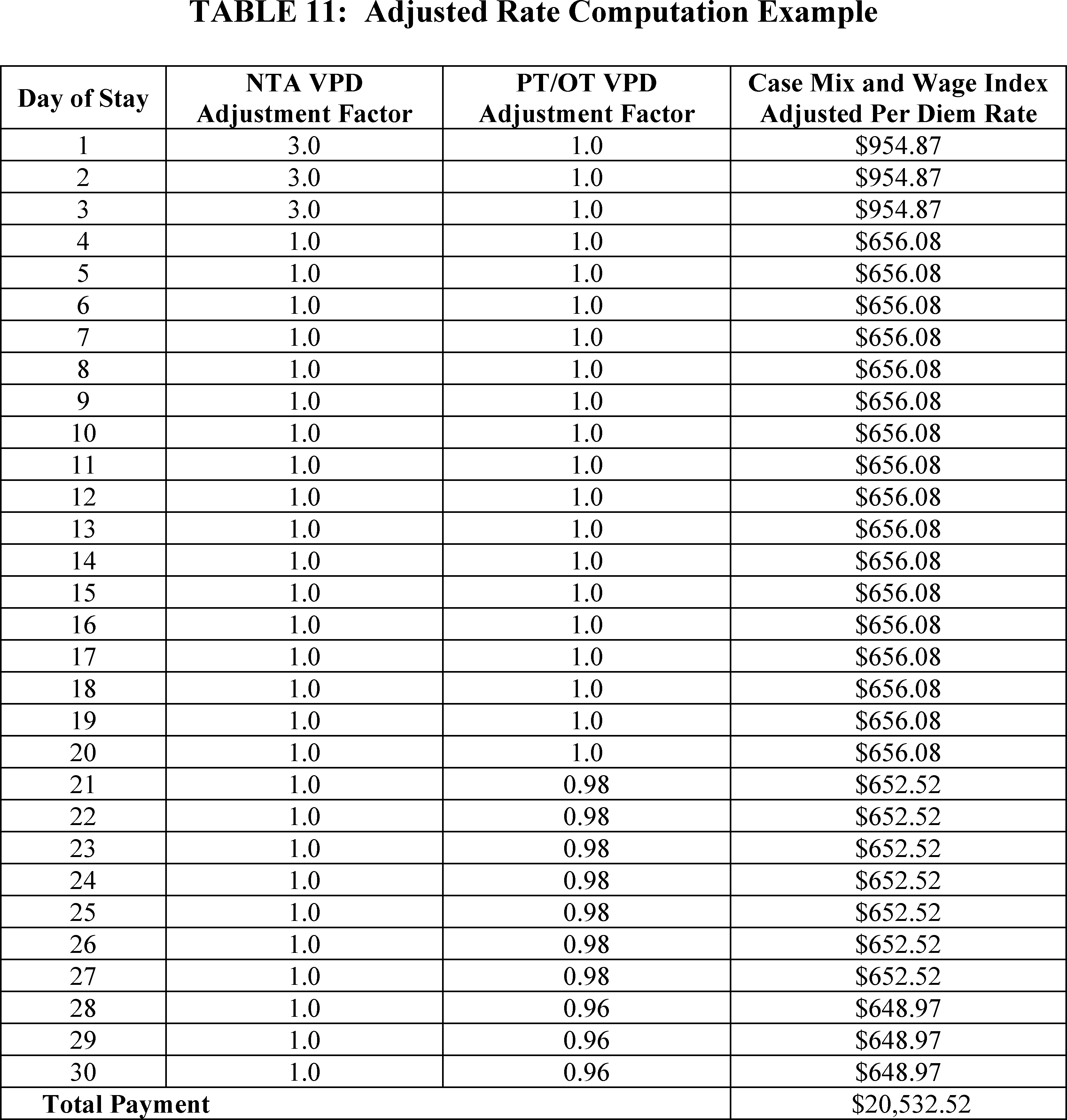
V. Additional Aspects of the SNF PPS
A. SNF Level of Care—Administrative Presumption
The establishment of the SNF PPS did not change Medicare's fundamental requirements for SNF coverage. However, because the case-mix classification is based, in part, on the beneficiary's need for skilled nursing care and therapy, we have attempted, where possible, to coordinate claims review procedures with the existing resident assessment process and case-mix classification system discussed in section IV.C. of this final rule. This approach includes an administrative presumption that utilizes a beneficiary's correct assignment, at the outset of the SNF stay, of one of the case-mix classifiers designated for this purpose to assist in making certain SNF level of care determinations.
In accordance with § 413.345, we include in each update of the Federal payment rates in the Federal Register a discussion of the resident classification system that provides the basis for case-mix adjustment. We also designate those specific classifiers under the case-mix classification system that represent the required SNF level of care, as provided in 42 CFR 409.30. This designation reflects an administrative presumption that those beneficiaries who are correctly assigned one of the designated case-mix classifiers on the initial Medicare assessment are automatically classified as meeting the SNF level of care definition up to and including the assessment reference date (ARD) for that assessment.
A beneficiary who does not qualify for the presumption is not automatically classified as either meeting or not meeting the level of care definition, but instead receives an individual determination on this point using the existing administrative criteria. This presumption recognizes the strong likelihood that those beneficiaries who are correctly assigned one of the designated case-mix classifiers during the immediate post-hospital period would require a covered level of care, which would be less likely for other beneficiaries.
In the July 30, 1999 final rule (64 FR 41670), we indicated that we would announce any changes to the guidelines for Medicare level of care determinations related to modifications in the case-mix classification structure. The FY 2018 final rule (82 FR 36544) further specified that we would henceforth disseminate the standard description of the administrative presumption's designated groups via the SNF PPS website at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/SNFPPS/ Start Printed Page 42442 index.html (where such designations appear in the paragraph entitled "Case Mix Adjustment"), and would publish such designations in rulemaking only to the extent that we actually intend to propose changes in them. Under that approach, the set of case-mix classifiers designated for this purpose under PDPM was finalized in the FY 2019 SNF PPS final rule (83 FR 39253) and is posted on the SNF PPS website (https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/SNFPPS/index.html), in the paragraph entitled "Case Mix Adjustment."
However, we note that this administrative presumption policy does not supersede the SNF's responsibility to ensure that its decisions relating to level of care are appropriate and timely, including a review to confirm that any services prompting the assignment of one of the designated case-mix classifiers (which, in turn, serves to trigger the administrative presumption) are themselves medically necessary. As we explained in the FY 2000 SNF PPS final rule (64 FR 41667), the administrative presumption is itself rebuttable in those individual cases in which the services actually received by the resident do not meet the basic statutory criterion of being reasonable and necessary to diagnose or treat a beneficiary's condition (according to section 1862(a)(1) of the Act). Accordingly, the presumption would not apply, for example, in those situations where the sole classifier that triggers the presumption is itself assigned through the receipt of services that are subsequently determined to be not reasonable and necessary. Moreover, we want to stress the importance of careful monitoring for changes in each patient's condition to determine the continuing need for Part A SNF benefits after the ARD of the initial Medicare assessment.
B. Consolidated Billing
Sections 1842(b)(6)(E) and 1862(a)(18) of the Act (as added by section 4432(b) of the BBA 1997) require a SNF to submit consolidated Medicare bills to its Medicare Administrative Contractor (MAC) for almost all of the services that its residents receive during the course of a covered Part A stay. In addition, section 1862(a)(18) of the Act places the responsibility with the SNF for billing Medicare for physical therapy, occupational therapy, and speech-language pathology services that the resident receives during a noncovered stay. Section 1888(e)(2)(A) of the Act excludes a small list of services from the consolidated billing provision (primarily those services furnished by physicians and certain other types of practitioners), which remain separately billable under Part B when furnished to a SNF's Part A resident. These excluded service categories are discussed in greater detail in section V.B.2. of the May 12, 1998 interim final rule (63 FR 26295 through 26297).
A detailed discussion of the legislative history of the consolidated billing provision is available on the SNF PPS website at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/SNFPPS/Downloads/Legislative_History_2018-10-01.pdf. In particular, section 103 of the BBRA 1999 amended section 1888(e)(2)(A)(iii) of the Act by further excluding a number of individual high-cost, low probability services, identified by HCPCS codes, within several broader categories (chemotherapy items, chemotherapy administration services, radioisotope services, and customized prosthetic devices) that otherwise remained subject to the provision. We discuss this BBRA 1999 amendment in greater detail in the SNF PPS proposed and final rules for FY 2001 (65 FR 19231 through 19232, April 10, 2000, and 65 FR 46790 through 46795, July 31, 2000), as well as in Program Memorandum AB-00-18 (Change Request #1070), issued March 2000, which is available online at www.cms.gov/transmittals/downloads/ab001860.pdf.
As explained in the FY 2001 proposed rule (65 FR 19232), the amendments enacted in section 103 of the BBRA 1999 not only identified for exclusion from this provision a number of particular service codes within four specified categories (that is, chemotherapy items, chemotherapy administration services, radioisotope services, and customized prosthetic devices), but also gave the Secretary the authority to designate additional, individual services for exclusion within each of these four specified service categories. In the proposed rule for FY 2001, we also noted that the BBRA 1999 Conference report (H.R. Rep. No. 106-479 at 854 (1999) (Conf. Rep.)) characterizes the individual services that this legislation targets for exclusion as high-cost, low probability events that could have devastating financial impacts because their costs far exceed the payment SNFs receive under the PPS. According to the conferees, section 103(a) of the BBRA 1999 is an attempt to exclude from the PPS certain services and costly items that are provided infrequently in SNFs. By contrast, the amendments enacted in section 103 of the BBRA 1999 do not designate for exclusion any of the remaining services within those four categories (thus, leaving all of those services subject to SNF consolidated billing), because they are relatively inexpensive and are furnished routinely in SNFs.
As we further explained in the final rule for FY 2001 (65 FR 46790), and as is consistent with our longstanding policy, any additional service codes that we might designate for exclusion under our discretionary authority must meet the same statutory criteria used in identifying the original codes excluded from consolidated billing under section 103(a) of the BBRA 1999: They must fall within one of the four service categories specified in the BBRA 1999; and they also must meet the same standards of high cost and low probability in the SNF setting, as discussed in the BBRA 1999 Conference report. Accordingly, we characterized this statutory authority to identify additional service codes for exclusion as essentially affording the flexibility to revise the list of excluded codes in response to changes of major significance that may occur over time (for example, the development of new medical technologies or other advances in the state of medical practice) (65 FR 46791).
Effective with items and services furnished on or after October 1, 2021, section 134 in Division CC of the Consolidated Appropriations Act, 2021 (Pub. L. 116-260) has established an additional category of excluded codes in section 1888(e)(2)(A)(iii)(VI) of the Act, for certain blood clotting factors for the treatment of patients with hemophilia and other bleeding disorders along with items and services related to the furnishing of such factors under section 1842(o)(5)(C) of the Act. The specific factors, and items and services related to the furnishing of such factors, excluded under this provision are those identified, as of July 1, 2020, by HCPCS codes J7170, J7175, J7177-J7183, J7185-J7190, J7192-J7195, J7198-J7203, J7205, and J7207-J7211. Like the provisions enacted in the BBRA 1999, new section 1888(e)(2)(A)(iii)(VI) of the Act gives the Secretary the authority to designate additional items and services for exclusion within the category of items and services described in that section. Section 1888(e)(4)(G)(iii) of the Act further requires that for any services that are unbundled from consolidated billing under section 1888(e)(2)(A)(iii) of the Act (and, thus, become qualified for separate payment under Part B), there must also be a corresponding proportional reduction made in aggregate SNF payments under Part A. Accordingly, using the methodology described in section III.B.6. of the proposed rule (see also section IV.B.6. of this final rule), we proposed to make a Start Printed Page 42443 proportional reduction of $0.02 in the unadjusted urban and rural rates to reflect these new exclusions, effective for items and services furnished on or after October 1, 2021.
In the proposed rule, we specifically invited public comments identifying HCPCS codes in any of these five service categories (chemotherapy items, chemotherapy administration services, radioisotope services, customized prosthetic devices, and blood clotting factors) representing recent medical advances that might meet our criteria for exclusion from SNF consolidated billing. We noted that we may consider excluding a particular service if it meets our criteria for exclusion as specified previously. We requested that commenters identify in their comments the specific HCPCS code that is associated with the service in question, as well as their rationale for requesting that the identified HCPCS code(s) be excluded.
We noted that the original BBRA amendment and the Consolidated Appropriations Act, 2021 identified a set of excluded items and services by means of specifying individual HCPCS codes within the designated categories that were in effect as of a particular date (in the case of the BBRA 1999, July 1, 1999, and in the case of the Consolidated Appropriations Act, 2021, July 1, 2020), as subsequently modified by the Secretary. In addition, as noted above, the statute (section 1888(e)(2)(A)(iii)(II) through (VI) of the Act) gives the Secretary authority to identify additional items and services for exclusion within the categories of items and services described in the statute, which are also designated by HCPCS code. Designating the excluded services in this manner makes it possible for us to utilize program issuances as the vehicle for accomplishing routine updates to the excluded codes to reflect any minor revisions that might subsequently occur in the coding system itself, such as the assignment of a different code number to a service already designated as excluded, or the creation of a new code for a type of service that falls within one of the established exclusion categories and meets our criteria for exclusion (for example, J7212, "factor viia (antihemophilic factor, recombinant)-jncw (sevenfact), 1 microgram", which became effective on January 1, 2021 and would fall in the blood clotting factor exclusion category).
Accordingly, we noted that in the event that we identify through the current rulemaking cycle any new services that would actually represent a substantive change in the scope of the exclusions from SNF consolidated billing, we would identify these additional excluded services by means of the HCPCS codes that are in effect as of a specific date (in this case, October 1, 2021). By making any new exclusions in this manner, we could similarly accomplish routine future updates of these additional codes through the issuance of program instructions. The latest list of excluded codes can be found on the SNF Consolidated Billing website at https://www.cms.gov/Medicare/Billing/SNFConsolidatedBilling.
The following is a summary of the public comments received on the proposed revisions to Consolidated Billing and our responses:
Comment: Several commenters noted support for the exclusion of blood clotting factors (BCFs) and related items and services from consolidated billing. Commenters stated that the exclusion of these services from consolidated billing will increase care to beneficiaries with BCF disorders.
Response: We thank these commenters for their support. In accordance with this support and the legislative mandate to exclude BCFs from consolidated billing, we are finalizing the exclusion of BCFs as proposed.
Comment: One commenter suggested the addition of two HCPCS codes to the list of BCF-related services that are excluded from consolidated billing: J7204 (effective as of 7/1/2020) and J7212 (effective as of 1/1/2021). The commenter stated that these two J Codes also represent treatments for people with hemophilia—J7204 is for hemophilia A and J7212 is for hemophilia A or B with inhibitors.
Response: Upon review, we agree with the commenter and we have determined that HCPCS codes J7204 and J7212 should be excluded from consolidated billing. HCPCS code J7212 was not created until January 1, 2021, after Division CC, section 134 of the Consolidated Appropriations Act of 2001 (CAA) (Pub. L. 116-260, enacted on December 27, 2000) had been enacted, and the statutory exclusion designates codes that were identified as of July 1, 2020. HCPCS code J7204 was added on July 1, 2020; by contrast, the immediately adjacent codes of J7203 and J7205 had already been added much earlier, in 2019 and 2016, respectively. Accordingly, HCPCS codes J7204 and J7212 were not included in the statutory code range provided in the aforementioned legislation. However, as we stated in the proposed rule, section 1888(e)(2)(A)(iii) (VI) of the Act gives the Secretary authority to identify any additional blood clotting factors for exclusion. We further stated that we will utilize program issuances as the vehicle for making such routine updates to the list of excluded codes. In fact, we used J7212 as an example of a new code that we would designate through the issuance of program instructions. Accordingly, the new exclusions for HCPCS codes J7204 and J7212 will appear in a forthcoming consolidated billing update, with an effective date of October 1, 2021, the date that the statutory exclusion for BCFs takes effect.
Comment: One commenter requested us to consider a particular chemotherapy drug, RIABNITM (rituximab-arrx), HCPCS code Q5123, that the commenter recommended as meeting the criteria for exclusion from consolidated billing. The commenter stated the drug meets the "high-cost, low probability" criteria for exclusion, represents a change in medical technology, and already has its own HCPCS code.
Response: We agree with the commenter and have determined that the drug described by HCPCS code Q5123 does qualify for exclusion. Its cost is comparable to other excluded chemotherapy drugs and it is rarely administered to SNF inpatients. Thus, it meets the "high-cost, low probability" standard in the SNF setting, as discussed in the BBRA 1999 Conf. Report. Furthermore, since it is a newly assigned code, the omission of this particular code from the original statutory code range would not indicate an intent for it to remain bundled. Accordingly, this new exclusion will appear in a forthcoming consolidated billing update.
Comment: One commenter encouraged CMS to exclude erythropoietin (EPO) when given for non-dialysis use. The commenter stated that currently CMS excludes erythropoietin (EPO) when given for dialysis, but not for other uses.
Response: We note that we have responded previously to comments regarding the use of EPO for non-dialysis purposes, including in the FY 2004 (68 FR 46059-62, August 4, 2003), FY 2006 (70 FR 45048-50, August 4, 2005), and FY 2008 (72 FR 43430-32, August 3, 2007) final rules. As we have noted previously in this final rule and in previous responses to comments on this issue in the past, section 1888(e)(2)(A)(iii) of the Act authorizes us to identify additional services for exclusion only within those particular service categories that it has designated for this purpose, and does not give us the authority to exclude other services which, though they may be related, fall Start Printed Page 42444 outside of the specified service categories themselves. Thus, while anti-emetics, for example, are commonly administered in conjunction with chemotherapy, they are not themselves inherently chemotherapeutic in nature and, consequently, do not fall within the excluded chemotherapy category designated in the section 1888(e)(2)(A)(iii)(II) of the Act. With regard to EPO, we additionally note that among the service categories that section 1888(e)(2)(A)(ii) of the Act already specifies as being excluded from SNF consolidated billing are items and services described in section 1861(s)(2)(O) of the Act—that is, EPO that is furnished to dialysis patients competent to use the such drug without medical or other supervision, and does not provide for coverage in any other, non-dialysis situations, such as chemotherapy. This means the exclusion under the consolidated billing provision for EPO falls within this scope.
Comment: One commenter reiterated the same set of comments that they had submitted in previous rulemaking cycles, noting the importance of continuing to exclude certain customized prosthetic devices from consolidated billing, and urging the exclusion of orthotics as well. The commenter also recommended the following four HCPCS codes for exclusion: L5000—Partial foot, shoe insert with longitudinal arch, toe filler; L5010—Partial foot, molded socket, ankle height, with toe filler; L5020—Partial foot, molded socket, tibial tubercle height, with toe filler; and L5987—All lower extremity prosthesis, shank foot system with vertical loading pylon.
Response: We refer to the previous discussions in the FY 2018 SNF PPS final rule (82 FR 36547) and FY 2017 SNF PPS final rule (81 FR 51986, August 5, 2016) regarding our decision not to adopt the recommendations for excluding orthotics as a class along with prosthetic codes L5010, L5020, and L5987. As we explained, it is our longstanding position that if a particular prosthetic code was already in existence as of the BBRA enactment date but was not designated in the BBRA for exclusion, this meant that it was intended to remain within the SNF PPS bundle. This would apply to all four of the prosthetic codes (L5000, L5010, L5020, and L5987) cited in the current comment.
Comment: One commenter encouraged CMS to address whether monoclonal antibody infusions for treatment of COVID-19 will be excluded from consolidated billing after the end of the COVID-19 PHE, to continue efforts to combat the infection in facilities.
Response: We appreciate the commenter's concern. However, as previously described in this rule, section 1888(e)(2)(A) of the Act authorizes us to identify additional services for exclusion from the consolidated billing requirements only within those particular service categories that it has designated for this purpose, and does not give us the authority to exclude other services which fall outside of the specified service categories themselves. Monoclonal antibody infusions do not fall within one of the specified service categories.
C. Payment for SNF-Level Swing-Bed Services
Section 1883 of the Act permits certain small, rural hospitals to enter into a Medicare swing-bed agreement, under which the hospital can use its beds to provide either acute- or SNF-level care, as needed. For critical access hospitals (CAHs), Part A pays on a reasonable cost basis for SNF-level services furnished under a swing-bed agreement. However, in accordance with section 1888(e)(7) of the Act, SNF-level services furnished by non-CAH rural hospitals are paid under the SNF PPS, effective with cost reporting periods beginning on or after July 1, 2002. As explained in the FY 2002 final rule (66 FR 39562), this effective date is consistent with the statutory provision to integrate swing-bed rural hospitals into the SNF PPS by the end of the transition period, June 30, 2002.
Accordingly, all non-CAH swing-bed rural hospitals have now come under the SNF PPS. Therefore, all rates and wage indexes outlined in earlier sections of this final rule for the SNF PPS also apply to all non-CAH swing-bed rural hospitals. As finalized in the FY 2010 SNF PPS final rule (74 FR 40356 through 40357), effective October 1, 2010, non-CAH swing-bed rural hospitals are required to complete an MDS 3.0 swing-bed assessment which is limited to the required demographic, payment, and quality items. As discussed in the FY 2019 SNF PPS final rule (83 FR 39235), revisions were made to the swing bed assessment to support implementation of PDPM, effective October 1, 2019. A discussion of the assessment schedule and the MDS effective beginning FY 2020 appears in the FY 2019 SNF PPS final rule (83 FR 39229 through 39237). The latest changes in the MDS for swing-bed rural hospitals appear on the SNF PPS website at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/SNFPPS/index.html.
D. Revisions to the Regulation Text
In the proposed rule, we proposed to make certain revisions in the regulation text itself. Specifically, we proposed to redesignate current 42 CFR 411.15(p)(2)(xvii) and 489.20(s)(17) to §§ 411.15(p)(2)(xviii) and 489.20(s)(18), respectively, and to update the regulation text at §§ 411.15(p)(2)(xvii) and 489.20(s)(17) to reflect the recently-enacted exclusion from SNF consolidated billing at section 1888(e)(2)(A)(iii)(VI) of the Act effective for items and services furnished on or after October 1, 2021. Specifically, proposed revised §§ 411.15(p)(2)(xvii) and 489.20(s)(17) would reflect the exclusion of certain blood clotting factors for the treatment of patients with hemophilia and other bleeding disorders (identified by designated HCPCS codes in effect as of July 1, 2020, as subsequently modified by CMS), and items and services related to the furnishing of such factors, and would allow for the exclusion of any additional blood clotting factors identified by CMS and items and services related to the furnishing of such factors. In addition, we proposed to make conforming changes to the regulation text at §§ 411.15(p)(2)(xiii) through (xvi) and 489.20(s)(13) through (16) to reflect the authority that has always existed for CMS to make updates to the list of excluded codes as provided in section 1888(e)(2)(A)(iii)(II) through (V) of the Act, and as discussed in section IV.C. of the proposed rule.
The following is a summary of the public comment received on the proposed revisions to the regulation text and our response:
Comment: One commenter noted support for the regulation text revisions.
Response: We thank the commenter for their support. We did not receive any other comments on the proposed revisions to the regulation text, and therefore, we are finalizing the revisions as proposed.
VI. Other SNF PPS Issues
A. Rebasing and Revising the SNF Market Basket
Section 1888(e)(5)(A) of the Act requires the Secretary to establish a market basket index that reflects the changes over time in the prices of an appropriate mix of goods and services included in covered SNF services. Accordingly, we have developed a SNF market basket index that encompasses the most commonly used cost categories for SNF routine services, ancillary Start Printed Page 42445 services, and capital-related expenses. We use the SNF market basket index, adjusted in the manner described in section III.B. of this final rule, to update the SNF PPS per diem rates and to determine the labor-related share on an annual basis.
The SNF market basket is a fixed-weight, Laspeyres-type price index. A Laspeyres price index measures the change in price, over time, of the same mix of goods and services purchased in the base period. Any changes in the quantity or mix of goods and services (that is, intensity) purchased over time relative to a base period are not measured.
The index itself is constructed in three steps. First, a base period is selected (the base period is 2018) and total base period expenditures are estimated for a set of mutually exclusive and exhaustive spending categories and the proportion of total costs that each category represents is calculated. These proportions are called cost or expenditure weights. Second, each expenditure category is matched to an appropriate price or wage variable, referred to as a price proxy. In nearly every instance, these price proxies are derived from publicly available statistical series that are published on a consistent schedule (preferably at least on a quarterly basis). Finally, the expenditure weight for each cost category is multiplied by the level of its respective price proxy. The sum of these products (that is, the expenditure weights multiplied by their price levels) for all cost categories yields the composite index level of the market basket in a given period. Repeating this step for other periods produces a series of market basket levels over time. Dividing an index level for a given period by an index level for an earlier period produces a rate of growth in the input price index over that timeframe.
Effective for cost reporting periods beginning on or after July 1, 1998, we revised and rebased our 1977 routine costs input price index and adopted a total expenses SNF input price index using FY 1992 as the base year. In the FY 2002 SNF PPS final rule (66 FR 39582), we rebased and revised the market basket to a base year of FY 1997. In the FY 2008 SNF PPS final rule (72 FR 43425), we rebased and revised the market basket to a base year of FY 2004. In the FY 2014 SNF PPS final rule (78 FR 47939), we revised and rebased the SNF market basket, which included updating the base year from FY 2004 to FY 2010. Lastly, in the FY 2018 SNF PPS final rule (82 FR 36548), we revised and rebased the SNF market basket, which included updating the base year from FY 2010 to FY 2014. In the FY 2022 SNF PPS proposed rule (86 FR 19969 through 19984) we proposed to rebase and revise the market basket updating the base year from 2014 to 2018. Below is our methodology, as well as responses to comments.
Effective for FY 2022 and subsequent fiscal years, we will rebase and revise the market basket to reflect 2018 Medicare-allowable total cost data (routine, ancillary, and capital-related) from freestanding SNFs and to revise applicable cost categories and price proxies used to determine the market basket. Medicare-allowable costs are those costs that are eligible to be paid under the SNF PPS. For example, the SNF market basket excludes home health agency (HHA) costs as these costs would be paid under the HHA PPS, and therefore, these costs are not SNF PPS Medicare-allowable costs. We will maintain our policy of using data from freestanding SNFs, which represent about 93 percent of the total SNFs shown in Table 12. We believe using freestanding Medicare cost report (MCR) data, as opposed to the hospital-based SNF MCR data, for the cost weight calculation is most appropriate because of the complexity of hospital-based data and the representativeness of the freestanding data. Because hospital-based SNF expenses are embedded in the hospital cost report, any attempt to incorporate data from hospital-based facilities requires more complex calculations and assumptions regarding the ancillary costs related to the hospital-based SNF unit. We believe the use of freestanding SNF cost report data is technically appropriate for reflecting the cost structures of SNFs serving Medicare beneficiaries.
We will use 2018 as the base year as we believe that the 2018 MCRs represent the most recent, complete set of MCR data available to develop cost weights for SNFs at the time of rulemaking. We believe it is important to regularly rebase and revise the SNF market to reflect more recent data. Historically, the cost weights change minimally from year to year as they represent percent of total costs rather than cost levels; however, given the COVID-19 PHE, we will continue to monitor the upcoming MCR data to see if a more frequent rebasing schedule is necessary than our recent historical precedent of about every 4 years. The 2018 Medicare cost reports are for cost reporting periods beginning on and after October 1, 2017 and before October 1, 2018. While these dates appear to reflect fiscal year data, we note that a Medicare cost report that begins in this timeframe is generally classified as a "2018 cost report". For example, we found that of the available 2018 Medicare cost reports for SNFs, approximately 7 percent had an October 1, 2017 begin date, approximately 70 percent of the reports had a January 1, 2018 begin date, and approximately 12 percent had a July 1, 2018 begin date. For this reason, we are defining the base year of the market basket as "2018-based" instead of "FY 2018-based".
Comment: Several commenters supported the rebasing and revising of the market basket, stating that a relevant market basket is a fundamental requirement for a well-functioning PPS. One commenter appreciated the proposed rebasing and revising of the SNF market basket as proposed and further stated that the use of the 2018 data is more reflective of current costs of providing services compared to 2014 data. Several commenters also supported CMS' plans to monitor and revise and rebase more frequently.
Response: We appreciate the commenters' support of the rebasing and revising of the SNF market basket and note that we plan to review the 2020 Medicare cost report data as soon as complete information is available to assess any impact of the PHE on the market basket relative cost shares. Any changes to the market basket would be proposed in rulemaking and will be subject to public comments.
We proposed to develop cost category weights for the 2018-based SNF market basket in two stages. First, we proposed to derive eight major expenditures or cost weights from the 2018 MCR data (CMS Form 2540-10, OMB NO. 0938-0463) for freestanding SNFs: Wages and Salaries; Employee Benefits; Contract Labor; Pharmaceuticals; Professional Liability Insurance; Home Office/Related Organization Contract Labor; Capital-related; and a residual "All Other". These are the same cost categories calculated using the 2014 MCR data for the 2014-based SNF market basket. The residual "All Other" category would reflect all remaining costs that are not captured in the other seven cost categories. Second, we proposed to divide the residual "All Other" cost category into more detailed subcategories, using U.S. Department of Commerce Bureau of Economic Analysis' (BEA) 2012 Benchmark Input-Output (I-O) "use table before redefinitions, purchaser's value" for the Nursing and Community Care Facilities industry (NAICS 623A00) aged to 2018 using applicable price proxy growth for each category of costs. Furthermore, we proposed to continue to use the same overall methodology as was used for the 2014-based SNF market basket to Start Printed Page 42446 develop the capital related cost weights of the 2018-based SNF market basket.
1. Development of Cost Categories and Weights
a. Use of Medicare Cost Report Data To Develop Major Cost Weights
In order to create a market basket that is representative of freestanding SNF providers serving Medicare patients and to help ensure accurate major cost weights (which is the percent of total Medicare-allowable costs, as defined below), we proposed to apply edits to remove reporting errors and outliers. Specifically, the SNF MCRs used to calculate the market basket cost weights exclude any providers that reported costs less than or equal to zero for the following categories: Total facility costs (Worksheet B, part 1, column 18, line 100); total operating costs (Worksheet B, part 1, column 18, line 100 less Worksheet B, part 2, column 18, line 100); Medicare general inpatient routine service costs (Worksheet D, part 1, column 1, line 1); and Medicare PPS payments (Worksheet E, part 3, column 1, line 1). We also limited our sample to providers that had a MCR reporting period that was between 10 and 14 months. The final sample used included roughly 13,500 MCRs (about 90 percent of the universe of SNF MCRs for 2018). The sample of providers is representative of the national universe of providers by region, by ownership-type (proprietary, nonprofit, and government), and by urban/rural status. Additionally, for all of the major cost weights, except Home Office/Related Organization Contract Labor costs, the data are trimmed to remove outliers (a standard statistical process) by: (1) Requiring that major expenses (such as Wages and Salaries costs) and total Medicare-allowable costs are greater than zero; and (2) excluding the top and bottom 5 percent of the major cost weight (for example, Wages and Salaries costs as a percent of total Medicare-allowable costs). We note that missing values are assumed to be zero, consistent with the methodology for how missing values are treated in the 2014-based market basket methodology.
For the Home Office/Related Organization Contract Labor cost weight, we proposed to first exclude providers whose Home Office/Related Organization Contract Labor costs are greater than Medicare-allowable total costs and then apply a trim that excludes those reporters with a Home Office/Related Organization Contract Labor cost weight above the 99th percentile. This allows providers with no Home Office/Related Organization Contract Labor costs to be included in the Home Office/Related Organization Contract Labor cost weight calculation . If we were to trim the top and bottom Home Office/Related Organization Contract Labor cost weight, we would exclude providers with a zero cost weight and the MCR data (WorksheetS-2 line 45) indicate that not all SNF providers have a home office. Providers without a home office would report administrative costs that might typically be associated with a home office in the Wages and Salaries and Employee Benefits cost weights, or in the residual "All-Other" cost weight if they purchased these types of services from external contractors. We believe the trimming methodology that excludes those who report Home Office costs above the 99th percentile is appropriate as it removes extreme outliers while also allowing providers with zero Home Office/Related Organization Contract Labor costs to be included in the Home Office/Related Organization Contract Labor cost weight calculation.
The trimming process is done individually for each cost category so that providers excluded from one cost weight calculation are not automatically excluded from another cost weight calculation. We note that these trimming methods are the same types of edits performed for the 2014-based SNF market basket, as well as other PPS market baskets (including but not limited to the IPPS market basket and HHA market basket). We believe this trimming process improves the accuracy of the data used to compute the major cost weights by removing possible data misreporting.
The final weights of the 2018-based SNF market basket are based on weighted means. For example, the aggregate Wages and Salaries cost weight, after trimming, is equal to the sum of total Medicare-allowable wages and salaries of all providers divided by the sum of total Medicare-allowable costs for all providers in the sample. This methodology is consistent with the methodology used to calculate the 2014-based SNF market basket cost weights and other PPS market basket cost weights. We note that for each of the cost weights, we evaluated the distribution of providers and costs by region, by ownership-type, and by urban/rural status. For all of the cost weights, with the exception of the PLI (which is discussed in more detail later), the trimmed sample was nationally representative.
For all of the cost weights, we use Medicare-allowable total costs as the denominator (for example, Wages and Salaries cost weight = Wages and Salaries costs divided by Medicare-allowable total costs). Medicare-allowable total costs were equal to total costs (after overhead allocation) from Worksheet B part I, column 18, for lines 30, 40 through 49, 51, 52, and 71 plus estimated Medicaid drug costs, as defined below. We included estimated Medicaid drug costs in the pharmacy cost weight, as well as the denominator for total Medicare-allowable costs. This is the same methodology used for the 2014-based SNF market basket. The inclusion of Medicaid drug costs was finalized in the FY 2008 SNF PPS final rule (72 FR 43425 through 43430), and for the same reasons set forth in that final rule, we proposed to continue to use this methodology in the 2018-based SNF market basket.
We describe the detailed methodology for obtaining costs for each of the eight cost categories determined from the Medicare Cost Report below. The methodology used in the 2014-based SNF market basket can be found in the FY 2018 SNF PPS final rule (82 FR 36548 through 36555).
(1) Wages and Salaries: To derive Wages and Salaries costs for the Medicare-allowable cost centers, we proposed first to calculate total facility wages and salaries costs as reported on Worksheet S-3, part II, column 3, line 1. We then proposed to remove the wages and salaries attributable to non-Medicare-allowable cost centers (that is, excluded areas), as well as a portion of overhead wages and salaries attributable to these excluded areas. Excluded area wages and salaries are equal to wages and salaries as reported on Worksheet S-3, part II, column 3, lines 3, 4, and 7 through 11 plus nursing facility and non-reimbursable salaries from Worksheet A, column 1, lines 31, 32, 50, and 60 through 63.
Overhead wages and salaries are attributable to the entire SNF facility; therefore, we proposed to include only the proportion attributable to the Medicare-allowable cost centers. We proposed to estimate the proportion of overhead wages and salaries attributable to the non-Medicare-allowable costs centers in two steps. First, we proposed to estimate the ratio of excluded area wages and salaries (as defined above) to non-overhead total facility wages and salaries (total facility wages and salaries (Worksheet S-3, part II, column 3, line 1) less total overhead wages and salaries (Worksheet S-3, Part III, column 3, line 14)). Next, we proposed to multiply total overhead wages and salaries by the ratio computed in step 1. We excluded providers whose excluded areas wages and salaries were greater than total facility wages and salaries and/or their Start Printed Page 42447 excluded area overhead wages and salaries were greater than total facility wages and salaries (about 50 providers). This is similar to the methodology used to derive Wages and Salaries costs in the 2014-based SNF market basket. For the 2014-based SNF market basket, we estimated the proportion of overhead wages and salaries that is attributable to the non-Medicare allowable costs centers (that is, excluded areas) by multiplying the ratio of excluded area wages and salaries (as defined above) to total wages and salaries as reported on Worksheet S-3, Part II, column 3, line 1 by total overhead wages and salaries as reported on Worksheet S-3, Part III, column 3, line 14.
(2) Employee Benefits: Medicare-allowable employee benefits are equal to total facility benefits as reported on Worksheet S-3, part II, column 3, lines 17 through 19 minus non-Medicare-allowable (that is, excluded area) employee benefits and minus a portion of overhead benefits attributable to these excluded areas. Excluded area employee benefits are derived by multiplying total excluded area wages and salaries (as defined above in the `Wages and Salaries' section) times the ratio of total facility benefits to total facility wages and salaries. This ratio of benefits to wages and salaries is defined as total facility benefit costs to total facility wages and salary costs (as reported on Worksheet S-3, part II, column 3, line 1). Likewise, the portion of overhead benefits attributable to the excluded areas is derived by multiplying overhead wages and salaries attributable to the excluded areas (as defined in the `Wages and Salaries' section) times the ratio of total facility benefit costs to total facility wages and salary costs (as defined above). Similar to the Wages and Salaries cost weight, we excluded providers whose excluded areas benefits were greater than total facility benefits and/or their excluded area overhead benefits were greater than total facility benefits (zero providers were excluded because of this edit). This is similar to the methodology used to derive Employee Benefits costs in the 2014-based SNF market basket.
(3) Contract Labor: We proposed to derive Medicare-allowable contract labor costs from Worksheet S-3, part II, column 3, line 14, which reflects costs for contracted direct patient care services (that is, nursing, therapeutic, rehabilitative, or diagnostic services furnished under contract rather than by employees and management contract services). This is the same methodology used to derive the Contract Labor costs in the 2014-based SNF market basket.
(4) Pharmaceuticals: We proposed to calculate pharmaceuticals costs using the non-salary costs from the Pharmacy cost center (Worksheet B, part I, column 0, line 11 less Worksheet A, column 1, line 11) and the Drugs Charged to Patients' cost center (Worksheet B, part I, column 0, line 49 less Worksheet A, column 1, line 49). Since these drug costs were attributable to the entire SNF and not limited to Medicare-allowable services, we proposed to adjust the drug costs by the ratio of Medicare-allowable pharmacy total costs (Worksheet B, part I, column 11, for lines 30, 40 through 49, 51, 52, and 71) to total pharmacy costs from Worksheet B, part I, column 11, line 11. Worksheet B, part I allocates the general service cost centers, which are often referred to as "overhead costs" (in which pharmacy costs are included) to the Medicare-allowable and non-Medicare-allowable cost centers. This adjustment was made for those providers who reported Pharmacy cost center expenses. Otherwise, we assumed the non-salary Drugs Charged to Patients costs were Medicare-allowable. Since drug costs for Medicare patients are included in the SNF PPS per diem rate, a provider with Medicare days should have also reported costs in the Drugs Charged to Patient cost center. We found a small number of providers (roughly 60) did not report Drugs Charged to Patients' costs despite reporting Medicare days (an average of about 2,600 Medicare days per provider), and therefore, these providers were excluded from the Pharmaceuticals cost weight calculations. This is similar to the methodology used for the 2014-based SNF market basket.
Second, as was done for the 2014-based SNF market basket, we proposed to continue to adjust the drug expenses reported on the MCR to include an estimate of total Medicaid drug costs, which are not represented in the Medicare-allowable drug cost weight. As stated previously in this section, the 2018-based SNF market basket reflects total Medicare-allowable costs (that is, total costs for all payers for those services reimbursable under the SNF PPS). For the FY 2006-based SNF market basket (72 FR 43426), commenters noted that the total pharmaceutical costs reported on the MCR did not include pharmaceutical costs for dual-eligible Medicaid patients as these were directly reimbursed by Medicaid. Since all of the other cost category weights reflect expenses associated with treating Medicaid patients (including the compensation costs for dispensing these drugs), we made an adjustment to include these Medicaid drug expenses so the market basket cost weights would be calculated consistently.
Similar to the 2014-based SNF market basket, we proposed to estimate Medicaid drug costs based on data representing dual-eligible Medicaid beneficiaries. Medicaid drug costs are estimated by multiplying Medicaid dual-eligible drug costs per day times the number of Medicaid days as reported in the Medicare-allowable skilled nursing cost center (Worksheet S-3, part I, column 5, line 1) in the SNF MCR. Medicaid dual-eligible drug costs per day (where the day represents an unduplicated drug supply day) were estimated using 2018 Part D claims for those dual-eligible beneficiaries who had a Medicare SNF stay during the year. The total drug costs per unduplicated day for 2018 of $24.48 represented all drug costs (including the drug ingredient cost, the dispensing fee, vaccine administration fee and sales tax) incurred during the 2018 calendar year for those dual-eligible beneficiaries who had a SNF Medicare stay during that 2018 calendar year. Therefore, they include drug costs incurred during a Medicaid SNF stay occurring in the 2018 calendar year. By comparison, the 2014-based SNF market basket also relied on data from the Part D claims, which yielded a dual-eligible Medicaid drug cost per day of $19.62 for 2014.
We continue to believe that Medicaid dual-eligible beneficiaries are a reasonable proxy for the estimated drug costs per day incurred by Medicaid patients staying in a skilled nursing unit under a Medicaid stay. The skilled nursing unit is the Medicare-allowable unit in a SNF, which encompasses more skilled nursing and rehabilitative care compared to a nursing facility or long-term care unit. We believe that Medicaid patients receiving this skilled nursing care would on average have similar drug costs per day to dual-eligible Medicare beneficiaries who have received Medicare skilled nursing care in the skilled nursing care unit during the year. We note that our previous analysis of the Part D claims data showed that Medicare beneficiaries with a SNF stay during the year have higher drug costs than Medicare patients without a SNF stay during the year. Also, in 2018, dual-eligible beneficiaries with a SNF stay during the year had drug costs per day of $24.48, which were approximately two times higher than the drug costs per day of $13.19 for nondual-eligible beneficiaries with a SNF Part A stay during the year.
The Pharmaceuticals cost weight using only 2018 MCR data (without the Start Printed Page 42448 inclusion of the Medicaid dual-eligible drug costs) is 2.6 percent, compared to the proposed Pharmaceuticals cost weight (including the adjustment for Medicaid dual-eligible drug costs) of 7.5 percent. The 2014-based SNF market basket had a Pharmaceuticals cost weight using only 2014 MCR data without the inclusion of the Medicaid dual-eligible drug costs of 2.9 percent and a total Pharmaceuticals cost weight of 7.3 percent. Therefore, the 0.2 percentage point increase in the Pharmaceuticals cost weight is a result of a 0.5-percentage point increase in the Medicaid dual-eligible drug cost weight (reflecting the 25 percent increase in the Medicaid dual-eligible drug costs per day between 2014 and 2018) and a 0.3-percentage point decrease in the MCR drug cost weight. The decrease in the MCR drug cost weight was consistent, in aggregate, across urban and rural status SNFs as well as across for-profit, government, and nonprofit ownership type SNFs.
(5) Professional Liability Insurance: We proposed to calculate the professional liability insurance (PLI) costs from Worksheet S-2 of the MCRs as the sum of premiums; paid losses; and self-insurance (Worksheet S-2, Part I, columns 1 through 3, line 41). This was the same methodology used to derive the Professional Liability costs for the 2014-based SNF market basket.
About 60 percent of SNFs (about 8,000) reported professional liability costs. After trimming, about 7,200 (reflecting about 850,000 Skilled Nursing unit beds) were included in the calculation of the PLI cost weight for the 2018-based SNF market basket. These providers treated roughly 870,000 Medicare beneficiaries and had a Medicare length of stay (LOS) of 33 days, a skilled nursing unit occupancy rate of 80 percent, and an average skilled nursing unit bed size of 125 beds, which are all consistent with the national averages. We also verified that this sample of providers are representative of the national distribution of providers by ownership-type and urban/rural status. We note that the sample of providers is less consistent with the national distribution of providers by region; however, we performed a sensitivity analysis where the PLI cost weight was reweighted based on the national regional distribution and the impacts were less than a 0.1 percentage point on the cost weight.
We note that based on prior comments during the rebasing of the 2014-based SNF market basket, we reviewed in detail the AON 2018 Professional and General Liability Benchmark for Long Term Care Providers[2] that examines professional liability and general liability claim costs for long term care providers (including skilled nursing facility beds as well as independent living, assisted living, home health care, and rehabilitation facilities, representing about 186,000 long term care beds). This study, although informative, was not appropriate for calculating a PLI cost weight as it represents more than just SNFs serving Medicare patients and captures claim losses as opposed to PLI costs (premiums, paid losses, and self-insurance) incurred during a cost reporting year. We note that only 13 percent of providers reported PLI paid losses or PLI self-insurance costs on the MCR while over 90 percent of providers reported PLI premiums indicating that the majority of losses incurred by Medicare participating SNFs will be covered by insurance premiums paid over time. Our comparison of the MCR data to the AON study for those select states' data provided did show consistencies between the average state PLI costs per bed relative to the national average (as measured by the MCR) and AON's loss per occupied bed relative to national values indicating that states with higher losses per occupied bed have higher PLI costs per total bed.
We believe the MCR data continues to be the most appropriate data source to calculate the PLI cost weight for the 2018-based SNF market basket as it is representative of SNFs serving Medicare beneficiaries and reflects PLI costs (premiums, paid losses, and self-insurance) incurred during the provider's cost reporting year.
(6) Capital-Related: We proposed to derive the Medicare-allowable capital-related costs from Worksheet B, part II, column 18 for lines 30, 40 through 49, 51, 52, and 71. This is the same methodology to derive capital-related costs used in the 2014-based SNF market basket.
(7) Home Office/Related Organization Contract Labor Costs: We proposed to calculate Medicare-allowable Home Office/Related Organization Contract Labor costs to be equal to data reported on Worksheet S-3, part II, column 3, line 16. We note that for the 2014-based SNF market basket we also used Worksheet S-3, part II, column 3, line 16 (Home office salaries & wage related costs) to determine these expenses; however, we referred to this category as Home Office Contract Labor Costs. The instructions for this data state "enter the salaries and wage related costs (as defined on lines 17 and 18 below) paid to personnel who are affiliated with a home office and/or related organization, who provide services to the SNF and/or NF, and whose salaries are not included on Worksheet A, column 1," and therefore, we are referring to this cost category as Home Office/Related Organization Contract Labor costs. Furthermore, for this rebasing we no longer adjusted these expenses by the ratio of Medicare allowable operating costs to total facility operating costs as done for the 2014-based SNF market basket as the instructions indicate these expenses are for the SNF and NF units.
About 7,000 providers (about 53 percent) in 2018 reported having a home office (as reported on Worksheet S-2, part I, line 45); a lower share of providers than those in the 2014-based SNF market basket. As discussed in section VI.A.1. of this final rule, providers without a home office can incur these expenses directly by having their own staff, for which the costs would be included in the Wages and Salaries and Employee Benefits cost weights. Alternatively, providers without a home office could also purchase related services from external contractors for which these expenses would be captured in the residual "All-Other" cost weight. For this reason, unlike the other major cost weights described previously, we did not exclude providers that did not report Home Office/Related Organization Contract Labor costs. We note that this is similar to the methodology that was used for other PPS market baskets such as the 2017-based LTCH market basket (85 FR 58911).
(8) All Other (residual): The "All Other" cost weight is a residual, calculated by subtracting the major cost weights (Wages and Salaries, Employee Benefits, Contract Labor, Pharmaceuticals, Professional Liability Insurance, Capital-Related, and Home Office/Related Organization Contract Labor) from 100.
Table 12 shows the major cost categories and their respective cost weights as derived from the 2018 Medicare cost reports.
Start Printed Page 42449

Compared to the 2014-based SNF market basket, the Wages and Salaries cost weight and the Employee Benefits cost weight as calculated directly from the Medicare cost reports decreased by 0.2 percentage point and 0.7 percentage point, respectively. The Contract Labor cost weight increased 0.7 percentage point and so in aggregate, the Compensation cost weight decreased 0.2 percentage point.
As we did for the 2014-based SNF market basket (82 FR 36555), we proposed to allocate contract labor costs to the Wages and Salaries and Employee Benefits cost weights based on their relative proportions under the assumption that contract labor costs are comprised of both wages and salaries and employee benefits. The contract labor allocation proportion for wages and salaries is equal to the Wages and Salaries cost weight as a percent of the sum of the Wages and Salaries cost weight and the Employee Benefits cost weight. Using the 2018 Medicare cost report data, this percentage is 84 percent (1 percentage point higher than the percent in the 2014-based SNF market basket); therefore, we proposed to allocate approximately 84 percent of the Contract Labor cost weight to the Wages and Salaries cost weight and 16 percent to the Employee Benefits cost weight.
Table 13 shows the Wages and Salaries and Employee Benefits cost weights after contract labor allocation for the 2018-based SNF market basket and the 2014-based SNF market basket.

b. Derivation of the Detailed Operating Cost Weights
To further divide the "All Other" residual cost weight estimated from the 2018 Medicare cost report data into more detailed cost categories, we proposed to use the 2012 Benchmark I-O "Use Tables/Before Redefinitions/Purchaser Value" for Nursing and Community Care Facilities industry (NAICS 623A00), published by the Census Bureau's, Bureau of Economic Analysis (BEA). These data are publicly available at http://www.bea.gov/industry/io_annual.htm. The BEA Benchmark I-O data are generally scheduled for publication every 5 years with 2012 being the most recent year for which data is available. The 2012 Benchmark I-O data are derived from the 2012 Economic Census and are the building blocks for BEA's economic accounts; therefore, they represent the most comprehensive and complete set of data on the economic processes or mechanisms by which output is produced and distributed.[3] BEA also produces Annual I-O estimates. However, while based on a similar methodology, these estimates are less comprehensive and provide less detail than benchmark data. Additionally, the annual I-O data are subject to revision once benchmark data become available. For these reasons, we proposed to inflate the 2012 Benchmark I-O data aged forward to 2018 by applying the annual price changes from the respective price proxies to the appropriate market basket cost categories that are obtained from the 2012 Benchmark I-O data. Next, the relative shares of the cost shares that each cost category represents to the total residual I-O costs are calculated. These resulting 2018 cost shares of the I-O data are applied to the "All Other" residual cost weight to obtain detailed cost weights for the residual costs for the 2018-based SNF market basket. For example, the cost for Food: Direct Purchases represents 11.3 percent of the sum of the "All Other" 2012 Benchmark I-O Expenditures inflated to 2018. Therefore, the Food: Direct Purchases cost weight is 2.5 percent of the 2018-based SNF market basket (11.3 percent × 22.3 percent = 2.5 percent). For the 2014-based SNF market basket (82 FR 36553), we used a similar methodology utilizing the 2007 Benchmark I-O data (aged to 2014).
Using this methodology, we proposed to derive 19 detailed SNF market basket cost category weights from the 2018-based SNF market basket "All Other" residual cost weight (22.3 percent). These categories are: (1) Fuel: Oil and Gas; (2) Electricity and Other Non-Fuel Utilities; (3) Food: Direct Purchases; (4) Food: Contract Services; (5) Chemicals; (6) Medical Instruments and Supplies; (7) Rubber and Plastics; (8) Paper and Printing Products; (9) Apparel; (10) Machinery and Equipment; (11) Miscellaneous Products; (12) Start Printed Page 42450 Professional Fees: Labor-Related; (13) Administrative and Facilities Support Services; (14) Installation, Maintenance, and Repair Services; (15) All Other: Labor-Related Services; (16) Professional Fees: Nonlabor-Related; (17) Financial Services; (18) Telephone Services; and (19) All Other: Nonlabor-Related Services. The 2014-based SNF market basket had separate cost categories for Postage services and Water and Sewerage. Due to the small weights (less than 0.1 percentage point), we proposed that Postage costs be included in the All Other: Non-labor-Related Services and Water and Sewerage costs be included in the Electricity and Other Non-Fuel Utilities category. We note that the machinery and equipment expenses are for equipment that is paid for in a given year and not depreciated over the asset's useful life. Depreciation expenses for moveable equipment are accounted for in the capital component of the 2018-based SNF market basket (described in section IV.A.1.c. of this final rule).
c. Derivation of the Detailed Capital Cost Weights
Similar to the 2014-based SNF market basket, we further divided the Capital-related cost weight into: Depreciation, Interest, Lease and Other Capital-related cost weights.
We calculated the depreciation cost weight (that is, depreciation costs excluding leasing costs) using depreciation costs from Worksheet S-2, column 1, lines 20 and 21. Since the depreciation costs reflect the entire SNF facility (Medicare and non-Medicare-allowable units), we used total facility capital costs (Worksheet B, Part I, Column 18, line 100) as the denominator. This methodology assumes that the depreciation of an asset is the same regardless of whether the asset was used for Medicare or non-Medicare patients. This methodology yielded depreciation costs as a percent of capital costs of 25.3 percent for 2018. We then apply this percentage to the 2018-based SNF market basket Medicare-allowable Capital-related cost weight of 8.2 percent, yielding a Medicare-allowable depreciation cost weight (excluding leasing expenses, which is described in more detail below) of 2.1 percent. To further disaggregate the Medicare-allowable depreciation cost weight into fixed and moveable depreciation, we proposed to use the 2018 SNF MCR data for end-of-the-year capital asset balances as reported on Worksheet A-7. The 2018 SNF MCR data showed a fixed/moveable split of 86/14. The 2014-based SNF market basket, which utilized the same data from the 2014 MCRs, had a fixed/moveable split of 83/17.
We also derived the interest expense share of capital-related expenses from 2018 SNF MCR data, specifically from Worksheet A, column 2, line 81. Similar to the depreciation cost weight, we calculated the interest cost weight using total facility capital costs. This methodology yielded interest costs as a percent of capital costs of 22.8 percent for 2018. We then apply this percentage to the 2018-based SNF market basket Medicare-allowable Capital-related cost weight of 8.2 percent, yielding a Medicare-allowable interest cost weight (excluding leasing expenses) of 1.9 percent. As done with the last rebasing (82 FR 36556), we proposed to determine the split of interest expense between for-profit and not-for-profit facilities based on the distribution of long-term debt outstanding by type of SNF (for-profit or not-for-profit/government) from the 2018 SNF MCR data. We estimated the split between for-profit and not-for-profit interest expense to be 25/75 percent compared to the 2014-based SNF market basket with 27/73 percent.
Because the detailed data were not available in the MCRs, we used the most recent 2017 Census Bureau Service Annual Survey (SAS) data to derive the capital-related expenses attributable to leasing and other capital-related expenses. The 2014-based SNF market basket used the 2014 SAS data. We note that we proposed to use the 2017 SAS data because the Census Bureau no longer publishes these detailed capital-related expenses effective for 2018.
Based on the 2017 SAS data, we determined that leasing expenses are 62 percent of total leasing and capital-related expenses costs. In the 2014-based SNF market basket, leasing costs represent 63 percent of total leasing and capital-related expenses costs. We then apply this percentage to the 2018-based SNF market basket residual Medicare-allowable capital costs of 4.2 percent derived from subtracting the Medicare-allowable depreciation cost weight and Medicare-allowable interest cost weight from the 2018-based SNF market basket of total Medicare-allowable capital cost weight (8.2 percent−2.1 percent−1.9 percent = 4.2 percent). This produces the 2018-based SNF Medicare-allowable leasing cost weight of 2.6 percent and all-other capital-related cost weight of 1.6 percent.
Lease expenses are not broken out as a separate cost category in the SNF market basket, but are distributed among the cost categories of depreciation, interest, and other capital-related expenses, reflecting the assumption that the underlying cost structure and price movement of leasing expenses is similar to capital costs in general. As was done with past SNF market baskets and other PPS market baskets, we assumed 10 percent of lease expenses are overhead and assigned them to the other capital-related expenses cost category. This is based on the assumption that leasing expenses include not only depreciation, interest, and other capital-related costs but also additional costs paid to the lessor. We distributed the remaining lease expenses to the three cost categories based on the proportion of depreciation, interest, and other capital-related expenses to total capital costs, excluding lease expenses.
Table 14 shows the capital-related expense distribution (including expenses from leases) in the 2018-based SNF market basket and the 2014-based SNF market basket.
Start Printed Page 42451
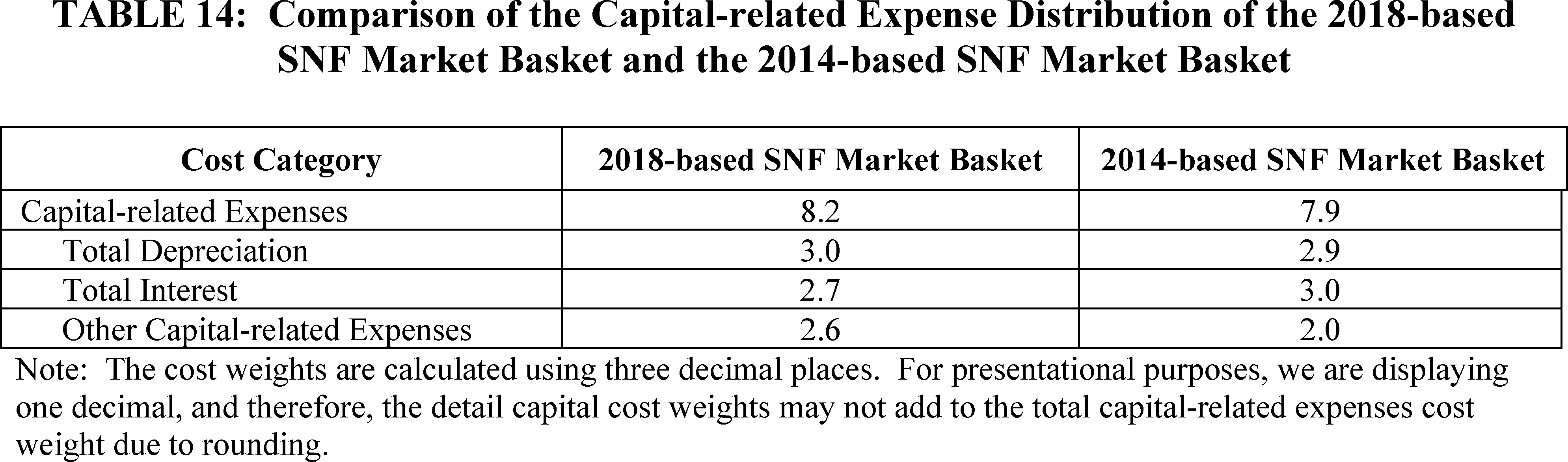
Table 15 presents the 2018-based SNF market basket and the 2014-based SNF market basket.
Start Printed Page 42452

2. Price Proxies Used To Measure Operating Cost Category Growth
After developing the 27 cost weights for the 2018-based SNF market basket, we selected the most appropriate wage and price proxies currently available to represent the rate of change for each expenditure category. With four Start Printed Page 42453 exceptions (three for the capital-related expenses cost categories and one for PLI), we base the wage and price proxies on Bureau of Labor Statistics (BLS) data, and group them into one of the following BLS categories:
- Employment Cost Indexes. Employment Cost Indexes (ECIs) measure the rate of change in employment wage rates and employer costs for employee benefits per hour worked. These indexes are fixed-weight indexes and strictly measure the change in wage rates and employee benefits per hour. ECIs are superior to Average Hourly Earnings (AHE) as price proxies for input price indexes because they are not affected by shifts in occupation or industry mix, and because they measure pure price change and are available by both occupational group and by industry. The industry ECIs are based on the 2012 NAICS and the occupational ECIs are based on the 2000 and 2010 Standard Occupational Classification System (SOC).
- Producer Price Indexes. Producer Price Indexes (PPIs) measure the average change over time in the selling prices received by domestic producers for their output. The prices included in the PPI are from the first commercial transaction for many products and some services (https://www.bls.gov/ppi/).
- Consumer Price Indexes. Consumer Price Indexes (CPIs) measure the average change over time in the prices paid by urban consumers for a market basket of consumer goods and services (https://www.bls.gov/cpi/). CPIs are only used when the purchases are similar to those of retail consumers rather than purchases at the producer level, or if no appropriate PPIs are available.
We evaluated the price proxies using the criteria of reliability, timeliness, availability, and relevance. Reliability indicates that the index is based on valid statistical methods and has low sampling variability. Widely accepted statistical methods ensure that the data were collected and aggregated in a way that can be replicated. Low sampling variability is desirable because it indicates that the sample reflects the typical members of the population. (Sampling variability is variation that occurs by chance because only a sample was surveyed rather than the entire population.) Timeliness implies that the proxy is published regularly, preferably at least once a quarter. The market baskets are updated quarterly, and therefore, it is important for the underlying price proxies to be up-to-date, reflecting the most recent data available. We believe that using proxies that are published regularly (at least quarterly, whenever possible) helps to ensure that we are using the most recent data available to update the market basket. We strive to use publications that are disseminated frequently, because we believe that this is an optimal way to stay abreast of the most current data available. Availability means that the proxy is publicly available. We prefer that our proxies are publicly available because this will help ensure that our market basket updates are as transparent to the public as possible. In addition, this enables the public to be able to obtain the price proxy data on a regular basis. Finally, relevance means that the proxy is applicable and representative of the cost category weight to which it is applied. The CPIs, PPIs, and ECIs that we have proposed meet these criteria. Therefore, we believe that they continue to be the best measure of price changes for the cost categories to which they would be applied.
Table 20 lists all price proxies for the 2018-based SNF market basket. Below is a detailed explanation of the price proxies used for each operating cost category.
- Wages and Salaries: We proposed to use the ECI for Wages and Salaries for Private Industry Workers in Nursing Care Facilities (NAICS 6231; BLS series code CIU2026231000000I) to measure price growth of this category. NAICS 623 includes facilities that provide a mix of health and social services, with many of the health services being largely some level of nursing services. Within NAICS 623 is NAICS 6231, which includes nursing care facilities primarily engaged in providing inpatient nursing and rehabilitative services. These facilities, which are most comparable to Medicare-certified SNFs, provide skilled nursing and continuous personal care services for an extended period of time, and therefore, have a permanent core staff of registered or licensed practical nurses. This is the same index used in the 2014-based SNF market basket.
- Employee Benefits: We proposed to use the ECI for Benefits for Nursing Care Facilities (NAICS 6231) to measure price growth of this category. The ECI for Benefits for Nursing Care Facilities is calculated using BLS's total compensation (BLS series ID CIU2016231000000I) for nursing care facilities series and the relative importance of wages and salaries within total compensation. We believe this constructed ECI series is technically appropriate for the reason stated above in the Wages and Salaries price proxy section. This is the same index used in the 2014-based SNF market basket.
- Electricity and Other Non-Fuel Utilities: We proposed to use the PPI Commodity for Commercial Electric Power (BLS series code WPU0542) to measure the price growth of this cost category as Electricity costs account for 93 percent of these expenses. This is the same index used for the Electricity cost category in the 2014-based SNF market basket. As previously noted, we proposed to include Water and Sewerage costs within the Electricity and Other Non-Fuel Utilities cost category, and to no longer use the CPI All Urban for Water and Sewerage Maintenance as we did for the 2014-based SNF market basket, due to the small size of this estimated cost weight (less than 0.1 percent).
Comment: One commenter noted that CMS is proposing to include water and sewerage costs in the Electricity and Other Non-Fuel utilities cost weight and to no longer use the CPI All Urban for Water and Sewerage Maintenance. They expressed concern stating that many SNFs have invested in waste-water monitoring systems as a result of COVID-19.
Response: We recognize the commenter's concern but as stated above, the most recent year of Benchmark I-O data we have available to derive the detailed cost weights for the SNF market basket is 2012, with the data generally scheduled for publication every 5 years. Based on these data, the cost weight associated with Water and Sewerage costs is less than 0.1 percent, and therefore, we do not believe a separate cost category is appropriate. We will continue to monitor new data for SNFs as it becomes available, including any new Benchmark I-O data, and will propose a rebasing or revising of the SNF market basket cost weights as appropriate.
- Fuel: Oil and Gas: We proposed to change the proxy used for the Fuel: Oil and Gas cost category. Our analysis of the Bureau of Economic Analysis' 2012 Benchmark I-O data for Nursing and Community Care Facilities shows approximately 96 percent of SNF Fuel: Oil and Gas expenses are for Petroleum Refineries (NAICS 324110), Natural gas (NAICS 221200), and Other Petroleum and Coal Products Manufacturing (NAICS 324190). We proposed to create a blended index based on those three NAICS chemical expenses listed above that account for 96 percent of SNF chemical expenses. We proposed to create this blend based on each NAICS' expenses as a share of their sum. Therefore, we proposed a blended proxy of 61 percent of the PPI Industry for Petroleum Refineries (BLS series code PCU32411-32411), 7 percent of the PPI Start Printed Page 42454 Commodity for Natural Gas (BLS series code WPU0531), and 32 percent of the PPI for Other Petroleum and Coal Products manufacturing (BLS series code PCU32419-32419).
The 2014-based SNF market basket also used a blended chemical proxy that was based on 2007 Benchmark I-O data. We believe our proposed Fuel: Oil and Gas blended index for the 2018-based SNF market basket is technically appropriate as it reflects more recent data on SNFs purchasing patterns. Table 16 provides the weights for the 2018-based blended chemical index and the 2014-based blended chemical index.

- Professional Liability Insurance: We proposed to use the CMS Hospital Professional Liability Insurance Index to measure price growth of this category. We were unable to find a reliable data source that collects SNF-specific PLI data. Therefore, we proposed to use the CMS Hospital Professional Liability Index, which tracks price changes for commercial insurance premiums for a fixed level of coverage, holding non-price factors constant (such as a change in the level of coverage). This is the same index used in the 2014-based SNF market basket. We believe this is an appropriate proxy to measure the price growth associated of SNF PLI as it captures the price inflation associated with other medical institutions that serve Medicare patients.
- Pharmaceuticals: We proposed to use the PPI Commodity for Pharmaceuticals for Human Use, Prescription (BLS series code WPUSI07003) to measure the price growth of this cost category. This is the same index used in the 2014-based SNF market basket.
- Food: Wholesale Purchases: We proposed to use the PPI Commodity for Processed Foods and Feeds (BLS series code WPU02) to measure the price growth of this cost category. This is the same index used in the 2014-based SNF market basket.
- Food: Retail Purchase: We proposed to use the CPI All Urban for Food Away From Home (All Urban Consumers) (BLS series code CUUR0000SEFV) to measure the price growth of this cost category. This is the same index used in the 2014-based SNF market basket.
- Chemicals: For measuring price change in the Chemicals cost category, we proposed to use a blended PPI composed of the Industry PPIs for Other Basic Organic Chemical Manufacturing (NAICS 325190) (BLS series code PCU32519-32519), Soap and Cleaning Compound Manufacturing (NAICS 325610) (BLS series code PCU32561-32561), and Other Miscellaneous Chemical Product Manufacturing (NAICS 325998) (BLS series code PCU325998325998).
Using the 2012 Benchmark I-O data, we found that these three NAICS industries accounted for approximately 96 percent of SNF chemical expenses. The remaining 4 percent of SNF chemical expenses are for three other incidental NAICS chemicals industries such as Paint and Coating Manufacturing. We proposed to create a blended index based on those three NAICS chemical expenses listed above that account for 96 percent of SNF chemical expenses. We proposed to create this blend based on each NAICS' expenses as a share of their sum. These expenses as a share of their sum are listed in Table 17.
The 2014-based SNF market basket also used a blended chemical proxy that was based on 2007 Benchmark I-O data. We believe our proposed chemical blended index for the 2018-based SNF market basket is technically appropriate as it reflects more recent data on SNFs purchasing patterns. Table 17 provides the weights for the 2018-based blended chemical index and the 2014-based blended chemical index.

- Medical Instruments and Supplies: We proposed to change the proxy used for the Medical Instruments and Supplies cost weight. The 2012 Benchmark I-O data shows 46 percent of medical instruments and supply costs are for Surgical and medical instrument manufacturing costs (NAICS 339112) and 54 percent are for Surgical appliance and supplies manufacturing costs (NAICS 339113). To proxy the price changes associated with NAICS 339112, we proposed using the PPI—Commodity—Surgical and medical instruments (BLS series code WPU1562). This the same price proxy we used in the 2014-based SNF market basket. To proxy the price changes associated with NAICS 339113, we proposed to use 50 percent for the PPI—Commodity—Medical and surgical Start Printed Page 42455 appliances and supplies (BLS series code WPU1563) and 50 percent for the PPI Commodity data for Miscellaneous products-Personal safety equipment and clothing (BLS series code WPU1571). The latter price proxy would reflect personal protective equipment including but not limited to face shields and protective clothing. The 2012 Benchmark I-O data does not provide specific expenses for personal protective equipment (which would be reflected in the NAICS 339113 expenses); however, we recognize that this category reflects costs faced by SNFs. In absence of any specific cost data on personal protective equipment, we proposed to include the PPI Commodity data for Miscellaneous products-Personal safety equipment and clothing (BLS series code WPU1571) in the blended proxy for Medical Instruments and Supplies cost category with a weight of 27 percent (that is, 50 percent of the NAICS 339113 expenses as a percent of the sum of NAICS 339113 and NAICS 339112 expenses from the I-O).
The 2014-based SNF market basket used a blend composed of 60 percent of the PPI Commodity for Medical and Surgical Appliances and Supplies (BLS series code WPU1563) and 40 percent of the PPI Commodity for Surgical and Medical Instruments (BLS series code WPU1562). Table 18 provides the proposed Medical Instruments and Supplies cost weight blended price proxy.

Comment: One commenter appreciated CMS' proposal to modify the Medical Instruments and Supplies proxy to reflect personal protective equipment.
Response: We appreciate the commenter's support and recognize the need to reflect the prices of medical instruments and supplies purchased by SNFs.
- Rubber and Plastics: We proposed to use the PPI Commodity for Rubber and Plastic Products (BLS series code WPU07) to measure price growth of this cost category. This is the same index used in the 2014-based SNF market basket.
- Paper and Printing Products: We proposed to use the PPI Commodity for Converted Paper and Paperboard Products (BLS series code WPU0915) to measure the price growth of this cost category. This is the same index used in the 2014-based SNF market basket.
- Apparel: We proposed to use the PPI Commodity for Apparel (BLS series code WPU0381) to measure the price growth of this cost category. This is the same index used in the 2014-based SNF market basket.
- Machinery and Equipment: We proposed to use the PPI Commodity for Machinery and Equipment (BLS series code WPU11) to measure the price growth of this cost category. This is the same index used in the 2014-based SNF market basket.
- Miscellaneous Products: For measuring price change in the Miscellaneous Products cost category, we proposed to use the PPI Commodity for Finished Goods less Food and Energy (BLS series code WPUFD4131). Both food and energy are already adequately represented in separate cost categories and should not also be reflected in this cost category. This is the same index used in the 2014-based SNF market basket.
- Professional Fees: Labor-Related: We proposed to use the ECI for Total Compensation for Private Industry Workers in Professional and Related (BLS series code CIU2010000120000I) to measure the price growth of this category. This is the same index used in the 2014-based SNF market basket.
- Administrative and Facilities Support Services: We proposed to use the ECI for Total Compensation for Private Industry Workers in Office and Administrative Support (BLS series code CIU2010000220000I) to measure the price growth of this category. This is the same index used in the 2014-based SNF market basket.
- Installation, Maintenance and Repair Services: We proposed to use the ECI for Total Compensation for All Civilian Workers in Installation, Maintenance, and Repair (BLS series code CIU1010000430000I) to measure the price growth of this new cost category. This is the same index used in the 2014-based SNF market basket.
- All Other: Labor-Related Services: We proposed to use the ECI for Total Compensation for Private Industry Workers in Service Occupations (BLS series code CIU2010000300000I) to measure the price growth of this cost category. This is the same index used in the 2014-based SNF market basket.
- Professional Fees: NonLabor-Related: We proposed to use the ECI for Total Compensation for Private Industry Workers in Professional and Related (BLS series code CIU2010000120000I) to measure the price growth of this category. This is the same index used in the 2014-based SNF market basket.
- Financial Services: We proposed to use the ECI for Total Compensation for Private Industry Workers in Financial Activities (BLS series code CIU201520A000000I) to measure the price growth of this cost category. This is the same index used in the 2014-based SNF market basket.
- Telephone Services: We proposed to use the CPI All Urban for Telephone Services (BLS series code CUUR0000SEED) to measure the price growth of this cost category. This is the same index used in the 2014-based SNF market basket.
- All Other: NonLabor-Related Services: We proposed to use the CPI All Urban for All Items Less Food and Energy (BLS series code CUUR0000SA0L1E) to measure the price growth of this cost category. This is the same index used in the 2014-based SNF market basket. As previously noted, we proposed to include Postage costs within the All Other: NonLabor-Related Services cost category, and to no Start Printed Page 42456 longer use the CPI All Urban for Postage as we did for the 2014-based SNF market basket, due to the small size of this estimated cost weight (less than 0.1 percent).
3. Price Proxies Used To Measure Capital Cost Category Growth
We proposed to apply the same capital price proxies as were used in the 2014-based SNF market basket, with the exception of the For-profit interest cost category, and below is a detailed explanation of the price proxies used for each capital cost category. We also proposed to continue to vintage weight the capital price proxies for Depreciation and Interest to capture the long-term consumption of capital. This vintage weighting method is the same method that was used for the 2014-based SNF market basket and is described below.
- Depreciation—Building and Fixed Equipment: We proposed to use the BEA Chained Price Index for Private Fixed Investment in Structures, Nonresidential, Hospitals and Special Care (BEA Table 5.4.4. Price Indexes for Private Fixed Investment in Structures by Type). This BEA index is intended to capture prices for construction of facilities such as hospitals, nursing homes, hospices, and rehabilitation centers. This is the same index used in the 2014-based SNF market basket.
- Depreciation—Movable Equipment: We proposed to use the PPI Commodity for Machinery and Equipment (BLS series code WPU11). This price index reflects price inflation associated with a variety of machinery and equipment that would be utilized by SNFs, including but not limited to medical equipment, communication equipment, and computers. This is the same index used in the 2014-based SNF market basket.
- Nonprofit Interest: We proposed to use the average yield on Municipal Bonds (Bond Buyer 20-bond index). This is the same index used in the 2014-based SNF market basket.
- For-Profit Interest: For the For-Profit Interest cost category, we proposed to use the iBoxx AAA Corporate Bond Yield index instead of the Moody's AAA Corporate Bond Yield index that was used for the 2014-based SNF market basket. Effective for December 2020, the Moody's AAA Corporate Bond series is no longer available for use under license to IGI, the nationally-recognized economic and financial forecasting firm with whom we contract to forecast the components of the market baskets and MFP. Therefore, we proposed to replace the price proxy for the For-Profit interest cost category. We compared the iBoxx AAA Corporate Bond Yield index with the Moody's AAA Corporate Bond Yield index and found that the average growth rates in the two series were similar. Over the historical time period of FY 2000 to FY 2020, the 4-quarter percent change moving average growth in the iBoxx series was approximately 0.1 percentage point higher, on average, than the Moody's AAA corporate Bond Yield index.
- Other Capital: Since this category includes fees for insurances, taxes, and other capital-related costs, we proposed to use the CPI for Rent of Primary Residence (BLS series code CUUS0000SEHA), which would reflect the price growth of these costs. This is the same index used in the 2014-based SNF market basket.
We believe that these price proxies are the most appropriate proxies for SNF capital costs that meet our selection criteria of relevance, timeliness, availability, and reliability.
As stated above, we proposed to continue to vintage weight the capital price proxies for Depreciation and Interest to capture the long-term consumption of capital. To capture the long-term nature, the price proxies are vintage-weighted; and the vintage weights are calculated using a two-step process. First, we determine the expected useful life of capital and debt instruments held by SNFs. Second, we identify the proportion of expenditures within a cost category that is attributable to each individual year over the useful life of the relevant capital assets, or the vintage weights.
We rely on Bureau of Economic Analysis (BEA) fixed asset data to derive the useful lives of both fixed and movable capital, which is the same data source used to derive the useful lives for the 2014-based SNF market basket. The specifics of the data sources used are explained below.
a. Calculating Useful Lives for Moveable and Fixed Assets
Estimates of useful lives for movable and fixed assets for the 2018-based SNF market basket are 9 and 26 years, respectively. These estimates are based on three data sources from the BEA: (1) Current-cost average age; (2) historical-cost average age; and (3) industry-specific current cost net stocks of assets.
BEA current-cost and historical-cost average age data by asset type are not available by industry but are published at the aggregate level for all industries. The BEA does publish current-cost net capital stocks at the detailed asset level for specific industries. There are 64 detailed movable assets (including intellectual property) and there are 32 detailed fixed assets in the BEA estimates. Since we seek aggregate useful life estimates applicable to SNFs, we developed a methodology to approximate movable and fixed asset ages for nursing and residential care services (NAICS 623) using the published BEA data. For the 2018 SNF market basket, we use the current-cost average age for each asset type from the BEA fixed assets Table 2.9 for all assets and weight them using current-cost net stock levels for each of these asset types in the nursing and residential care services industry, NAICS 6230. (For example, nonelectro medical equipment current-cost net stock (accounting for about 35 percent of total moveable equipment current-cost net stock in 2018) is multiplied by an average age of 4.7 years. Current-cost net stock levels are available for download from the BEA website at https://apps.bea.gov/iTable/index_FA.cfm. We then aggregate the "weighted" current-cost net stock levels (average age multiplied by current-cost net stock) into moveable and fixed assets for NAICS 6230. We then adjust the average ages for moveable and fixed assets by the ratio of historical-cost average age (Table 2.10) to current-cost average age (Table 2.9).
This produces historical cost average age data for movable (equipment and intellectual property) and fixed (structures) assets specific to NAICS 6230 of 4.7 and 13.1 years for 2018, respectively. The average age reflects the average age of an asset at a given point in time, whereas we want to estimate a useful life of the asset, which would reflect the average over all periods an asset is used. To do this, we multiply each of the average age estimates by two to convert to average useful lives with the assumption that the average age is normally distributed (about half of the assets are below the average at a given point in time, and half above the average at a given point in time). This produces estimates of likely useful lives of 9.49 and 26.19 years for movable and fixed assets, which we round to 9 and 26 years, respectively. We proposed an interest vintage weight time span of 24 years, obtained by weighting the fixed and movable vintage weights (26 years and 9 years, respectively) by the fixed and movable split (86 percent and 14 percent, respectively). This is the same methodology used for the 2014-based SNF market basket, which had useful lives of 23 years and 10 years for fixed and moveable assets, respectively. We estimate that the impact of revising the Start Printed Page 42457 useful lives had a minor impact on the average historical growth rate of the 2018-based SNF market basket total aggregate capital cost price proxy. Over the FY 2016 to FY 2020 time period, the percent change moving average in the total aggregate capital cost price proxy was about 0.06 percentage point higher, on average, based on the 2018-based SNF market basket compared to the 2014-based SNF market basket.
b. Constructing Vintage Weights
Given the expected useful life of capital (fixed and moveable assets) and debt instruments, we must determine the proportion of capital expenditures attributable to each year of the expected useful life for each of the three asset types: Building and fixed equipment, moveable equipment, and interest. These proportions represent the vintage weights. We were not able to find a historical time series of capital expenditures by SNFs. Therefore, we approximated the capital expenditure patterns of SNFs over time, using alternative SNF data sources. For building and fixed equipment, we used the stock of beds in nursing homes from the National Nursing Home Survey (NNHS) conducted by the National Center for Health Statistics (NCHS) for 1962 through 1999. For 2000 through 2010, we extrapolated the 1999 bed data forward using a 5-year moving average of growth in the number of beds from the SNF MCR data. For 2011 to 2014, we extrapolate the 2010 bed data forward using the average growth in the number of beds over the 2011 to 2014 time period. For 2015 to 2018, we proposed to extrapolate the 2014 bed data forward using the average growth in the number of beds over the 2015 to 2018 time period. We then used the change in the stock of beds each year to approximate building and fixed equipment purchases for that year. This procedure assumes that bed growth reflects the growth in capital-related costs in SNFs for building and fixed equipment. We believe that this assumption is reasonable because the number of beds reflects the size of a SNF, and as a SNF adds beds, it also likely adds fixed capital.
As was done for the 2014-based SNF market basket (as well as prior market baskets), we proposed to estimate moveable equipment purchases based on the ratio of ancillary costs to routine costs. The time series of the ratio of ancillary costs to routine costs for SNFs measures changes in intensity in SNF services, which are assumed to be associated with movable equipment purchase patterns. The assumption here is that as ancillary costs increase compared to routine costs, the SNF caseload becomes more complex and would require more movable equipment. The lack of movable equipment purchase data for SNFs over time required us to use alternative SNF data sources. A more detailed discussion of this methodology was published in the FY 2008 SNF final rule (72 FR 43428). We believe the resulting two time series, determined from beds and the ratio of ancillary to routine costs, reflect real capital purchases of building and fixed equipment and movable equipment over time.
To obtain nominal purchases, which are used to determine the vintage weights for interest, we converted the two real capital purchase series from 1963 through 2018 determined above to nominal capital purchase series using their respective price proxies (the BEA Chained Price Index for Nonresidential Construction for Hospitals & Special Care Facilities and the PPI for Machinery and Equipment). We then combined the two nominal series into one nominal capital purchase series for 1963 through 2018. Nominal capital purchases are needed for interest vintage weights to capture the value of debt instruments.
Once we created these capital purchase time series for 1963 through 2018, we averaged different periods to obtain an average capital purchase pattern over time: (1) For building and fixed equipment, we averaged 31, 26-year periods; (2) for movable equipment, we averaged 48, 9-year periods; and (3) for interest, we averaged 33, 24-year periods. We calculate the vintage weight for a given year by dividing the capital purchase amount in any given year by the total amount of purchases during the expected useful life of the equipment or debt instrument. To provide greater transparency, we posted on the CMS market basket website at http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MedicareProgramRatesStats/MarketBasketResearch.html, an illustrative spreadsheet that contains an example of how the vintage-weighted price indexes are calculated.
The vintage weights for the 2018-based SNF market basket and the 2014-based SNF market basket are presented in Table 19.
Start Printed Page 42458
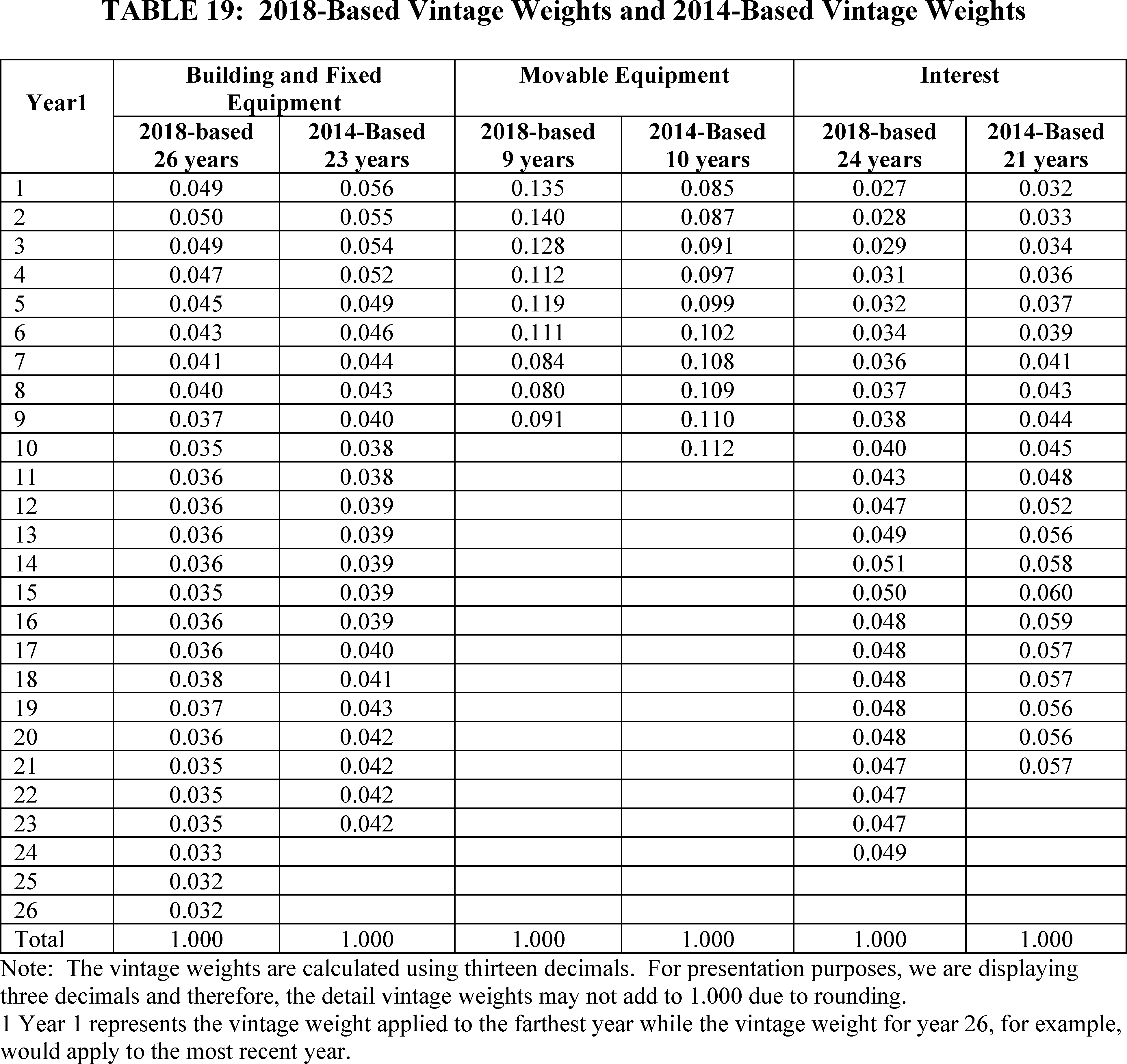
Comment: Many commenters stated that COVID-19 has required SNFs to make significant changes in operations resulting in much higher operating costs as a result of increased labor, PPE, janitorial, and capital costs. They stated the new cost levels were permanent and noted that the 2018 data used to rebase the market basket would not reflect these cost levels. They recommended CMS account for these increased costs in the market basket.
Several commenters requested that CMS explore the temporary use of more heavily-weighted market basket elements to account for COVID-19 influenced cost increases, especially for both in-house and contract labor costs and capital costs. To account for the change in labor costs, some commenters recommended that CMS make an adjustment to the labor-related price proxy to account for the increase in wages and salaries and contract labor costs. One commenter recommended that CMS use the Payroll-Based Journal (PBJ) data and examine the wage rate differential between Agency and Employed Nurses/Aides using the labor data reported on Schedule S-3 Part V of the SNF Medicare cost reports. The commenter recommended that the greater proportion of Agency staff in the PBJ data when combined with the price differential between Employed vs Agency staff would result in an increase in the price proxy for labor (with labor being roughly 70 percent of costs).
One commenter listed testing of staff as one of the largest unbudgeted and unreimbursed costs for nursing homes. They stated that staff testing costs vary widely based on the size of the facility, types of tests used, and laboratory charges and on average have cost about 100 per week per staff member tested. Some commenters stated that some PPE allotments were provided by state and local governments; however, the amounts were inconsequential in comparison with the needs. Some commenters further requested that CMS consider additional under-detected costs due to room-sharing by more than one COVID-19 positive patient which was required by space constraints and/or isolation room shortages.
One commenter also recommended CMS inflate the capital costs noting that SNFs have incurred increased costs to reduce the spread of COVID-19 by investing in fresh air intake systems, air purification systems, and new heating ventilation and air conditions systems. They also cited additional costs Start Printed Page 42459 incurred in 2020 to invest in improved wireless technology and ultraviolet light. One commenter suggested that the capital costs should also reflect the increased costs of replacing and/or updating older facilities and the construction of larger facilities which would better position nursing facilities for any future pandemic situations.
Response: We appreciate the commenter's concern regarding the impact of COVID-19 on SNF costs. We reiterate that the SNF market basket is a fixed-weight, Laspeyres-type price index that measures the change in price, over time, of the same mix of goods and services purchased in the base period. Any changes in the quantity or mix of goods and services (that is, intensity) purchased over time relative to a base period are not reflected. Changes in costs are taken into consideration and reflected when the market basket is rebased and the cost weights are revised to reflect the most recent cost structure. CMS proposed to rebase and revise the SNF market basket for FY 2022 since it has been 4 years since the last rebasing. The SNF market basket cost weights rely on the data reported on the Medicare cost reports, which provide the most comprehensive expense data available for the universe of SNFs. We proposed to use the data reported for 2018 because it is the most recent year of complete data available at the time of performing the analysis for the proposed SNF rule.
We understand that the COVID-19 pandemic has resulted in unanticipated challenges to SNF providers and all other healthcare provider settings. We note that the market basket updates account for the expected changes in the input prices, including labor, medical supplies, other products (including PPE), and capital. The price proxies take into account the changes in the expected prices of these good and services. The rates are set prospectively which requires forecasting the expected inflation pressures. The FY 2022 SNF payment update is based on the most recent forecast of expected price pressures that SNF providers will face in FY 2022. Additionally, the SNF payment update formula includes a forecast error adjustment if the difference between the historical SNF market basket growth and projected SNF market basket growth exceeds the forecast error threshold (in absolute terms). As discussed in section IV.B.3 of this final rule, the forecast error for FY 2020 is −0.8 percentage point indicating the SNF market basket update factor was higher than the actual SNF market basket growth. The same analysis will be considered for FY 2021 once historical data is available.
We also note that while the overall operating expenses may have been impacted for providers in 2020, the market basket cost share weights are based on the relative shares of expenses by category. CMS would need to have a dataset that would provide expenditure levels for all categories of expenses to determine the relative shares of each cost category and there is not a comprehensive set of 2020 cost data for SNF providers available at this time. It would be inappropriate to only make adjustments to select costs as suggested by the commenters. As stated previously, we plan to review the 2020 Medicare cost report data as soon as complete information is available to ensure the market basket relative cost shares are still appropriate.
Finally, we respectfully disagree that the capital cost weight in the market basket should reflect future costs of replacing and/or updating older facilities and the construction of larger facilities in order to better position nursing facilities for any future pandemic situations. The market basket cost weights are based on actual expenses that SNF facilities incur and reported on the Medicare cost reports.
After consideration of public comments, we are finalizing the 2018-based SNF market basket as proposed. Table 20 shows all the price proxies for the finalized 2018-based SNF market basket.
Start Printed Page 42460

Start Printed Page 42461

4. Labor-Related Share
We define the labor-related share (LRS) as those expenses that are labor-intensive and vary with, or are influenced by, the local labor market. Each year, we calculate a revised labor-related share based on the relative importance of labor-related cost categories in the input price index. Effective for FY 2022, we proposed to revise and update the labor-related share to reflect the relative importance of the 2018-based SNF market basket cost categories that we believe are labor-intensive and vary with, or are influenced by, the local labor market. For the 2018-based SNF market basket these are: (1) Wages and Salaries (including allocated contract labor costs as described above); (2) Employee Benefits (including allocated contract labor costs as described above); (3) Professional fees: Labor-related; (4) Administrative and Facilities Support Services; (5) Installation, Maintenance, and Repair Services; (6) All Other: Labor-Related Services; and (7) a proportion of capital-related expenses. We proposed to continue to include a proportion of capital-related expenses because a portion of these expenses are deemed to be labor-intensive and vary with, or are influenced by, the local labor market. For example, a proportion of construction costs for a medical building would be attributable to local construction workers' compensation expenses.
Consistent with previous SNF market basket revisions and rebasings, the All Other: Labor-related services cost category is mostly comprised of building maintenance and security services (including, but not limited to, landscaping services, janitorial services, waste management services services) and dry cleaning and laundry services. Because these services tend to be labor-intensive and are mostly performed at the SNF facility or in the local area (and therefore, unlikely to be purchased in the national market), we believe that they meet our definition of labor-related services.
These are the same cost categories we have included in the LRS for the 2014-based SNF market basket rebasing (82 FR 36563), as well as the same categories included in the LRS for the 2016-based IRF market basket (84 FR 39087), 2016-based IPF market basket Start Printed Page 42462 (84 FR 38445), and 2017-based LTCH market basket (85 FR 58910).
As discussed in the FY 2018 SNF PPS proposed rule (82 FR 21040), in an effort to determine more accurately the share of nonmedical professional fees (included in the 2018-based SNF market basket Professional Fees cost categories) that should be included in the labor-related share, we surveyed SNFs regarding the proportion of those fees that are attributable to local firms and the proportion that are purchased from national firms. Based on these weighted results, we determined that SNFs purchase, on average, the following portions of contracted professional services inside their local labor market:
- 78 percent of legal services.
- 86 percent of accounting and auditing services.
- 89 percent of architectural, engineering services.
- 87 percent of management consulting services.
Together, these four categories represent 3.5 percentage points of the total costs for the 2018-based SNF market basket. We applied the percentages from this special survey to their respective SNF market basket weights to separate them into labor-related and nonlabor-related costs. As a result, we are designating 2.9 of the 3.5 percentage points total to the labor-related share, with the remaining 0.6 percentage point categorized as nonlabor-related.
In addition to the professional services as previously listed, for the 2018-based SNF market basket, we proposed to allocate a proportion of the Home Office/Related Organization Contract Labor cost weight, calculated using the Medicare cost reports as previously stated, into the Professional Fees: Labor-related and Professional Fees: Nonlabor-related cost categories. We proposed to classify these expenses as labor-related and nonlabor-related as many facilities are not located in the same geographic area as their home office, and therefore, do not meet our definition for the labor-related share that requires the services to be purchased in the local labor market.
Similar to the 2014-based SNF market basket, we proposed for the 2018-based SNF market basket to use the Medicare cost reports for SNFs to determine the home office labor-related percentages. The Medicare cost report requires a SNF to report information regarding its home office provider. Using information on the Medicare cost report, we compared the location of the SNF with the location of the SNF's home office. We proposed to classify a SNF with a home office located in their respective labor market if the SNF and its home office are located in the same Metropolitan Statistical Area (MSA). Then we determine the proportion of the Home Office/Related Organization Contract Labor cost weight that should be allocated to the labor-related share based on the percent of total Home Office/Related Organization Contract Labor costs for those SNFs that had home offices located in their respective local labor markets of total Home Office/Related Organization Contract Labor costs for SNFs with a home office. We determined a SNF's and its home office's MSA using their zip code information from the Medicare cost report. Using this methodology, we determined that 21 percent of SNFs' Home Office/Related Organization Contract Labor costs were for home offices located in their respective local labor markets. Therefore, we proposed to allocate 21 percent of the Home Office/Related Organization Contract Labor cost weight (0.14 percentage point = 0.69 percent × 21 percent) to the Professional Fees: Labor-related cost weight and 79 percent of the Home Office/Related Organization Contract Labor cost weight to the Professional Fees: Nonlabor-related cost weight (0.55 percentage point = 0.69 percent × 79 percent). The 2014-based SNF market basket used a similar methodology for allocating the Home Office/Related Organization Contract Labor cost weight to the labor-related share.
In summary, based on the two allocations mentioned earlier, we proposed to apportion 3.0 percentage points of the Professional Fees (2.9 percentage points) and Home Office/Related Organization Contract Labor (0.1 percentage point) cost weights into the Professional Fees: Labor-Related cost category. This amount was added to the portion of professional fees that we already identified as labor-related using the I-O data such as contracted advertising and marketing costs (approximately 0.45 percentage point of total costs) resulting in a Professional Fees: Labor-Related cost weight of 3.5 percent.
Based on IHS Global Inc. 2020q4 forecast with historical data thrugh 2020q3, we proposed a FY 2022 labor-related share of 70.1 percent (86 FR 19965).
Comment: A few commenters appreciated the reduction of the labor-related share from 71.3 percent to 70.1 percent for FY 2022.
Response: We appreciate the commenters' support. We believe that updating the labor-related share to reflect the more recent data of the 2018-based SNF market basket is appropriate to ensuring accurate payments to SNF providers.
Comment: One commenter urged CMS to reverse the decrease in the labor-related share from 71.3 percent to 70.1 percent in FY 2022. The commenter stated that a lower labor share does not reflect the experiences of SNFs during the PHE. They stated that SNFs face difficulty hiring and maintaining staff and to keep pace with labor shortages and also claim that average salary costs have increased over 2020.
Response: We disagree with the commenter's request to not finalize our proposal to determine the labor-related share for FY 2022 based on the proposed 2018-based SNF market basket. We believe that updating the labor share to reflect more recent cost data of the 2018-based SNF market basket is a technical improvement in determining the labor-related share. We also note that the SNF labor-related share is based on the relative importance of the labor-related categories and therefore, accounts for both a change to the base year weights (accounting for total spending) but also accounts for price changes from the base year to the FY 2022 payment period. Therefore, we believe that the LRS based on the 2018-based market basket is a technical improvement. As stated in the FY 2022 SNF PPS proposed rule (86 FR 19959), if more recent data became available (for example, a more recent estimate of the SNF market basket and/or productivity), we would use such data, if appropriate, to determine the FY 2022 SNF market basket percentage change, labor-related share relative importance, forecast error adjustment, or productivity adjustment in the FY 2022 SNF PPS final rule. Based on IGI's 2021q2 forecast (with historical data through 2021q1), the labor-related share of the finalized 2018-based SNF market basket is 70.4 percent.
Table 21 compares the FY 2022 labor-related share based on the 2018-based SNF market basket relative importance and the FY 2021 labor-related share based on the 2014-based SNF market basket relative importance as finalized in the FY 2021 SNF final rule (85 FR 47605).
Start Printed Page 42463

The FY 2022 SNF labor-related share is 0.9 percentage point lower than the FY 2021 SNF labor-related share (based on the 2014-based SNF market basket). The major reason for the lower labor-related share is due to the incorporation of the 2012 Benchmark I-O data, primarily stemming from a decrease in the All Other: Labor-related services and Professional Fees: Labor-related services cost weights, and a decrease in the Compensation cost weight as a result of incorporating the 2018 MCR data.
5. Market Basket Estimate for the FY 2022 SNF PPS Update
As discussed previously, beginning with the FY 2022 SNF PPS update, we are adopting the 2018-based SNF market basket as the appropriate market basket of goods and services for the SNF PPS. Consistent with historical practice, we estimate the market basket update for the SNF PPS based on IHS Global Inc.'s (IGI) forecast. IGI is a nationally recognized economic and financial forecasting firm that contracts with CMS to forecast the components of the market baskets and multifactor productivity (MFP). Based on IGI's second quarter 2021 forecast with historical data through the first quarter of 2021, the most recent estimate of the 2018-based SNF market basket update for FY 2022 is 2.7 percent—which is the same update as the FY 2022 percent change of the 2014-based SNF market basket.
Table 22 compares the 2018-based SNF market basket and the 2014-based SNF market basket percent changes. For the historical period between FY 2017 and FY 2020, there is no difference in the average growth rates between the two market baskets. For the forecasted period between FY 2021 and FY 2023, the average difference in the growth rates between the two market baskets is −0.1 percentage point.
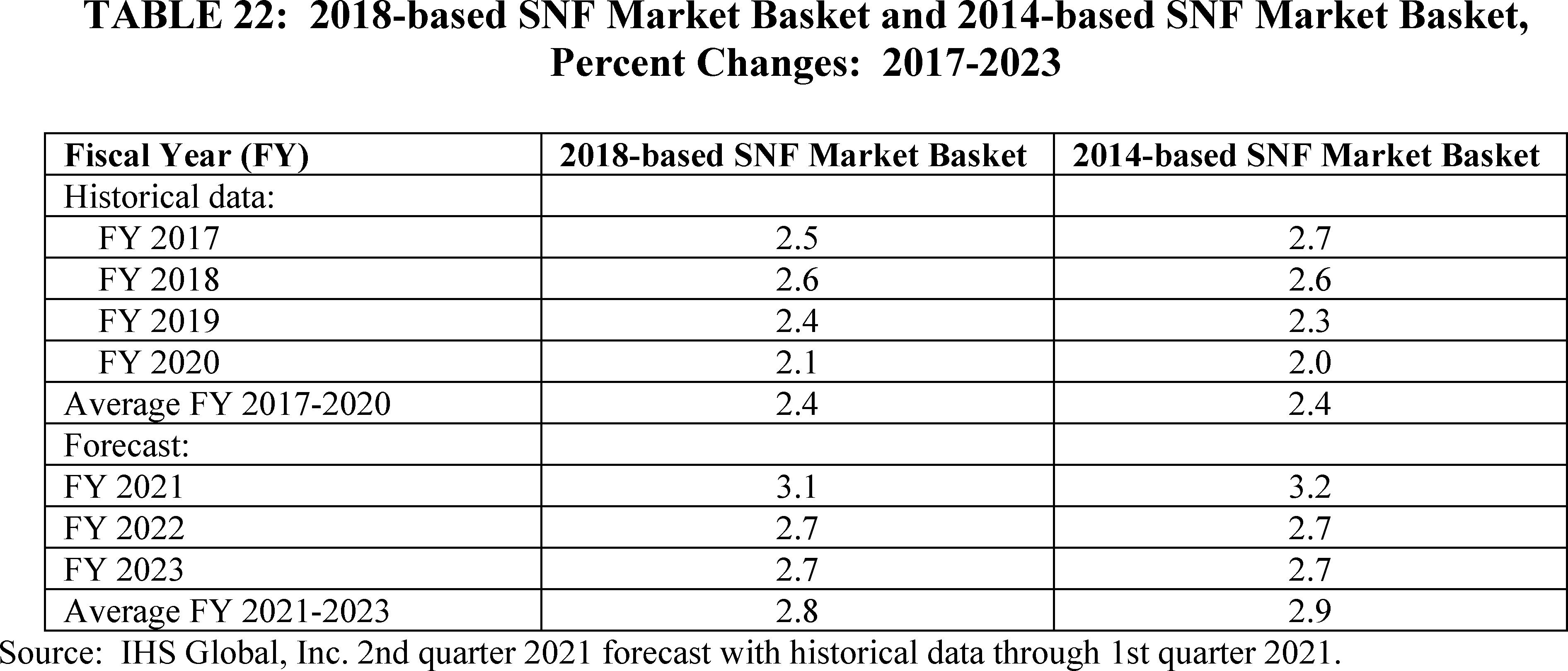
Start Printed Page 42464
B. Technical Updates to PDPM ICD-10 Mappings
In the FY 2019 SNF PPS final rule (83 FR 39162), we finalized the implementation of the Patient Driven Payment Model (PDPM), effective October 1, 2019. The PDPM utilizes International Classification of Diseases, Version 10 (ICD-10) codes in several ways, including to assign patients to clinical categories used for categorization under several PDPM components, specifically the PT, OT, SLP and NTA components. The ICD-10 code mappings and lists used under PDPM are available on the PDPM website at https://www.cms.gov/Medicare/MedicareFee-for-Service-Payment/SNFPPS/PDPM.
Each year, the ICD-10 Coordination and Maintenance Committee, a Federal interdepartmental committee that is chaired by representatives from the National Center for Health Statistics (NCHS) and by representatives from CMS, meets biannually and publishes updates to the ICD-10 medical code data sets in June of each year. These changes become effective October 1 of the year in which these updates are issued by the committee. The ICD-10 Coordination and Maintenance Committee also has the ability to make changes to the ICD-10 medical code data sets effective on April 1.
In the FY 2020 SNF PPS final rule (84 FR 38750), we outlined the process by which we maintain and update the ICD-10 code mappings and lists associated with the PDPM, as well as the SNF GROUPER software and other such products related to patient classification and billing, so as to ensure that they reflect the most up to date codes possible. Beginning with the updates for FY 2020, we apply nonsubstantive changes to the ICD-10 codes included on the PDPM code mappings and lists through a subregulatory process consisting of posting updated code mappings and lists on the PDPM website at https://www.cms.gov/Medicare/Medicare-Fee-for-ServicePayment/SNFPPS/PDPM. Such nonsubstantive changes are limited to those specific changes that are necessary to maintain consistency with the most current ICD-10 medical code data set. On the other hand, substantive changes, or those that go beyond the intention of maintaining consistency with the most current ICD-10 medical code data set, will be proposed through notice and comment rulemaking. For instance, changes to the assignment of a code to a comorbidity list or other changes that amount to changes in policy are considered substantive changes for which we would undergo notice and comment rulemaking.
This year's proposed rule (86 FR 19984-19985) proposed several changes to the PDPM ICD-10 code mappings and lists. We proposed the following changes:
On October 1, 2020 two ICD-10 codes representing types of sickle-cell disease; D57.42 "Sickle-cell thalassemia beta zero without crisis" and D57.44 "Sickle-cell thalassemia beta plus without crisis" took effect and were clinically mapped to the category of "Medical Management". However, there are more specific codes to indicate why a patient with sickle-cell disease would require SNF care, and if the patient is not in crisis, this most likely indicates that SNF care is not required. For this reason, we proposed to change the assignment of D57.42 and D57.44 to "Return to Provider".
On October 1, 2020, three new ICD-10 codes representing types of esophageal conditions; K20.81 "Other esophagitis with bleeding", K20.91, "Esophagitis, unspecified with bleeding, and K21.01 "Gastro-esophageal reflux disease with esophagitis, with bleeding" took effect and were clinically mapped to "Return to Provider". Upon review of these codes, we recognize that these codes represent these esophageal conditions with more specificity than originally considered because of the bleeding that is part of the conditions and that they would more likely be found in SNF patients. Therefore, we proposed to change the assignment of K20.81, K20.91, and K21.01 to "Medical Management" in order to promote more accurate clinical category assignment.
In December 2020, the CDC announced several additions to the ICD-10 Classification related to COVID-19 that became effective on January 1, 2021. One such code, M35.81 "Multisystem inflammatory syndrome", was assigned to "Non-Surgical Orthopedic/Musculoskeletal". However, Multisystem inflammatory syndrome can involve more than the musculoskeletal system. It can also involve the gastrointestinal tract, heart, central nervous system, and kidneys. For this reason, we proposed to change the assignment of M35.81 to "Medical Management" in order to promote more accurate clinical category assignment.
On October 1, 2020, three new ICD-10 codes representing types of neonatal cerebral infarction were classified as "Return to Provider." These codes were P91.821 "Neonatal cerebral infarction, right side of brain," P91.822, "Neonatal cerebral infarction, left side of brain," and P91.823, "Neonatal cerebral infarction, bilateral." While a neonate is unlikely to be a Medicare beneficiary, this diagnosis could continue to be used later in life hence placing those with this condition in the acute neurologic category. Therefore, we proposed to change the assignment of P91.821, P91.822, and P91.823 to "Acute Neurologic" in order to promote more accurate clinical category assignment.
On April 1, 2020, U07.0, "Vaping-related disorder," took effect and was classified as a "Return to Provider" code because at the time, "Vaping-related disorder" was not considered a code that would be a primary diagnosis during a SNF stay. However, upon further review, we believe that many patients who exhibit this diagnosis require steroids, empiric antibiotics and oxygen for care which could carry over to the post-acute setting. For this reason, we proposed to change the assignment of U07.0 to "Pulmonary" classification in order to promote more accurate clinical category assignment.
In the FY 2021 proposed rule (85 FR 20939), we sought comments on additional substantive and nonsubstantive changes that commenters believed were necessary. We received three comments suggesting several changes to the ICD-10 to clinical category mappings. One of those changes was substantive, requiring notice and comment rulemaking. The commenter suggested that the FY 2020 ICD-10 to clinical category mapping of G93.1 "Anoxic brain damage, not elsewhere classified" be changed to "Acute Neurologic" from "Return to Provider," which we would consider a substantive change. Codes that result in "Return to Provider" are codes that cannot be used in I0020B of the MDS because item I0020B is used to establish the primary medical condition that a patient presents with during a SNF stay. Although some codes are considered "Return to Provider" for payment purposes, they are still used to support the care and services used for secondary and co-morbidity diagnoses. The ICD-10 code, G93.1 was initially clinically mapped to "Return to provider" because "Anoxic brain damage, not elsewhere classified" was non-specific and did not fully describe a patient's deficits and may not have been an acute condition. However, upon further review, our clinicians determined that although this may not be an acute condition, "Anoxic brain damage, not elsewhere classified" would still likely result in a need for SNF care and is similar to conditions such as "Compression of the brain", "Cerebral edema", and "encephalopathy", which are mapped into the "Acute Neurologic" category. Therefore, we proposed to change the Start Printed Page 42465 assignment of G93.1 "Anoxic brain damage, not elsewhere classified" to "Acute Neurologic".
We invited comments on the proposed substantive changes to the ICD-10 code mappings discussed previously, as well as comments on additional substantive and non-substantive changes that commenters believe are necessary.
The following is a summary of the public comments received on the proposed revisions to the Technical Updates to PDPM ICD-10 Mappings and our responses:
Comment: Several commenters stated that they support the overall effort to improve accuracy and clarity within PDPM. One commenter specifically notd their appreciation for the change to the PDPM mapping for G93.1 "Anoxic brain damage, not elsewhere classified" from "Return to provider" to "Acute neurologic". Commenters explained that they treat many patients with this ICD-10 diagnosis and the proposed change would better compensate for these services. Another commenter supported the proposed change to the PDPM mapping for K20.81 "Other esophagitis with bleeding", K20.91, "Esophagitis, unspecified with bleeding, and K21.01 "Gastro-esophageal reflux disease with esophagitis, with bleeding" from "Return to provider" to "Medical management".
Response: We appreciate the positive comments we received that supported our efforts to more accurately map several diagnoses under PDPM. We agree with the comments regarding the remapping of G93.1 to "Acute neurologic" and K20.81 "Other esophagitis with bleeding", K20.91, "Esophagitis, unspecified with bleeding, and K21.01 "Gastro-esophageal reflux disease with esophagitis, with bleeding" to "Medical management' as well as the proposal to remap M35.81 "Multisystem inflammatory syndrome;" P91.821 "Neonatal cerebral infarction, right side of brain;" P91.822 "Neonatal infarction, left side of brain;" P91.823 "Neonatal cerebral infarction, bilateral;" U07.0 "Vaping-related disorder;" and G93.1 "Anoxic brain damage, not elsewhere classified." Like the commenters, we believe that remapping will allow for more accurate payment for these diagnoses.
Comment: One commenter did not support the proposal to change mapping of D57.42 "Sickle-cell thalassemia beta zero without crisis" and D57.44 "Sickle-cell thalassemia beta plus without crisis" from Medical Management to Return to Provider. They stated an understanding that in some cases, there may be a more specific ICD-10 code that may be available, if supported by the physician. However, they stated that residents who have been diagnosed with only D57.42 or D57.44 and not a further specified code may still require a skilled level of care in the SNF for this condition. They stated that since a particular diagnosis, in and of itself, cannot meet the criteria of a skilled level of care, they stated it would be appropriate to continue to map D57.42 and D57.44 to the Medical Management clinical category.
Response: As the commenter explained, a diagnosis, in and of itself, may not meet the criteria of a skilled level of care. We agree with that notion. Therefore, we continue to believe that the diagnosis codes of only D57.42 or D57.44 do not provide enough specific information to be the primary diagnosis used for payment. If there is a symptom or condition that is a result of this diagnosis, that symptom or condition should be coded on the MDS and would be able to be mapped for PDPM payment. We would note that there is no limitation on which ICD-10 diagnoses a provider can include on the MDS 3.0. However, there are specific diagnoses which are more appropriate for PDPM mapping and are used for payment as the primary diagnosis under PDPM.
Comment: One commenter suggested additional changes to the ICD-10 code mappings and comorbidity lists that were outside the scope of this rulemaking. As mentioned previously, this commenter stated their support for changing K20.81, K20.91, and K21.01 from the "Return to Provider" mapping to "Medical Management." This commenter also requested that we also consider remapping the following similar diagnosis codes that frequently require SNF skilled care, from Return to Provider to Medical Management: K22.11 "Ulcer of esophagus with bleeding", K25.0 "Acute gastric ulcer with hemorrhage", K25.1"Acute gastric ulcer with perforation", K25.2 "Acute gastric ulcer with both hemorrhage and perforation", K26.0 "Acute duodenal ulcer with hemorrhage", K26.1 "Acute duodenal ulcer with perforation", K26.2 "Acute duodenal ulcer with both hemmhorage and perforation", K27.0 "Acute peptic ulcer, site unspecified with hemorrhage", K27.1 "Acute peptic ulcer, site unspecified with perforation", K27.2 "Acute peptic ulcer, site unspecified with both hemorrhage and perforation", K28.0 "Acute gastrojejunal ulcer with hemorrhage", K28.1 "Acute gastrojejunal ulcer with perforation", K28.2 "Acute gastrojejunal ulcer with both hemorrhage and perforation", and K29.01 "Acute gastritis with bleeding."
They also requested that we consider remapping M62.81 "Muscle weakness (generalized)" from Return to Provider to Non-orthopedic Surgery with the rationale that frail elderly beneficiaries are often admitted to the SNF following hospitalization for a significant infection (for example, pneumonia, COVID-19, urinary tract infection, other respiratory infection). This commenter explained that there is currently no sequela or late-effects ICD-10 code available when such beneficiaries require skilled nursing and therapy due to the late effects of the resolved infection. The active infection may no longer exist, but muscle weakness is often the primary diagnosis the physician identifies as requiring skilled care for these frail elderly beneficiaries. Additionally, this commenter asked that we consider remapping R62.7 "Adult failure to thrive" from Return to Provider to Medical Management. According to this commenter, physicians often diagnose adult failure to thrive when a resident has been unable to have oral intake sufficient for survival. Typically, this diagnosis is appended when the physician has determined that a feeding tube should be considered to provide sufficient intake for survival. According to the commenter, it would then appropriately become the primary diagnosis for a skilled stay.
Response: We note that the changes suggested by the commenter are outside the scope of this rulemaking, and will not be addressed in this rule. We will further consider the suggested changes to the ICD-10 code mappings and comorbidity lists and may implement them in the future as appropriate. To the extent that such changes are non-substantive, we may issue them in a future subregulatory update if appropriate; however, if such changes are substantive changes, in accordance with the update process established in the FY 2020 SNF PPS final rule, such changes must undergo full notice and comment rulemaking, and thus may be included in future rulemaking. See the discussion of the update process for the ICD-10 code mappings and lists in the FY 2020 SNF PPS final rule (84 FR 38750) for more information.
After considering public comments, we are finalizing the revisions as proposed. Start Printed Page 42466
C. Recalibrating the PDPM Parity Adjustment
1. Background
On October 1, 2019, we implemented the Patient Driven Payment Model (PDPM) under the SNF PPS, a new case-mix classification model that replaced the prior case-mix classification model, the Resource Utilization Groups, Version IV (RUG-IV). As discussed in the FY 2019 SNF PPS final rule (83 FR 39256), as with prior system transitions, we proposed and finalized implementing PDPM in a budget neutral manner. This means that the transition to PDPM, along with the related policies finalized in the FY 2019 SNF PPS final rule, were not intended to result in an increase or decrease in the aggregate amount of Medicare payment to SNFs. We believe ensuring parity is integral to the process of providing "for an appropriate adjustment to account for case mix" that is based on appropriate data in accordance with section 1888(e)(4)(G)(i) of the Act. Section V.I. of the FY 2019 SNF PPS final rule (83 FR 39255 through 39256) discusses the methodology that we used to implement PDPM in a budget neutral manner. Specifically, we multiplied each of the PDPM case-mix indexes (CMI) by an adjustment factor that was calculated by comparing total payments under RUG-IV, using FY 2017 claims and assessment data (the most recent final claims data available at the time), and what we expected total payments would be under the then proposed PDPM based on that same FY 2017 claims and assessment data. In the FY 2020 SNF PPS final rule (84 FR 38734 through 38735), we finalized an updated standardization multiplier and parity adjustment based on FY 2018 claims and assessment data. Through this comparison, and as discussed in the FY 2020 SNF PPS final rule, this analysis resulted in an adjustment factor of 1.46, by which all the PDPM CMIs were multiplied so that total estimated payments under PDPM would be equal to total actual payments under RUG-IV, assuming no changes in the population, provider behavior, and coding. By multiplying each CMI by 1.46, the CMIs were inflated by 46 percent in order to achieve budget neutrality.
A similar type of adjustment was used when we transitioned from RUG-III to RUG-IV in FY 2011. However, as discussed in the FY 2012 SNF PPS final rule (76 FR 48492 through 48500), we observed that once actual RUG-IV utilization data became available, the actual RUG-IV utilization patterns differed significantly from those we had projected using the historical data that grounded the RUG-IV parity adjustment. As a result, in the FY 2012 SNF PPS final rule, we used actual FY 2011 RUG-IV utilization data to recalibrate the RUG-IV parity adjustment. Based on the use of FY 2011 RUG-IV utilization data, we decreased the RUG-IV parity adjustment applied to the nursing CMIs for all RUG-IV therapy groups from an adjustment factor of 61 percent to an adjustment factor of 19.84 percent (while maintaining the original 61 percent total nursing CMI increase for all non-therapy RUG-IV groups). As a result of this recalibration, FY 2012 SNF PPS rates were reduced by 12.5 percent, or $4.47 billion, in order to achieve budget neutrality under RUG-IV prospectively.
Since PDPM implementation, we have closely monitored PDPM utilization data to ascertain, among other things, if the PDPM parity adjustment provided for a budget neutral transition to this new case-mix classification model. Similar to what occurred in FY 2011 with RUG-IV implementation, we have observed significant differences between expected SNF PPS payments and case-mix utilization, based on historical data, and the actual SNF PPS payments and case-mix utilization under PDPM, based on FY 2020 data. As a result, it would appear that rather than simply achieving parity, the FY 2020 parity adjustment may have inadvertently triggered a significant increase in overall payment levels under the SNF PPS. We believed that, based on the data from this initial phase of PDPM, a recalibration of the PDPM parity adjustment may be warranted to ensure that the adjustment serves its intended purpose to make the transition between RUG-IV and PDPM budget neutral.
However, we also acknowledged in the proposed rule that the pandemic-related PHE for COVID-19, which began during the first year of PDPM and has continued into at least part of FY 2021, has had a likely impact on SNF PPS utilization data. Further, following the methodology utilized in calculating the initial parity adjustment, we typically would use claims and assessment data for a given year to classify patients under both the current system and the prior system to compare aggregate payments and determine an appropriate adjustment factor to achieve parity. When we performed a similar recalibration of the RUG-IV parity adjustment, for example, we used data from FY 2011, the first year of RUG-IV implementation, as the basis for recalibrating the RUG-IV parity adjustment. However, in addition to the aforementioned potential issues with the FY 2020 SNF utilization data arising from the PHE for COVID-19, we were concerned that given the significant differences in both patient assessment requirements and payment incentives between RUG-IV and PDPM, using the same methodology we have used in the past to calculate a recalibrated PDPM parity adjustment could lead to a potentially inaccurate recalibration.
As described in the FY 2022 SNF proposed rule, we presented some of the results of our PDPM data monitoring efforts and a potential recalibration methodology intended to address the issues presented above. First, it was important to provide transparency on the observed impacts of PDPM implementation, as we believed there have been significant changes observed in SNF utilization that are tied strictly to PDPM and not the PHE for COVID-19. Second, we wished to make clear why we believed that the typical methodology for recalibrating the parity adjustment may not provide an accurate recalibration under PDPM. Finally, we viewed this as an opportunity to seek comment on a path forward for recalibrating the PDPM parity adjustment to ensure that PDPM is implemented in a budget neutral manner, as intended.
2. FY 2020 Changes in SNF Case-Mix Utilization
FY 2020 was a year of significant change under the SNF PPS. In addition to implementing PDPM, a national PHE for COVID-19 was declared. With the announcement of the PHE for COVID-19, we also announced a number of waivers that impacted SNF operations and the population of Medicare beneficiaries who were able to access the Part A SNF benefit. Most notably, under authority granted us by section 1812(f) of the Act, we issued a waiver of section 1861(i) of the Act, specifically the requirement that in order for a SNF stay to be covered by Medicare, a beneficiary must have a prior inpatient hospital stay of not less than 3 consecutive days before being admitted to the Part A SNF stay. Additionally, this waiver also allowed certain beneficiaries renewed SNF coverage without first having to start a new benefit period. The section 1812(f) waiver, particularly the component that permits beneficiaries to access the Part A SNF benefit without a prior hospitalization, allowed beneficiaries who would not typically be able to access the Part A SNF benefit to receive a Part A covered SNF stay (for example, long term care nursing home patients without any prior hospitalization). A key aspect of our suggested potential methodology for recalibrating the PDPM Start Printed Page 42467 parity adjustment involved parsing out the impact of these waivers and the different population of beneficiaries that had access to the SNF benefit as result of these waivers from the population of beneficiaries that would have been admitted to SNFs subsequent to PDPM implementation without these waivers, as well as differences in the type of care these patients received.
We noted that while the PHE for COVID-19 clearly had impacts on nursing home care protocols and many other aspects of SNF operations, the relevant issue for pursuing a recalibration of the PDPM parity adjustment is whether or not these changes caused the SNF case-mix distribution to be distinctly different from what it would have been were it not for the PHE for COVID-19. In other words, while different people were able to access the Part A SNF benefit than would typically be able to do so, the issue was whether or not the relative percentage of beneficiaries in each PDPM group was different than what those percentages would have been were it not for the PHE for COVID-19 and related waivers. We solicited comments on whether and how stakeholders believed that the PHE for COVID-19 impacted the distribution of patient case-mix.
In the proposed rule, we acknowledged the impact of COVID-19 on SNF utilization data by removing those using a PHE-related waiver and those with a COVID-19 diagnosis from our data set. In FY 2020, only approximately 9.8 percent of SNF stays included a COVID-19 ICD-10 diagnosis code either as a primary or secondary diagnosis, while 15.6 percent of SNF stays utilized a section 1812(f) waiver (with the majority of these cases using the prior hospitalization waiver), as identified by the presence of a "DR" condition code on the SNF claim. As compared to prior years, when approximately 98 percent of SNF beneficiaries had a qualifying prior hospital stay, approximately 87 percent of SNF beneficiaries had a qualifying prior hospitalization in FY 2020. These general statistics are important, as they highlight that while the PHE for COVID-19 certainly impacted many aspects of nursing home operations, the overwhelming majority of SNF beneficiaries entered into Part A SNF stays in FY 2020 as they would have in any other year; that is, without using a PHE-related waiver, with a prior hospitalization, and without a COVID-19 diagnosis.
Our data analysis found that even after removing those using a PHE-related waiver and those with a COVID-19 diagnosis from our data set, the observed inadvertent increase in SNF payments since PDPM was implemented was approximately the same. This finding suggests that the significant changes observed in SNF utilization are tied strictly to PDPM and not the PHE for COVID-19, as the "new" population of SNF beneficiaries (that is, COVID-19 patients and those using a section 1812(f) waiver) did not appear to be the cause of the increase in SNF payments after implementation of PDPM.
Moreover, we presented evidence that PDPM alone impacted certain aspects of SNF patient classification and care provision. For example, through FY 2019, SNF patients received an average of approximately 91 therapy minutes per day. Beginning concurrently with PDPM implementation (and well before the onset of the pandemic), the average number of therapy minutes SNF patients received per day dropped to approximately 62 minutes, a decrease of over 30 percent. Similarly, we also observed an increase in non-individualized modes of therapy provision beginning with PDPM implementation. While the percentage of SNF stays that included concurrent or group therapy was approximately 1 percent for each of these therapy modes prior to FY 2020, these numbers rose to approximately 32 percent and 29 percent, respectively, concurrent with PDPM implementation. Notably, when the PHE for COVID-19 was declared in April 2020, these numbers then dropped to 8 percent and 4 percent, respectively, highlighting an impact of the PHE for COVID-19 on SNF care provision and utilization.
We also noted that while the increases in concurrent and group therapy utilization were anticipated prior to PDPM implementation based on comments on the FY 2019 and FY 2020 SNF PPS proposed rules, we maintain the belief that the unique characteristics and goals of each SNF patient should drive patient care decisions and we did not identify any significant changes in health outcomes for SNF patients due to PDPM implementation. For example, we observed no significant changes in the percentage of stays with falls with major injury, the percentage of stays ending with Stage 2-4 or unstageable pressure ulcers or deep tissue injury, the percentage of stays readmitted to an inpatient hospital setting within 30 days of SNF discharge, or other similar metrics. As we stated in the FY 2020 SNF PPS final rule (84 FR 38748), we believe that financial motives should not override the clinical judgment of a therapist or therapy assistant to provide less than appropriate therapy, and we will continue to monitor these and other metrics to identify any adverse trends accompanying the implementation of PDPM.
These changes in therapy provision highlight the reasons we believed that the typical methodology for recalibrating a parity adjustment would not be appropriate in the context of PDPM and may lead to an overcorrection. As discussed previously in this final rule and in the FY 2012 SNF PPS final rule (76 FR 26371), we would typically utilize claims and assessment data from a given period under the new payment system, classify patients under both the current and prior payment model using this same set of data, compare aggregate payments under each payment model, and calculate an appropriate adjustment factor to achieve budget neutrality. However, given the significant changes in therapy provision since PDPM implementation, we found that using FY 2020 patient assessment data collected under PDPM would lead to a significant underestimation of RUG-IV case mix for purposes of determining what aggregate payments would have been under RUG-IV for the same period.
We invited comments on the information presented above, as well as on the potential impact of using the reported FY 2020 patient assessment data from the MDS to reclassify SNF beneficiaries under RUG-IV, consistent with the same type of recalibration methodology we have used for prior system transitions.
3. Methodology for Recalibrating the PDPM Parity Adjustment
In this section, we discuss the methodology we considered in the FY 2022 proposed rule for recalibrating the PDPM parity adjustment. Table 23 provides the expected and actual average PDPM CMI expected for each of the PDPM rate components based on data from FY 2019 and FY 2020. First, we calculated the expected average CMI for each component by summing the expected PDPM CMI for each day of service in FY 2019 and then dividing by the total number of days of service in FY 2019. Next, we provided two separate calculations for the actual average PDPM CMI, both for the full SNF population and for the SNF population after exclusions due to COVID (henceforth referred to as the "subset population"), by summing the CMI for each day of service in FY 2020 and then divided this by the total number of days of service in FY 2020. As discussed above, we excluded SNF stays where the patient was diagnosed with COVID- Start Printed Page 42468 19 or the stay utilized a PHE for COVID-19 related waiver, as identified by the presence of a "DR" condition code on the associated SNF claim.

The results presented in Table 23 show that the average CMI for both the full and subset FY 2020 populations was slightly lower than expected for the PT and OT rate components, and much higher than expected for the SLP, Nursing, and NTA components. We believed that the significant increases of 22.6 percent, 16.8 percent, and 5.6 percent in average case-mix, respectively, for the full FY 2020 SNF population was primarily responsible for the inadvertent increase in spending under PDPM. Further, given that we observed similar increases in the average CMI for these components in the subset FY 2020 SNF population, we believed that these increases in average case-mix for these components were the result of PDPM and not the PHE for COVID-19. We invited comments on this approach and the extent to which commenters believed that the PHE for COVID-19 may have impacted the PDPM case-mix distribution in ways not captured in Table 23 or in the discussion provided here.
Historically, our basic methodology for recalibrating the parity adjustment has been to compare total payments under the new case-mix model with what total payments would have been under the prior case-mix model, were the new model not implemented. In the context of the PDPM, this meant comparing total FY 2020 payments under PDPM to what FY 2020 payments would have been under RUG-IV if PDPM were not implemented. In order to calculate expected total payments under RUG-IV, we used the percentage of stays in each RUG-IV group in FY 2019 and multiplied these percentages by the total number of FY 2020 days of service. We then multiplied the number of days for each RUG-IV group by the RUG-IV per diem rate, which we obtained by inflating the FY 2019 SNF PPS RUG-IV rates by the FY 2020 market basket update factor. The total payments under RUG-IV also accounted for the AIDS add-on under RUG-IV and a provider's FY 2020 urban or rural status. In order to calculate the actual total payments under PDPM, we used data reported on FY 2020 claims. Specifically, we used the Health Insurance Prospective Payment System (HIPPS) code on the SNF claim to identify the patient's case-mix assignment and associated CMIs, utilization days on the claim to calculate stay payments and the variable per diem adjustment, the presence of an HIV diagnosis on the claim to account for the PDPM AIDS add-on, and a provider's urban or rural status. As with the analysis for Table 23, we calculated total payments both for the full and subset FY 2020 SNF populations.
We believed that this methodology provided a more accurate representation of what RUG-IV payments would have been in FY 2020, were it not for the change in payment incentives and care provision precipitated by PDPM implementation, than using data reported under PDPM to reclassify these patients under RUG-IV. In particular, given the reduction in therapy utilization under PDPM as compared to RUG-IV, using the therapy utilization data reported under PDPM to reclassify SNF patients back into RUG-IV groups would produce a case-mix distribution that would be significantly different from the RUG-IV case-mix distribution we would have expected were it not for PDPM implementation. Since the reduction in therapy would lead to a reduction in the RUG-IV case-mix assignments (for example, Ultra-High and Very-High Rehabilitation assignments are not nearly as prevalent using PDPM-reported data as they are using data that existed prior to PDPM), this would lead to an underestimation of what RUG-IV payments would have been in FY 2020. This, in turn, would lead to an overcorrection in recalibrating the parity adjustment due to the low estimated total RUG-IV payments. Additionally, given the significant changes in the patient assessment schedule, specifically the removal of the Change of Therapy Other Medicare Required Assessment, we cannot know if the patient would continue to remain classified in the RUG-IV group into which the patient classified on the 5-day assessment beyond that assessment window. In other words, without having an interim assessment between the 5-day assessment and the patient's discharge from the facility, we would be unable to determine if the RUG-IV group into which the patient classified on the 5-day assessment changed during the stay, or if the patient continued to receive an amount of therapy services consistent with the initial RUG-IV classification. As a result, using reported data under PDPM could lead to a reclassification of patients under RUG-IV that is not consistent with how patients would have been classified under RUG-IV if PDPM had not been implemented. As such, we believed that using the FY 2019 RUG-IV case-mix distribution as a proxy for what the RUG-IV case-mix distribution would have been in FY 2020 were it not for PDPM implementation provides a more accurate calculation of what total RUG-IV payments would have been during FY 2020 absent PDPM implementation.
Our analysis identified a 5.3 percent increase in aggregate spending under PDPM as compared to expected total payments under RUG-IV for FY 2020 Start Printed Page 42469 when considering the full SNF population, and a 5 percent increase in aggregate spending under PDPM for FY 2020 when considering the subset population. Although these results are similar, in light of the potential differences in the PDPM case-mix distribution that may have been precipitated by the admission of patients diagnosed with COVID-19 and patients whose stays utilized a PHE-related waiver, we believe it would be more appropriate to pursue a recalibration using the subset population. Since the initial increase to the PDPM CMIs to achieve budget neutrality applied equally across all case-mix adjusted components, we believed it would be appropriate, in the event an adjustment is made, to adjust the CMIs across all such components in equal measure. Using the methodology described above, the resultant PDPM parity adjustment factor would be lowered from 46 percent to 37 percent for each of the PDPM case-mix adjusted components. If we applied this methodology for FY 2022, we estimated a reduction in SNF spending of 5 percent, or approximately $1.7 billion.
Based on the above discussion and analysis, we described a potential path towards a recalibration of the PDPM parity adjustment. We invited comments on our methodology, particularly on the use of the FY 2019 RUG-IV case-mix distribution to calculate expected FY 2020 SNF payments and on using the subset FY 2020 SNF population.
As we noted in the FY 2012 SNF PPS final rule (76 FR 48493), we believe it is imperative that we act in a well-considered but expedient manner once excess payments are identified, as we did in FY 2012. However, despite the importance of ensuring that PDPM is budget neutral going forward, we acknowledged that applying such a significant reduction in payments in a single year without time to prepare for the reduction in revenue could create a financial burden for providers. We therefore considered two potential mitigation strategies to ease the transition to prospective budget neutrality in the event an adjustment is finalized: Delayed implementation and phased implementation.
With regard to a delayed implementation strategy, this would mean that we would implement the reduction in payment, or some portion of the reduction in payment if combined with a phased implementation approach described below, in a later year than the year in which the reduction is finalized. For example, considering the 5 percent reduction discussed above, if this reduction was finalized in FY 2022 with a 1 year delayed implementation, this would mean that the full 5 percent reduction would be prospectively applied to the PDPM CMIs in FY 2023. If the reduction was finalized in FY 2022 with a 2 year delayed implementation, then the full 5 percent reduction in the PDPM CMIs would be applied prospectively beginning in FY 2024. This type of strategy on its own does not serve to mitigate the overall amount of the reduction in a single year, but rather serves to provide facilities with time to prepare for the impending reduction in payments. We solicited comments on whether stakeholders believe that, in the event we finalize the parity adjustment recalibration, we should finalize this recalibration with a delayed implementation. Additionally, to the extent that stakeholders believe that a delayed implementation would be warranted, we solicited comments on the appropriate length of the delay.
With regard to a phased implementation strategy, this would mean that the amount of the reduction would be spread out over some number of years. Such an approach helps to mitigate the impact of the reduction in payments by applying only a portion of the reduction in a given year. For example, if we were to use a 2-year phased implementation approach to the 5 percent reduction discussed above, this would mean that the PDPM CMIs would be reduced by 2.5 percent in the first year of implementation and then reduced by the remaining 2.5 percent in the second and final year of implementation. So, for example, if this adjustment was finalized for FY 2022, then the PDPM CMIs would be reduced by 2.5 percent in FY 2022 and then reduced by an additional 2.5 percent in FY 2023. We note that the number of years for a phased implementation approach could be as little as 2 years but as long as necessary to appropriately mitigate the yearly impact of the reduction. For example, we could implement a 5-year phased approach for this reduction, which would apply a one percent reduction to the PDPM CMIs each year for 5 years. We solicited comments on the need for a phased implementation approach to recalibrating the PDPM parity adjustment, as well as on the appropriate length of such an approach.
We could also use a combination of both mitigation strategies. For example, we could finalize a 2 year phased approach with a 1 year delayed implementation. Using FY 2022 as the hypothetical year in which such an approach could be finalized, this would mean that there would be no reduction to the PDPM CMIs in FY 2022, a 2.5 percent reduction to the PDPM CMIs in FY 2023, and then a 2.5 percent reduction in the PDPM CMIs in FY 2024. We solicited comments on the possibility of combining these approaches and what stakeholders believe would be appropriate to mitigate the impact of the reduction in SNF PPS payments.
We noted that for any of these options, the adjustment would be applied prospectively, and the case mix indexes would not be adjusted to account for deviations from budget neutrality in years before the payment adjustments are implemented.
We invited comments on the methodology described above for recalibrating the PDPM parity adjustment and the strategies described above for mitigating the impact of implementing such an adjustment, in the event we finalize a recalibration.
Comment: The majority of commenters strongly objected to our methodology and the possibility of finalizing the recalibration in FY 2022 during the COVID-19 PHE. We received comments about this issue both from individual commenters and multiple letter writing campaigns. Commenters suggested that FY 2020 data was not representative because PDPM was only in place for 5 months, from October 2019 to February 2020, prior to the beginning of the PHE. They outlined several ways that the PHE affected FY 2020 data in ways not accounted for by our subset population methodology, which excluded patients with a COVID-19 diagnosis or who utilized a PHE-related disaster waiver. Their critiques of our methodology fall into two categories: That we did not fully account for the acuity of patients with COVID-19 and that we did not fully account for the overall effect of the PHE across all patients.
First, commenters were concerned that our analysis did not account for the impact of COVID-19 on overall patient case-mix and acuity. Some commenters suggested that we may have missed COVID-19 cases from the early months of the PHE because there was no COVID-19 specific diagnosis code available before April 2020 and because providers were unaware of or confused about waiver utilization. Additionally, the well-documented shortage of COVID-19 testing led to SNFs being unable to confirm and report COVID-19 cases despite higher than average caseloads in upper respiratory infections and associated increases in patient acuity. In light of this, one commenter suggested that we analyze the FY 2020 data for a higher-than- Start Printed Page 42470 expected burden of upper respiratory infection cases and exclude these sicker patients from the parity adjustment analysis. Finally, commenters were concerned that PDPM did not fully capture clinically appropriate sequelae or adequately reimburse intensive nursing care provided to COVID-19 patients who were cohorted together instead of in a single room.
Second, commenters stated that the PHE raised the clinical complexity of all residents regardless of COVID-19 illness or diagnosis, therefore skewing the case-mix data for FY 2020. Because many providers chose to halt elective surgeries during a portion of the PHE, the residents admitted were the most acute who could not be cared for at home. Limitations regarding visitation led to higher levels of mood distress, cognitive decline, mobility decline, change in appetite, weight loss requiring diet modifications, and compromised skin integrity. Occupancy dropped significantly compared to pre-pandemic levels (many commenters reported an approximate 20 percent decrease) and commenters believe it could take up to 2 or 3 years to return to a pre-pandemic level census. One commenter expressed concern with the accuracy of the CMIs due to having a smaller sample size due to excluding COVID cases, stating that these factors would have impacted average CMI calculations and would not be representative of an average SNF yearly census.
Overall, the majority of commenters agreed that it was difficult to assess true PDPM case-mix distribution due to only a very short period before the PHE, and therefore believed that a longer time period of data outside of a PHE environment is necessary to determine whether a parity adjustment is required. They urged CMS to take more time for deliberation and utilize a period of data outside of a PHE environment, defined by one commenter as beginning 90 days after the end of the PHE and continuing for one year thereafter.
Some commenters supported the analytic approach we described in the proposed rule and concurred with the need for a parity adjustment. While MedPAC recommended proceeding cautiously and making no update for FY 2022, they found our data analysis approach to be reasonable and urged CMS to keep an account of overpayments that would have been made in establishing future updates. Several commenters indicated that they would support a future parity adjustment, if warranted, if CMS combines delayed implementation with a phased-in approach. One commenter recommended proceeding with the parity adjustment for FY 2022 due primarily to behavioral changes exhibited by SNFs at the outset of PDPM, such as the reduction in therapy services provided to SNF patients.
Response: We thank the commenters for their feedback. In light of these comments, as well as the importance of addressing any existing overpayments under the SNF PPS, we intend to utilize these comments to refine the data we have collected in developing a proposed methodology that will be included in the FY 2023 SNF PPS Proposed Rule.
Comment: Several commenters made suggestions for revisions to our methodology and opposed the possibility of finalizing the recalibration in FY 2022 for reasons unrelated to the COVID-19 PHE. Some commenters pointed out that our analysis did not account for the effect of CMS' instruction to assess all patients anew in October 2019 using the PDPM MDS assessment, which would likely have elevated NTA scores due to restarting the stay at the highest payment level, even though some patients assessed may have been in the middle or end of their Medicare Part A coverage. One commenter supported our methodology, stating that it would be inappropriate to attempt to reclassify the data set associated with the FY 2020 SNF population using the RUG-IV model, given the significant differences between the two and the changes implemented to the patient assessment schedule.
Some commenters suggested that budget neutrality may not be an attainable goal because less attention was paid to diagnosis coding under RUG-IV. One commenter stated that the exact opposite occurred of the assumption stated in the proposed rule regarding no changes in the population, provider behavior, and coding, as PDPM represented a significant change in how nursing homes should manage and document care for Medicare Part A residents. The same commenter stated that by transitioning to a system where therapy minutes primarily drove reimbursement to a system where a more holistic coding approach established payment, one would expect more accurate coding. This change is better for patient care and does not indicate that conditions such as depression and swallowing difficulties were not treated prior to PDPM, but rather indicates providers are demonstrating more accurate documentation to support the care already being given for these conditions.
Response: We thank the commenters for their feedback and will take these recommendations into consideration for the FY 2023 SNF PPS proposed rule. However, we remind commenters that the methodology used to identify the magnitude of the adjustment necessary to achieve parity does not rely on the actual dollar amounts paid under PDPM, but rather a comparison between expected SNF PPS payments, based on historical case-mix utilization data under RUG-IV, to SNF PPS payments based on actual case-mix utilization data collected after PDPM implementation.
Comment: Some commenters stated that expenditures for their facilities did not support a 5 percent potential parity adjustment. One commenter calculated a 4.5 percent increase, inclusive of the 2.8 percent market basket increase, in overall payment under PDPM as compared to the RUG-IV. Another commenter stated that the PDPM budget neutrality adjustment did not take into account the 2 percent reduction (60 percent of which would be available to be earned back as a value-based incentive payment) to be put in the Medicare trust fund from the SNF VBP program.
Response: We appreciate these comments. As described in the proposed rule, our methodology included the subset population of SNF beneficiaries without a COVID-19 diagnosis or a PHE-related disaster waiver, across all facilities. We understand that there may be variation between facilities, though the parity adjustment is calculated and applied at a systemic level to all facilities paid under the SNF PPS. We emphasize that budget neutrality refers only to the transition between case-mix classification models (in this case, from RUG-IV to PDPM) and is not intended to include unrelated SNF policies such as the market basket increase or the SNF VBP program.
Comment: One commenter supported delaying the PDPM parity adjustment due to the proposed substantive changes to the ICD-10 diagnosis code mapping, stating that these changes may have a significant impact on the accuracy of patient classification and on payment amounts if finalized.
Response: We thank the commenter for this feedback and will take this recommendation into consideration for the FY 2023 SNF PPS proposed rule.
Comment: The majority of commenters supported combining both mitigation strategies of delayed implementation of 2 years and a gradual phase-in of no more than 1 percent per year. MedPAC supported delayed implementation, but did not believe a phased-in approach is warranted given Start Printed Page 42471 the high level of aggregate payment to SNFs.
Response: We thank the commenters for their feedback and will take these recommendations into consideration for the FY 2023 SNF PPS proposed rule.
Comment: Some commenters made recommendations to revise the methodology for applying the recalibrated parity adjustment factor, after it is recalculated in light of the comments on the proposed rule. Several commenters disagreed with adjusting the CMIs across all case-mix adjusted components in equal measure, suggesting that this approach would harm patient care by further reducing therapy minutes. Instead, the commenters recommended adjusting only the CMIs for those PDPM components that drive the unintended increase observed under PDPM. According to data provided in the proposed rule, these would be the SLP, Nursing, and NTA components, not the PT or OT components. One commenter further recommended that the bottom four PDPM SLP groups (A, B, C, and D) remain unadjusted as those reimbursement levels are already very low. Several other commenters disagreed with adjusting the CMIs across all SNFs, instead suggesting that CMS should develop indicators to identify and impose financial penalties on the specific facilities driving the increase.
Response: We thank the commenters for their feedback and will take these recommendations into consideration for the FY 2023 SNF PPS proposed rule.
We thank the commenters for their feedback and will take these suggestions and recommendations into consideration as we consider the best path forward to ensure budget neutrality in the FY 2023 SNF PPS proposed rule. As stated earlier in this section, we believe it is imperative that we act in a well-considered but expedient manner once excess payments are identified. Additionally, as stated earlier in this section, our analysis of FY 2020 data found that even after removing beneficiaries using a PHE-related waiver or with a COVID-19 diagnosis from our data set, the observed inadvertent increase in SNF payments since PDPM was implemented was approximately the same. We will continue to monitor all available data and take that into consideration, in combination with the feedback and recommendations received, for developing the FY 2023 SNF PPS proposed rule.
VII. Skilled Nursing Facility (SNF) Quality Reporting Program (QRP)
A. Background and Statutory Authority
The Skilled Nursing Facility Quality Reporting Program (SNF QRP) is authorized by section 1888(e)(6) of the Act, and it applies to freestanding SNFs, SNFs affiliated with acute care facilities, and all non-CAH swing-bed rural hospitals. Section 1888(e)(6)(A)(i) of the Act requires the Secretary to reduce by 2 percentage points the annual market basket percentage update described in section 1888(e)(5)(B)(i) of the Act applicable to a SNF for a fiscal year, after application of section 1888(e)(5)(B)(ii) of the Act (the productivity adjustment) and section 1888(e)(5)(B)(iii) of the Act, in the case of a SNF that does not submit data in accordance with sections 1888(e)(6)(B)(i)(II) and (III) of the Act for that fiscal year. For more information on the requirements we have adopted for the SNF QRP, we refer readers to the FY 2016 SNF PPS final rule (80 FR 46427 through 46429), FY 2017 SNF PPS final rule (81 FR 52009 through 52010), FY 2018 SNF PPS final rule (82 FR 36566 through 36605), FY 2019 SNF PPS final rule (83 FR 39162 through 39272), and FY 2020 SNF PPS final rule (84 FR 38728 through 38820).
B. General Considerations Used for the Selection of Measures for the SNF QRP
For a detailed discussion of the considerations we use for the selection of SNF QRP quality, resource use, or other measures, we refer readers to the FY 2016 SNF PPS final rule (80 FR 46429 through 46431).
1. Quality Measures Currently Adopted for the FY 2022 SNF QRP
The SNF QRP currently has 13 measures for the FY 2022 SNF QRP, which are outlined in Table 24. For a discussion of the factors used to evaluate whether a measure should be removed from the SNF QRP, we refer readers to 42 CFR 413.360(b)(3).
Start Printed Page 42472

C. SNF QRP Quality Measure Proposals Beginning With the FY 2023 SNF QRP
Section 1899B(h)(1) of the Act permits the Secretary to remove, suspend, or add quality measures or resource use or other measures described in sections 1899B(c)(1) and (d)(1) of the Act, respectively, so long as the Secretary publishes in the Federal Register (with a notice and comment period) a justification for such removal, suspension or addition. Section 1899B(a)(1)(B) of the Act requires that all of the data that must be reported in accordance with section 1899B(a)(1)(A) of the Act (including resource use or other measure data under section 1899B(d)(1)) be standardized and interoperable to allow for the exchange of the information among post-acute care (PAC) providers and other providers and the use by such providers of such data to enable access to longitudinal information and to facilitate coordinated care.
We proposed to adopt two new measures for the SNF QRP beginning with the FY 2023 SNF QRP: The SNF Healthcare-Associated Infections Requiring Hospitalization measure (SNF HAI) and the COVID-19 Vaccination Coverage among Healthcare Personnel (HCP)[4] measure as an "other measure" under section 1899B(d)(1) of the Act. The SNF HAI measure is an outcome measure. The data used to report the SNF HAI measure are standardized and interoperable and would allow providers to exchange this data and compare outcomes across the care continuum and PAC settings. Clinical data captured in every clinical setting informs a resident's current medical care plan, facilitates coordinated care, and improves Medicare beneficiary outcomes. We plan to develop HAI measures in other PAC settings, such as the Inpatient Rehabilitation Facility (IRF) Quality Reporting Program and the Long-Term Care Hospital (LTCH) Quality Reporting Program. The proposed measure supports the CMS Meaningful Measures Initiative through the Making Care Safer by Reducing Harm Caused in the Delivery of Care domain. We have previously solicited feedback on the SNF HAI measure as a future measure for the SNF QRP and received several comments of support as well as a few comments recommending suggestions (84 FR 38765). The measure is described in more detail below.
We proposed the COVID-19 Vaccination Coverage among HCP measure as an "other" measure under section 1899B(d)(1) of the Act beginning with the FY 2023 SNF QRP. In accordance with section 1899B(a)(1)(B) of the Act, the data used to calculate this measure are standardized and interoperable. The proposed measure supports the Meaningful Measures domain of Promote Effective Prevention Start Printed Page 42473 and Treatment of Chronic Disease. We identified the measure concept as a priority in response to the current public health crisis. This process measure was developed with the Centers for Disease Control and Prevention (CDC) to track COVID-19 vaccination coverage among HCP in the SNF setting. This measure is described in more detail below.
In addition, we proposed to update the denominator for one measure, the Transfer of Health (TOH) Information to the Patient—Post-Acute Care (PAC) measure to exclude residents discharged home under the care of an organized home health service or hospice.
1. Skilled Nursing Facility (SNF) Healthcare-Associated Infections (HAI) Requiring Hospitalization Quality Measure Beginning With the FY 2023 SNF QRP
a. Background
Monitoring the occurrence of HAIs among SNF residents can provide valuable information about a SNF's quality of care. Although HAIs are not considered "never events", or serious adverse errors in the provision of health care services that should never occur, most are preventable as they are often the result of poor processes and structures of care.[5] Evidence suggests there is a wide variation in HAI rates among SNF providers. An analysis of FY 2018 SNF claims indicates a performance gap in HAI rates across SNFs. Among the 14,347 SNFs included in the sample for the analysis, risk-adjusted measure scores ranged from a minimum of 2.19 percent to a maximum of 19.83 percent. Further, a 2014 report from the Office of the Inspector General (OIG) estimated that one in four adverse events among SNF residents are due to HAIs, and more than half of all HAIs are potentially preventable.[6] Typically, HAIs result from inadequate patient management following a medical intervention, such as surgery or device implementation, or poor adherence to protocol and antibiotic stewardship guidelines.[7 8 9] Several provider characteristics are also related to HAIs including staffing levels (for example, high turnover, low staff-to-resident ratios, etc.), facility structure characteristics (for example, national chain membership, high occupancy rates, etc.), and adoption or lack thereof of infection surveillance and prevention policies.[10 11 12 13 14 15] Inadequate prevention and treatment of HAIs is likely to result in poor health care outcomes for residents and wasteful resource use. For example, HAIs are associated with longer lengths of stay, use of higher-intensity care (for example, critical care services and hospital readmissions), increased mortality, and high health care costs.[16 17 18 19] Monitoring SNF HAI rates would provide information about each facility's adeptness in infection prevention and management.
Addressing HAIs in SNFs is particularly important as several factors place SNF residents at high risk for infection, including increased age, cognitive and functional decline, use of indwelling devices, frequent care transitions, and close contact with other resident and healthcare workers.[20 21] Furthermore, in SNFs, COVID-19 has a disproportionate impact on racial and ethnic minorities as well as people living with disabilities.[22 23] Emerging COVID-19 studies reveal higher patient spread due to poor infection control, staff rotations between multiple SNFs, and poor patient COVID-19 screenings.[24 25] An analysis comparing Start Printed Page 42474 SNF HAI rates using FY 2019 data with the currently reported rates of COVID-19 in SNFs found that nursing homes with higher HAI rates in FY 2019 also have a higher number of COVID-19 cases.[26] This analysis was presented to the PAC-LTC MAP Workgroup at the January 11th meeting (http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=94559, slide 134). We believe this finding supports a relationship not only between this measure and overall HAI prevention and control in SNFs, but also in predicting those SNFs more likely to have higher rates of infection in future pandemics. Several interventions may reduce HAI rates among SNFs, thus improving quality of care. These interventions include the adoption of infection surveillance and prevention policies, safety procedures, antibiotic stewardship, and staff education and training programs.[27 28 29 30 31 32 33] Additionally, infection prevention and control programs with core components in education, monitoring, and feedback on infection rates from surveillance programs or feedback on infection control practices from audits have been found to be successful interventions for reducing HAIs.[34] The effectiveness of these interventions suggests improvement of HAI rates among SNF residents is possible through modifying provider-led processes and interventions.
The proposed SNF HAI measure uses Medicare fee-for-service (FFS) claims data to estimate the risk-standardized rate of HAIs that are acquired during SNF care and result in hospitalization. Unlike other HAI measures that target specific infections, this measure would target all HAIs serious enough to require admission to an acute care hospital. Given the current COVID-19 public health emergency, we believe this measure would promote patient safety and increase the transparency of quality of care in the SNF setting. This measure also compares SNFs to their peers to statistically separate those that perform better than or worse than each other in infection prevention and management. We believe peer comparison would encourage SNFs to improve the quality of care they deliver.
b. Stakeholder and Technical Expert Panel (TEP) Input
In our development and specification of this measure, we employed a transparent process in which we sought input from stakeholders and national experts and engaged in a process that allowed for pre-rulemaking input, in accordance with section 1890A of the Act.
To meet this requirement, we provided the following opportunities for stakeholder input. Our measure development contractor for the SNF HAI measure convened a Technical Expert Panel (TEP) on May 9, 2019 to obtain expert input on the development of an HAI measure for use in the SNF QRP. The TEP consisted of stakeholders with a diverse range of expertise, including SNF and PAC subject matter knowledge, clinical and infectious disease expertise, patient and family perspectives, and measure development experience. The TEP supported the proposed measure concept and provided substantive input regarding the measure's specifications. Recommendations provided by the TEP included refining the measure's operational definition, exclusion criteria, and HAI ICD-10 diagnosis code list, among other considerations. All recommendations from the TEP were taken into consideration and applied appropriately where feasible. A summary of the TEP proceedings titled SNF HAI Final TEP Report is available on the SNF QRP Measures and Technical Information page at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Skilled-Nursing-Facility-Quality-Reporting-Program/SNF-Quality-Reporting-Program-Measures-and-Technical-Information.
Following the TEP, our measure development contractor released draft quality measure specifications for public comment on the SNF HAI measure. Stakeholder feedback was solicited on the proposed measure by requesting comment on the CMS Measures Management System Blueprint site. The comment submission period was from September 14, 2020 to October 14, 2020. Comments on the measure varied. Many commenters supported the idea of adopting an HAI measure to improve prevention efforts; however, commenters also offered criticisms about the measure's specifications and implementation. The summary report of the September 14 to October 14, 2020 public comment period titled SNF HAI Public Comment Summary Report is available on the SNF QRP Measures and Technical Information page at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Skilled-Nursing-Facility-Quality-Reporting-Program/SNF-Quality-Reporting-Program-Measures-and-Technical-Information.
c. Measure Applications Partnership (MAP) Review
Our pre-rulemaking process includes making publicly available a list of quality and efficiency measures, called the Measures under Consideration (MUC) List that the Secretary is considering adopting through the Federal rulemaking process for use in Medicare programs. This allows multi-stakeholder groups to provide recommendations to the Secretary on the measures included on the list.
We included the SNF HAI measure under the SNF QRP Program in the publicly available "List of Measures under Consideration for December 21, Start Printed Page 42475 2020" (MUC List).[35] The National Quality Forum (NQF)-convened Measure Applications Partnership (MAP) Post-Acute Care/Long-Term Care (PAC-LTC) workgroup met virtually on January 11, 2021 and provided input on the proposed measure. The MAP offered conditional support of the SNF HAI measure for rulemaking contingent upon NQF endorsement, noting that the measure adds value to the SNF QRP by presenting one overall measurement of all HAIs acquired during SNF care that result in hospitalizations, information that is not currently available. The MAP recognized that the proposed measure is intended to reflect global infection control for a facility, and may encourage SNFs to access processes and perform interventions to reduce adverse events among SNF residents that are due to HAIs. The MAP Rural Health Workgroup also agreed that the SNF HAI measure is suitable for use with rural providers in the SNF QRP. The final MAP report is available at http://www.qualityforum.org/Publications/2021/03/MAP_2020-2021_Considerations_for_Implementing_Measures_Final_Report_-_Clinicians,_Hospitals,_and_PAC-LTC.aspx.
Additionally, measure testing was conducted on the SNF HAI measure. Split-half testing revealed the proposed measure's moderate reliability. Validity testing of the measure showed good model discrimination as the HAI model can accurately predict HAI cases while controlling for differences in resident case-mix. The SNF HAI TEP also showed strong support for the face validity of the proposed measure. For measure testing details, refer to the document titled, Skilled Nursing Facility Healthcare-Associated Infections Requiring Hospitalization for the Skilled Nursing Facility Quality Reporting Program Technical Report available on the SNF QRP Measures and Technical Information page at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Skilled-Nursing-Facility-Quality-Reporting-Program/SNF-Quality-Reporting-Program-Measures-and-Technical-Information. This proposed measure is not currently NQF endorsed, but CMS plans to submit the measure for NQF endorsement in the future.
d. Competing and Related Measures
Section 1899B(e)(2)(A) of the Act requires that, absent an exception under section 1899B(e)(2)(B) of the Act, measures specified under section 1899B of the Act be endorsed by the entity with a contract under section 1890(a) of the Act, currently the National Quality Forum (NQF). In the case of a specified area or medical topic determined appropriate by the Secretary for which a feasible and practical measure has not been endorsed, section 1899B(e)(2)(B) of the Act permits the Secretary to specify a measure that is not so endorsed, as long as due consideration is given to measures that have been endorsed or adopted by a consensus organization identified by the Secretary.
The proposed SNF HAI measure is not NQF endorsed, so we considered whether there are other available measures that assess HAIs in SNFs. After review of the NQF's consensus-endorsed measures, we were unable to identify any NQF endorsed measures for SNFs focused on capturing several types of severe infections attributable to the SNF setting in one composite score. For example, although the measures Percent of Residents with a Urinary Tract Infection (Long-Stay) (NQF #0684), National Healthcare Safety Network (NHSN) Catheter-Associated Urinary Tract Infections (NQF #0138), NHSN Central Line-Associated Bloodstream Infections (NQF #0139), and NHSN Facility-Wide Inpatient Hospital-onset Clostridium Difficile Infection (NQF #1717) are NQF endorsed and all report on specific types of infections, they do not provide an overall HAI rate and are not specific to the SNF setting. Additionally, although the Skilled Nursing Facility 30-Day All-Cause Readmission measure (NQF #2510), the Potentially Preventable 30-Day Post-Discharge Readmission measure for SNF QRP, and the Skilled Nursing Facility 30-Day Potentially Preventable Readmission after Hospital Discharge measure (SNFPPR) are all specific to the SNF setting, they are not solely focused on infections. We intend to submit this proposed measure to the NQF for consideration of endorsement when feasible.
Therefore, after consideration of other available measures, we find that the exception under section 1899B(e)(2)(B) of the Act applies and are proposing the measure, Skilled Nursing Facility (SNF) Healthcare-Associated Infections (HAI) Requiring Hospitalization measure beginning with the FY 2023 SNF QRP.
e. Quality Measure Calculation
The proposed measure estimates the risk-standardized rate of HAIs that are acquired during SNF care and result in hospitalization using 1 year of Medicare FFS claims data.
Both the proposed measure numerator and denominator are risk-adjusted. The measure's adjusted numerator is the estimated number of SNF stays predicted to have an HAI that results in hospitalization. The estimate starts with the observed count of the measure outcome, which is then risk-adjusted for resident characteristics and a statistical estimate of the SNF effect beyond resident case mix. The term "SNF effect" represents provider-specific behaviors that result in facilities' HAI rates. These behaviors may include adherence to evidence-based infection control policies and procedures. The adjusted denominator is the expected number of SNF stays with the measure outcome. The adjusted denominator is calculated by risk-adjusting the total eligible SNF stays for resident characteristics excluding the SNF effect.
The proposed measure is calculated using a standardized risk ratio (SRR) in which the predicted number of HAIs for SNF stays per provider is divided by the expected number of HAIs. For each SNF, a risk-adjusted rate of HAIs that are acquired during SNF care and result in hospitalization is calculated by multiplying the SRR by the overall national observed rate of HAIs for all SNF stays. The measure is risk-adjusted for age and gender characteristics, original reason for Medicare Entitlement, principal diagnosis during the prior proximal inpatient (IP) stay, types of surgery or procedure from the prior proximal IP stay, length of stay and ICU/CCU utilization from the prior proximal IP stay, dialysis treatment from the prior proximal IP stay, and HCC comorbidities and number of prior IP stays within 1 year preceding the SNF stay. For technical information about this proposed measure, including information about the measure calculation, risk adjustment, and exclusions, refer to the document titled, Skilled Nursing Facility Healthcare-Associated Infections Requiring Hospitalization for the Skilled Nursing Facility Quality Reporting Program Technical Report available on the SNF QRP Measures and Technical Information page at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Skilled-Nursing-Facility-Quality-Reporting-Program/SNF-Quality-Reporting-Program-Measures-and-Technical-Information. If this measure is finalized, we intend to publicly report this measure using four quarters of claims data. We refer readers to section VII.H.2. of this proposed rule for information regarding public reporting. Start Printed Page 42476
We invited public comment on our proposal to adopt the quality measure, the Skilled Nursing Facility (SNF) Healthcare-Associated Infections (HAIs) Requiring Hospitalization measure (SNF HAI measure), beginning with the FY 2023 SNF QRP.
The following is a summary of the public comments received on our proposal to adopt the quality measure, Skilled Nursing Facility (SNF) Healthcare-Associated Infections (HAIs) Requiring Hospitalization measure (SNF HAI measure), beginning with the FY 2023 SNF QRP and our responses:
Comment: Several commenters supported adoption of the SNF HAI measure beginning with the FY 2023 SNF QRP. The Medicare Payment Advisory Commission (MedPAC) supported the adoption of the measure, stating that Medicare quality programs should include population-based outcome measures and the rate of infections acquired during a SNF stay that are severe enough to require hospitalization is an outcome of importance to beneficiaries and the Medicare program. Additionally, commenters noted that HAIs are potentially preventable and signal actionable gaps in care quality. Commenters agree that the measure is actionable in reducing HAI incidence, and does not add burden to providers through its use of Medicare FFS claims. One commenter supported interoperability of the measure in its future expansion to other post-acute care settings, such as IRFs and LTCHs. Another commenter supported the SNF HAI measure, recognizing emerging evidence that associates high SNF HAI rates with higher patient COVID-19 spread. Additional commenters supported the overall concept of the SNF HAI measure, recognizing the effectiveness of the measure to prevent and control the spread of infections and improve transparency among providers.
Response: We thank commenters for their support of the SNF HAI measure. We agree that there is a critical need to reduce HAIs in SNFs and that monitoring SNF HAI rates provides valuable information on a SNF's quality of care. We believe this proposed quality measure will address the lack of HAI data in SNFs, increase transparency, and help reduce rates of HAIs.
Comment: One commenter disagreed with the assertion that there is a performance gap regarding HAIs in SNFs. The commenter noted that there is an inability to define the magnitude of the issue which makes it difficult to identify benchmarks and goals.
Response: Our analysis of FY 2019 data demonstrated that there is a performance gap in HAI rates across SNFs. Among the 14,102 SNFs included in the sample for the analysis, risk-adjusted measure scores ranged from a minimum of 2.36 percent to a maximum of 17.62 percent.[36] Further, a 2014 report from the Office of the Inspector General (OIG) estimated that one in four adverse events among SNF residents are due to HAIs.[37] Although most HAIs are not considered "never-events," most are preventable and result from inadequate care processes and structures.[38] Including the SNF HAI measure in the SNF QRP would provide SNFs information to help them improve their infection control and prevention strategies, as they will learn about their own facility's HAI rate compared to their peer SNFs and the national average. Including the SNF HAI measure in the SNF QRP would also help patients choose which SNF they would like to receive care from.
Comment: A commenter supported the SNF HAI measure's focus on infection prevention in the nursing facility, but was concerned that FY 2019 data would be used as a benchmark for HAI performance and that FY 2019 data do not take into account changes in infection prevention requirements like those at 42 CFR 483.80(b), which requires the facility to designate one or more individual(s) as the infection preventionist(s) responsible for the facility's infection prevention and control program.
Response: We would like to clarify that FY 2019 data are not being used as a benchmark for HAI performance. This measure compares facilities' HAI rates to their peers (that is, all other SNFs in the United States), and to the national average. Therefore, the benchmark of this measure's performance is the national average of the reporting period, not specifically FY 2019. With regard to the infection preventionist role, we note that under § 483.80, facilities have been required to establish an infection prevention and control program since late 2016 prior to the infection preventionist role requirement effective late 2019.
Comment: Several commenters recommended that CMS postpone implementation of the measure until it receives NQF endorsement. These comments advocated for use of NQF-endorsed measures, indicating that the NQF process includes a robust measure review with routine measure maintenance to reflect changes in performance.
Response: We direct readers to section VII.C.1.d. of this final rule, where we discuss this topic in detail. Despite the current absence of NQF endorsement, we still believe it is critical to adopt the SNF HAI measure into the FY 2023 SNF QRP as one in four adverse events among SNF residents are due to HAIs, and approximately more than half of all HAIs are potentially preventable.[39] Identifying several types of severe HAIs attributable to the SNF setting in one composite score provides actionable information to providers that may hold them accountable, encourage them to improve the quality of care they deliver, and improve transparency. Although the SNF HAI measure is not currently endorsed by the NQF, we agree that there is value in obtaining measure endorsement and plan to submit the measure for NQF endorsement in the future.
Comment: Several commenters opposed the use of Medicare FFS claims for the SNF HAI measure. Many commenters do not believe that claims-based measures are appropriate for measuring HAIs, and would instead support the use of NHSN chart-abstracted surveillance data. Commenters emphasized the scientific process that ensures integrity and accuracy of NHSN data while questioning the reliability of claims data. Another commenter suggested using NHSN data in conjunction with claims data, noting the benefits of using standardized, validated NHSN definitions.
Response: As mentioned in the SNF HAI Final TEP Summary Report, some TEP members voiced concerns about the accuracy of using inpatient claims to accurately capture infections acquired in a SNF.[40] The TEP discussed Start Printed Page 42477 alternative data sources, including the use of NHSN data, but ultimately decided against it as it would increase provider burden. The TEP ultimately agreed that claims data are high quality and would strengthen the SNF QRP measure portfolio without increasing provider burden. Additionally, other claims-based measures have been deemed reliable through NQF endorsement, such as the Skilled Nursing Facility 30-Day All-Cause Readmission measure (SNFRM) (NQF #2510).
Comment: Many commenters opposed the use of Medicare claims due to concerns that its data delay would not allow for timely improvement of the HAI rate.
Response: We have worked to streamline our public reporting processes, and to narrow the gap between the submission of claims data and the public display of that data. To ensure that we give ample time for providers to submit their claims data, we have established a 90-day run-out period following the end of a calendar year or fiscal year. Beyond that, there are specific administrative and review/quality assurance processes that must take place in a sequential order for CMS to ensure we are displaying accurate data. We have narrowed this gap between claims submission and public display to the extent feasible at this time.
Comment: Commenters expressed concern over the measure's dependence on the diagnosis of patients by medical practitioners who are outside of the influence of the SNF. These commenters are concerned that because the measure outcome is calculated based on hospital information, not SNF information, it reflects the coding practices of hospitals rather than actual quality of care at SNFs. Commenters also expressed concerns about differences in hospital surveillance that may result in an inaccurate SNF HAI rate.
Response: We use inpatient claims for the SNF HAI measure because the measure's main outcome is HAIs that require hospitalization. In response to the commenters' assertion that inpatient claims are unreliable, a medical record review on the accuracy of hospital coding of Hospital Acquired Conditions (HACs) and Present on Admission (POA) conditions did not find patterns of widespread underreporting of HACs or overreporting of POA status.[41] Rather, the study found that only 3 percent of HAC cases were underreported and 91 percent of all cases coded POA were coded accurately. Another medical record review conducted by us assessed the accuracy of the principal diagnosis coded on a Medicare claim to identify whether a patient was admitted for a diagnosis included in our list of potentially preventable readmission (PPR) diagnoses.[42] The study analyzed inpatient discharges from October 2015 through September 2017 and found high agreement between principal diagnoses in Medicare claims and corresponding medical records. Specifically, the agreement rate between principal diagnoses in Medicare claims and information in the corresponding medical records ranged from 83 percent to 94 percent by study hospital. Additionally, 91 percent to 97 percent of principal diagnoses from the corresponding medical records were included in CMS' list of PPR diagnoses. Therefore, we disagree with commenters' concerns about the accuracy of inpatient claims data.
In addition, several other SNF QRP measures rely on data from other settings such as Skilled Nursing Facility 30-Day Potentially Preventable Readmission after Hospital Discharge (SNFPPR), Skilled Nursing Facility 30-Day All-Cause Readmission (SNFRM) (NQF #2510), and Potentially Preventable 30-Day Post-Discharge Readmission Measure for Skilled Nursing Facility Quality Reporting.
Comment: Several commenters disagreed with the measure's restriction to only include HAIs that require inpatient hospitalization and to exclude emergency room visits and observation stays. These commenters believe that limiting HAIs to only those that require hospitalization will undercount preventable HAIs and lead to negative outcomes for residents.
Response: We acknowledge that detecting all HAIs in the measure's definition would increase the amount of infection data provided to SNFs and empower quality improvement. However, we decided to propose only including HAIs requiring hospitalization in our measure definition in response to suggestions by the TEP.[43] One TEP member noted that SNFs could risk information overload if we include every possible HAI in the SNF HAI rate.
TEP members ultimately recommended that it would be more valuable for SNFs to have a concentrated list of severe infections to target quality improvement in the biggest impact areas. Avoiding information overload will help to make the measure more actionable, as SNFs may be able to target the focus of their infection and prevention control programs on their residents' most severe infections. The TEP also recommended excluding observation stays and emergency department visits out of concern that these stays are not long enough to acquire all the lab results needed for accurate diagnosis of infections.
Overall, TEP members believed that diagnoses of SNF residents transferred and hospitalized would be more likely to be based on the whole history and comprehensive test results and thus more likely to represent true infections.
Comment: Some commenters opposed the adoption of a composite score, with concern that the measure is not infection-specific and would not allow for timely facility-level targeted interventions. One commenter recommended to narrow the SNF HAI measure to specific infections such as central line-associated bloodstream infections (CLASBI) or catheter-associated urinary tract infections (CAUTI). This commenter noted that focusing on a couple of infections could make it easier to isolate performance issues and focus on improving those outcomes.
Response: The SNF HAI composite score is intended to provide a summary of overall performance in HAI prevention and control. Rather than focusing on interventions targeting a single infection, the goal of this measure is for SNFs to focus on foundational safety interventions, such as rates of hand washing, vaccinations, and Start Printed Page 42478 antibiotic stewardship programs that will reduce all instances of infection. We believe that reporting a composite, facility-level score is valuable because it informs SNFs of their overall HAI rates and allows them to compare these rates to their peers. This will enable SNFs to track their own performance and improve their quality of care through infection prevention and control programs. However, we recognize the benefits of measuring infection-specific data and will consider developing infection-specific HAI measures in the future.
Comment: One commenter urged that the SNF HAI measure should include mitigation approaches to prevent misattribution of a HAI to a SNF. This commenter also recommended that the measure implement infection-specific incubation periods and states that the COVID-19 pandemic has exposed the importance of infection-specific incubation periods. COVID-19 infections can occur before the onset of symptoms or a positive infection test result is observed, and in many cases, residents may have been exposed to COVID-19 prior to SNF admission.
Response: We acknowledge the difficulties of assigning attribution in the SNF setting since HAIs often have risk factors that are outside of the SNF's control. Although most are preventable, HAIs are not considered to be "never-events" and we acknowledge that residents may contract infections outside of the SNF. However, we note that it is the responsibility of the SNF to implement infection prevention protocols and to best manage infections when they occur. Further, to help prevention misattribution, the measure excludes certain community-acquired infections, implements an incubation window, and applies the Centers for Disease Control (CDC) and Prevention's National Healthcare Safety Network (NHSN) Repeat Infection Timeframe (RIT) to exclude preexisting infections that were acquired from the prior inpatient stay. Predating the COVID-19 pandemic, we obtained clinical input from TEP panelists on the SNF HAI measure about the time window to identify HAIs attributable to the SNF.[44] The TEP agreed that the same time window should be applied to all infections. Although the selected incubation window may not hold true for all infections, TEP members noted it was a reasonable average.
Since COVID-19 was not discussed during TEP proceedings, we will consider working with the CDC to determine whether or not this reasonable average approach is still appropriate or if we should consider establishing an infection-specific incubation window to account for COVID-19 in the future.
Comment: Several commenters did not find the measure actionable, citing that they would only have access to facility-level data rather than patient-level information. Commenters requested patient-level data in confidential feedback reports be available through the Certification and Survey Provider Enhanced Reports (CASPER) system, noting its importance in improving provider transparency and actionability. Additionally, commenters expressed the importance of providing facilities with infection-specific data to help reduce future infection prevalence.
Response: We disagree with the commenters that the use of facility-level data for the measure makes it less actionable. One of the benefits of a facility-level, composite indicator is its simplicity. A single score, representative of an entire facility, is easier to interpret, easier to use as a benchmark for tracking performance, and easier to use for comparisons among peers. The measure is not intended to stand alone; rather, it can be used in conjunction with other surveillance activities to plan for quality improvement. While an overall facility HAI rate may not provide information for targeting HAI prevention efforts to specific infection types, we believe that aggregate HAI prevalence data still provides actionable feedback to SNFs. The prevention of HAIs is not specific to an individual type of infection that can be presented in patient-level feedback reports. Rather, infection prevention and control efforts should address multiple infection types and SNFs should already be implementing infection control practices that include various approaches such as vaccination, isolation, hand washing, antibiotic stewardship programs, surveillance, sanitation, and staff training. Therefore, a facility-level HAI score is a reflection of quality of care as it measures a SNF's adeptness in infection prevention and management.
Comment: We received several comments about risk adjustment of the SNF HAI measure. One commenter disagreed that the SNF HAI measure should be risk-adjusted, especially for factors that are under facility control. This commenter believes that risk adjustment masks poor outcomes for residents that result directly from poor quality of care because risk adjustment excuses facilities from properly caring for high-risk patients.
Response: We share the commenters' concern that inclusion of certain covariates could mask adverse outcomes. However, lack of risk adjustment would disadvantage SNFs that specialize in treating high-risk populations in terms of HAI performance. In order to prevent provider manipulation, we focused on selecting factors that are not under the control of SNFs, such as patient characteristics rather than service provision. We would like to emphasize that the goal of this risk-adjusted measure is to identify SNFs that have notably higher rates of HAIs acquired during SNF care, when compared to the national average HAI rate. The purpose of risk adjustment is to account for risk factor differences across SNFs, when comparing quality of care among them. In other words, risk adjustment "levels the playing field" and allows for fairer quality-of-care comparisons across SNFs by controlling for differences in resident case-mix. Risk adjustment is particularly important for outcome measures because resident outcomes may be affected by factors such as age, gender, and health status that go beyond the quality of care delivered by SNFs.
Comment: A few commenters supported risk adjustment but considered the proposed risk adjustment approach as inadequate and missing patient-level and provider-level factors. One commenter specifically asked that the measure be risk adjusted to account for high rates of patients with spinal cord injuries.
Response: The risk adjustment model accounts for several patient-level factors such as age, sex, original reason for Medicare Entitlement, 283 principal diagnoses Clinical Classification Software (CCS) categories, 79 Hierarchical Condition Categories (HCC) comorbidities, 10 surgical procedure CCS categories from the prior proximal stay, length of stay, and intensive care unit (ICU)/critical care unit (CCU) utilization from the prior proximal stay. We would like to clarify that spinal cord injuries are included in the risk adjustment model as CCS 227 spinal cord injury and HCC72 spinal cord disorders/injuries.
Comment: One commenter was concerned about the lack of adjustment for social risk factors.
Response: Risk adjustment includes age and sex but we acknowledge that Start Printed Page 42479 the measure does not address social risk factors, such as income nor race/ethnicity. During the development of the SNF HAI measure, the NQF was conducting a Social Risk Trial to investigate social risk factors' association with outcome measures. Past NQF guidelines stated that social risk factors should not be included as adjustment variables. After the 2021 conclusion of the trial, the NQF acknowledged that adjusting for social risk factors can obscure disparities and the Disparities Standing Committee recommended that each performance measure be assessed individually to determine appropriateness of adjustment for social risk factors.[45] It is unclear if the benefits of adjusting for other social risk factors in the SNF HAI measure outweigh the potential consequences of masking social disparities. Therefore, we proposed to exclude social risk factors for now, but will continue to evaluate this issue by monitoring disparities and social risk factors as part of our routine measure monitoring work.
Comment: One commenter believes that risk adjustment is inappropriately applied at the patient level and hospital level due to the use of inpatient claims, rather than at the SNF level.
Response: SNF HAI risk adjustment is not implemented at the patient level nor at the hospital level. While the measure uses inpatient claims to identify HAIs acquired during a SNF stay, the unit of analysis for the risk adjustment is at the SNF stay level. The risk adjustment model applies a SNF provider-specific intercept via a hierarchical modeling approach. For more information about our risk adjustment approach, we refer to the SNF HAI Technical Report.[46]
Comment: One commenter advocated for CMS to be transparent about the measure's calculations, noting that providers should be able to calculate their own HAI rate for measure validation, if necessary.
Response: While we intend to make as much information related to SNF HAI performance as possible available to SNFs through confidential feedback reports under section 1899B(f) of the Act, we understand that claims-based quality measurement is difficult for SNFs to replicate for validation purposes. It would require familiarity with a number of data sources that are used to develop the risk-adjustment model for SNF HAI in order to account for variation across SNFs in case-mix and patient characteristics predictive of HAIs requiring hospitalization (including the Medicare Enrollment Database [EDB], Agency for Healthcare Research & Quality [AHRQ] Clinical Classification Software [CCS] groupings of ICD-10 codes, and CMS's HCC mappings of ICD-10 codes). We view this as a necessary compromise to minimize reporting burden on participating SNFs by using claims data while ensuring we obtain timely data for quality improvement. We refer readers to the SNF HAI Technical Report for more information regarding the measure's specifications and formulas used for rate calculations.[47]
Comment: One commenter did not support the measure because its testing results demonstrated moderate reliability.
Response: We used FY 2018 and 2019 data to conduct split-half reliability analyses to assess the internal consistency of the measure. Although our results showed moderate measure reliability, the MAP offered conditional support of the measure contingent upon NQF endorsement based on the above reliability results as well as other testing results.[48] Additional measure testing results revealed high reportability and usability, high variability, strong face validity, and good model discrimination.43 We plan to submit the measure for NQF endorsement in the future.
Comment: Some commenters highlighted their concerns regarding SNF HAI and COVID-19, noting the challenges they faced during the PHE, and how these challenges may impact their SNF HAI measure rates.
Response: We acknowledge the severity of the pandemic and its detrimental impact on SNFs. As included in section VII.H.3. of this final rule, we proposed that no data reflecting services provided in FY 2020 would be publicly reported, as this measure would only be publicly reported using FY 2019 and FY 2021 data. We recognize that quality data collection and reporting for services furnished during the PHE may not be reflective of their true level of performance during this time of emergency. At the same time, COVID-19 has heightened the importance of infection prevention and control programs and the need for HAI data.
Comment: One commenter linked the SNF HAI measure to health equity through the use of Medicare claims, noting that the measure should report demographic information such as race and ethnicity to shed light on potential health care disparities among SNF residents.
Response: We plan to track sex, age, race, ethnicity, and Medicare/Medicaid dual-eligibility status as part of CMS' routine monitoring and evaluation of the SNF HAI measure. This information will not be displayed on Care Compare as part of SNF HAI measure reporting, but we will take this request into consideration in our future efforts to promote health equity.
Comment: Some commenters urged CMS to provide resources, support, and trainings for quality improvement and infection prevention among SNFs. Commenters encourage CMS to work with stakeholders to consider the labor required to measure and prevent HAIs in SNFs under the critical shortage of healthcare personnel, and recommend for CMS to implement a requirement for SNFs to hire at least one person trained in infection control to be available at the facility, with their hours predicated on the number of beds.
Response: We would like to emphasize that SNFs should already be maintaining infection control programs in order to meet the quality requirements for certification in the Medicare program as outlined in the long-term care facility Requirements of Participation (RoPs). These regulations at § 483.80 require facilities to establish and maintain an infection prevention and control program, including designating one or more individual(s) as the infection preventionist who works at least part time at the facility and who is responsible for the facility's infection prevention and control program.
Comment: Other commenters urge CMS to train SNFs on best practices for reducing HAIs.
Response: We have made several resources available such as free online Start Printed Page 42480 training modules in partnership with the CDC and Quality Improvement Organizations (QIOs). The QIO program aims to increase patient safety and care coordination, and improve clinical quality by, among other things, working with providers, other stakeholders, and Medicare beneficiaries on initiatives to improve the quality of health care for Medicare beneficiaries. Several of these resources can be found on the following web pages as provided by the CDC: https://www.cdc.gov/longtermcare/prevention/index.html and https://www.cdc.gov/longtermcare/training.html. Additionally, the CMS Office of Minority Health (OMH) offers a Disparity Impact Statement as an intervention to address HAI-related disparities. This tool may be used to provide health equity technical assistance and reduce HAIs among vulnerable populations. The Disparity Impact Statement tool can be viewed at https://www.cms.gov/About-CMS/Agency-Information/OMH/Downloads/Disparities-Impact-Statement-508-rev102018.pdf.
After careful consideration of the public comments we received, we are finalizing our proposal to adopt the SNF HAI measure as a Medicare FFS claims-based measure beginning with the FY 2023 payment determination and subsequent years as proposed.
2. COVID-19 Vaccination Coverage Among Healthcare Personnel (HCP) Measure Beginning With the FY 2023 SNF QRP
a. Background
On January 31, 2020, the Secretary of the U.S. Department of Health and Human Services (HHS) declared a public health emergency (PHE) for the United States in response to the global outbreak of SARS-CoV-2, a novel (new) coronavirus that causes a disease named "coronavirus disease 2019" (COVID-19).[49] COVID-19 is a contagious respiratory infection[50] that can cause serious illness and death. Older individuals, racial and ethnic minorities, and those with underlying medical conditions are considered to be at higher risk for more serious complications from COVID-19.[51, 52] As stated in the proposed rule, as of April 4, 2021, the U.S. reported over 30 million cases of COVID-19 and over 553,000 COVID-19 deaths.[53] As of July 21, 2021, the U.S. has reported over 34 million cases of COVID-19 and over 607,000 COVID-19 deaths.[54]
Hospitals and health systems saw significant surges of COVID-19 patients as community infection levels increased.[55] In December 2020 and January 2021, media outlets reported that more than 100,000 Americans were in the hospital with COVID-19.[56]
Evidence indicates that COVID-19 primarily spreads when individuals are in close contact with one another.[57] The virus is typically transmitted through respiratory droplets or small particles created when someone who is infected with the virus coughs, sneezes, sings, talks or breathes.[58] Experts believe that COVID-19 spreads less commonly through contact with a contaminated surface.[59] According to the CDC, those at greatest risk of infection are persons who have had prolonged, unprotected close contact (that is, within 6 feet for 15 minutes or longer) with an individual with confirmed SARS-CoV-2 infection, regardless of whether the individual has symptoms.[60] Subsequent to the publication of the proposed rule, the CDC has confirmed that the three main ways that COVID-19 is spread are: (1) Breathing in air when close to an infected person who is exhaling small droplets and particles that contain the virus; (2) Having these small droplets and particles that contain virus land on the eyes, nose, or mouth, especially through splashes and sprays like a cough or sneeze; and (3) Touching eyes, nose, or mouth with hands that have the virus on them.[61] Personal protective equipment (PPE) and other infection-control precautions can reduce the likelihood of transmission in health care settings, but COVID-19 can still spread between healthcare personnel (HCP) and patients given the close contact that may occur during the provision of care.[62] The CDC has emphasized that health care settings, including long-term care settings, can be high-risk places for COVID-19 exposure and transmission.[63]
Vaccination is a critical part of the nation's strategy to effectively counter the spread of COVID-19 and ultimately help restore societal functioning.[64] On December 11, 2020, the Food and Drug Administration (FDA) issued the first Emergency Use Authorization (EUA) for a COVID-19 vaccine in the U.S.[65] Subsequently the FDA issued EUAs for additional COVID-19 vaccines. In issuing these EUAs, the FDA determined that it was reasonable to conclude that the known and potential benefits of each vaccine, when used as Start Printed Page 42481 authorized to prevent COVID-19, outweighed its known and potential risks.[66] [67] [68]
As part of its national strategy to address COVID-19, the Biden administration stated that it would work with states and the private sector to execute an aggressive vaccination strategy and has outlined a goal of administering 200 million shots in 100 days.[69] Although the goal of the U.S. government is to ensure that every American who wants to receive a COVID-19 vaccine can receive one, Federal agencies recommended that early vaccination efforts focus on those critical to the PHE response, including healthcare personnel (HCP), and individuals at highest risk for developing severe illness from COVID-19.[70] For example, the CDC's Advisory Committee on Immunization Practices (ACIP) recommended that HCP should be among those individuals prioritized to receive the initial, limited supply of the COVID-19 vaccination, given the potential for transmission in health care settings and the need to preserve health care system capacity.[71] Research suggests most states followed this recommendation,[72] and HCP began receiving the vaccine in mid-December of 2020.[73] Subsequent to the publication of the SNF PPS proposed rule, on April 8, 2021, the White House confirmed that there was sufficient vaccine supply for all Americans.[74]
HCP are at risk of carrying COVID-19 infection to patients, experiencing illness or death as a result of COVID-19 themselves, and transmitting it to their families, friends, and the general public. We believe it is important to require that SNFs report HCP vaccination in order to assess whether they are taking steps to limit the spread of COVID-19 among their HCP, reduce the risk of transmission of COVID-19 within their facilities, and to help sustain the ability of SNFs to continue serving their communities throughout the PHE and beyond. Currently, as required under the May 8, 2020 interim final rule with comment period (85 FR 27601-27602), SNFs are required to submit COVID-19 data through the CDC's NHSN Long-term Care Facility COVID-19 Module of the NHSN. Examples of data reported in the module include: Suspected and confirmed COVID-19 infections among residents and staff, including residents previously treated for COVID-19; total deaths and COVID-19 deaths among residents and staff; personal protective equipment and hand hygiene supplies in the facility; ventilator capacity and supplies available in the facility; resident beds and census; access to COVID-19 testing while the resident is in the facility; and staffing shortages. Although HCP and resident COVID-19 vaccination data reporting modules are currently available through the NHSN, the reporting of this data is voluntary.[75] Subsequent to the publication of the SNF PPS proposed rule, an interim final rule with comment period (IRC) published on May 13, 2021 entitled "Medicare and Medicaid Programs; COVID-19 Vaccine Requirements for Long-Term Care (LTC) Facilities and Intermediate Care Facilities for Individuals with Intellectual Disabilities (ICFs-IID) Residents, Clients, and Staff" (86 FR 26315-26316) (hereafter referred to as the May 2021 IFC), SNFs are required to report to the CDC's NHSN, on a weekly basis, the COVID-19 vaccination status of all residents and staff.
We also believe that publishing facility-level COVID-19 HCP vaccination rates on Care Compare would be helpful to many patients, including those who are at high-risk for developing serious complications from COVID-19, as they choose facilities from which to seek treatment. Under CMS' Meaningful Measures Framework, the COVID-19 Vaccination Coverage among Healthcare Personnel measure addresses the quality priority of "Promote Effective Prevention & Treatment of Chronic Disease" through the Meaningful Measures Area of "Preventive Care."
Therefore, we proposed a new measure, COVID-19 Vaccination Coverage among HCP to assess the proportion of a SNF's healthcare workforce that has been vaccinated against COVID-19.
b. Stakeholder Input
In the development and specification of the measure, a transparent process was employed to seek input from stakeholders and national experts and engage in a process that allows for pre-rulemaking input on each measure, under section 1890A of the Act.[76] To meet this requirement, the following opportunity was provided for stakeholder input.
The pre-rulemaking process includes making publicly available a list of quality and efficiency measures, called the Measures Under Consideration (MUC) List that the Secretary is considering adopting, through Federal rulemaking process, for use in Medicare program(s). This allows multi-stakeholder groups to provide recommendations to the Secretary on the measures included on the list. The COVID-19 Vaccination Coverage among HCP measure was included on the publicly available "List of Measures under Consideration for December 21, 2020" (MUC List).[77] Five comments were received from industry stakeholders during the pre-rulemaking process on the COVID-19 Vaccination Coverage among HCP measure, and support was mixed. Commenters generally supported the concept of the measure. However, there was concern about the availability of the vaccine and Start Printed Page 42482 measure definition for HCP, and some commenters encouraged CMS to continue to update the measure as new evidence comes in.
c. Measure Applications Partnership (MAP) Review
When the Measure Applications Partnership (MAP) PAC-LTC Workgroup convened on January 11, 2021, it reviewed the MUC List and the COVID-19 Vaccination Coverage among HCP measure. The MAP recognized that the proposed measure represents a promising effort to advance measurement for an evolving national pandemic and that it would bring value to the SNF QRP measure set by providing transparency about an important COVID-19 intervention to help limit COVID-19 infections.[78] The MAP also stated that collecting information on COVID-19 vaccination coverage among healthcare personnel and providing feedback to facilities would allow facilities to benchmark coverage rates and improve coverage in their facility, and that reducing rates of COVID-19 in healthcare personnel may reduce transmission among patients and reduce instances of staff shortages due to illness.[79]
In its preliminary recommendations, the MAP PAC-LTC Workgroup did not support this measure for rulemaking, subject to potential for mitigation.[80] To mitigate its concerns, the MAP believed that the measure needed well-documented evidence, finalized specifications, testing, and NQF endorsement prior to implementation.[81] Subsequently, the MAP Coordinating Committee met on January 25, 2021, and reviewed the COVID-19 Vaccination Coverage among Healthcare Personnel measure. In the 2020-2021 MAP Final Recommendations, the MAP offered conditional support for rulemaking contingent on CMS bringing the measure back to the MAP once the specifications are further clarified. The final MAP report is available at http://www.qualityforum.org/Publications/2021/03/MAP_2020-2021_Considerations_for_Implementing_Measures_Final_Report_-_Clinicians,_Hospitals,_and_PAC-LTC.aspx.
In response to the MAP request for CMS to bring the measure back once the specifications were further clarified, CMS met with the MAP Coordinating Committee on March 15, 2021. First, CMS and CDC clarified the alignment of the COVID-19 Vaccination Coverage among HCP with the Influenza Vaccination Coverage among HCP (NQF #0431), an NQF-endorsed measure since 2012. The COVID-19 Vaccination Coverage among HCP measure is calculated using the same approach as the Influenza Vaccination Coverage among HCP measure.[82] The approach to identifying HCPs eligible for the COVID-19 vaccination is analogous to those used in the NQF endorsed flu measure which underwent rigorous review from technical experts about the validity of that approach and for which ultimately received NQF endorsement. More recently, prospective cohorts of health care personnel, first responders, and other essential and frontline workers over 13 weeks in eight U.S. locations confirmed that authorized COVID-19 vaccines are highly effective in real-world conditions. Vaccine effectiveness of full immunization with two doses of vaccines was 90 percent.[83]
Additionally, to support the measure's data element validity, CDC conducted testing of the COVID-19 vaccination numerator using data collected through the NHSN and independently reported through the Federal Pharmacy Partnership for Long-term Care Program for delivering vaccines to long-term care facilities. These are two completely independent data collection systems. In initial analyses of the first month of vaccination, the number of HCP vaccinated in approximately 1,200 facilities which had data from both systems, the number of HCP vaccinated was highly correlated between these two systems with a correlation coefficient of nearly 90 percent in the second two weeks of reporting. Of note, assessment of data element reliability may not be required by NQF if data element validity is demonstrated.[84] To assess the validity of new performance measure score (in this case, percentage of COVID-19 vaccination coverage), NQF allows assessment by face validity (that is, subjective determination by experts that the measure appears to reflect quality of care, done through a systematic and transparent process),[85] and the MAP concurred with the face validity of the COVID-19 Vaccination Coverage among HCP measure. Materials from the March 15, 2021 MAP Coordinating Committee meeting are on the NQF website at https://www.qualityforum.org/ProjectMaterials.aspx?projectID=75367.
This measure is not NQF endorsed, but the CDC, in collaboration with CMS, plans to submit the measure for NQF endorsement in the future.
d. Competing and Related Measures
Section 1899B(e)(2)(A) of the Act requires that absent an exception under section 1899B(e)(2)(B) of the Act, each measure specified by the Secretary be endorsed by the entity with a contract under section 1890(a) of the Act, currently the National Quality Forum (NQF). In the case of a specified area or medical topic determined appropriate by the Secretary for which a feasible and practical measure has not been endorsed, section 1899B(e)(2)(B) of the Act permits the Secretary to specify a measure that is not so endorsed, as long as due consideration is given to the measures that have been endorsed or adopted by a consensus organization identified by the Secretary. The proposed COVID-19 Vaccination Coverage among HCP measure is not currently NQF endorsed and has not been submitted to the NQF for consideration, so we considered whether there are other available measures that assess COVID-19 vaccinations among HCP. After review of the NQF's consensus-endorsed measures, we were unable to identify any NQF endorsed measures for SNFs focused on capturing COVID-19 vaccination coverage of HCP, and we found no other feasible and practical measure on the topic of COVID-19 vaccination coverage among HCP. The only other vaccination coverage of HCP measure found was the Influenza Vaccination Coverage among Healthcare Personnel (NQF #0431) measure which is NQF endorsed and was adopted in the IRF QRP in the FY 2014 IRF PPS final rule (78 FR 47905 through 47906), and in the LTCH QRP in the FY 2013 IPPS/LTCH PPS final rule (77 FR 53630 through 53631). Start Printed Page 42483
Given the novel nature of the SARS-CoV-2 virus, and the significant and immediate risk it poses in SNFs, we believe it was necessary to propose the measure as soon as possible. Therefore, after consideration of other available measures that assess COVID-19 vaccination rates among HCP, we believe the exception under section 1899B(e)(2)(B) of the Act applies. This proposed measure has the potential to generate actionable data on vaccination rates that can be used to target quality improvement among SNF providers.
e. Quality Measure Calculation
The COVID-19 Vaccination Coverage among Healthcare Personnel (HCP) measure is a process measure developed by the CDC to track COVID-19 vaccination coverage among HCP in facilities such as SNFs. Since this proposed measure is a process measure, rather than an outcome measure, it does not require risk-adjustment.
The denominator would be the number of HCP eligible to work in the facility for at least one day during the reporting period, excluding persons with contraindications to COVID-19 vaccination that are described by the CDC.[86] While the SNF QRP applies to freestanding SNFs, SNFs affiliated with acute care facilities, and all non-CAH swing-bed rural hospitals, we believe it is necessary to include all HCP within the facility in the measure denominator because all HCP would have access to and may interact with SNF residents.
The numerator would be the cumulative number of HCP eligible to work in the facility for at least one day during the reporting period and who received a complete vaccination course against SARS-CoV-2. A complete vaccination course may require one or more doses depending on the specific vaccine used. The finalized measure specifications are on the CDC website at https://www.cdc.gov/nhsn/nqf/index.html.
We proposed that SNFs would submit data for the measure through the CDC/NHSN data collection and submission framework.[87] SNFs would use the COVID-19 vaccination data reporting module in the NHSN Healthcare Personnel Safety (HPS) Component to report the number of HCP eligible who have worked at the facility that week (denominator) and the number of those HCP who have received a completed COVID-19 vaccination course (numerator). SNFs would submit COVID-19 vaccination data for at least 1 week each month. If SNFs submit more than 1 week of data in a month, the most recent week's data would be used for measure calculation purposes. Each quarter, the CDC would calculate a summary measure of COVID-19 vaccination coverage from the 3 monthly modules of data reported for the quarter. This quarterly rate would be publicly reported on the Care Compare website. Subsequent to the first refresh, one additional quarter of data would be added to the measure calculation during each advancing refresh, until the point four full quarters of data is reached. Thereafter, the measure would be reported using four rolling quarters of data on Care Compare.
For purposes of submitting data to CMS for the FY 2023 SNF QRP, SNFs would be required to submit data for the period October 1, 2021 through December 31, 2021. Following the initial data submission quarter for the FY 2023 SNF QRP, subsequent compliance for the SNF QRP would be based on four quarters of such data submission. For more information on the measure's proposed public reporting period, we refer readers to section VII.H.3. of this final rule.
We invited public comment on our proposal to add a new measure, COVID-19 Vaccination Coverage among Healthcare Personnel (HCP), to the SNF QRP beginning with the FY 2023 SNF QRP.
The following is a summary of the public comments received on our proposal to add a new measure, COVID-19 Vaccination Coverage among Healthcare Personnel (HCP), to the SNF QRP beginning with the FY 2023 SNF QRP and our responses:
Comment: A number of organizations, including provider associations and patient advocacy groups, support the proposal to adopt the COVID-19 Vaccination Coverage among HCP measure for the SNF QRP. Commenters agree that the measure would help assess the degree to which SNFs are taking steps to limit the spread of COVID-19 and reduce the risk of transmission within their facilities. Commenters pointed out that public reporting of COVID-19 vaccination among HCP on Care Compare would provide consumers with important information with which to make informed decisions about the safety of a SNF. Commenters also believe the information would provide greater transparency to Federal officials and other stakeholders seeking to effectively target vaccine hesitancy, as well as provide resources related to the COVID-19 vaccines.
Response: We thank the commenters for their support and agree that the COVID-19 Vaccination among HCP measure will help assess the degree to which SNFs are taking steps to limit the spread of COVID-19 and assess the risk of transmission within their facilities. This is consistent with information published by the CDC and others, which has emphasized that healthcare settings, including SNFs, can be high-risk places for COVID-19 exposure and transmission, and notes that COVID-19 can spread among HCP and residents given the close contact that may occur during the provision of care.[88] Vaccination is a critical part of the nation's strategy to effectively counter the spread of COVID-19 and ultimately help restore societal functioning.[89] We also agree with commenters that public reporting of COVID-19 Vaccination Coverage among HCP on Care Compare would provide consumers with important information with which to make informed decisions about the safety of a SNF.
Comment: One commenter cautioned against using the data in a way that adversely impacts the nursing home workforce, including SNF HCP, but believes the reporting will assist CMS to provide targeted support and education to providers.
Response: The SNF QRP helps inform health care consumers about the quality of healthcare SNFs provide to their residents. The measure does not impose additional requirements on the HCP workforce. We agree with the commenter that public reporting of the COVID-19 Vaccination Coverage among HCP measure on Care Compare would provide consumers with important information with which to make informed decisions about the safety of a SNF.
Comment: Another commenter urged CMS to require provider reporting of other activities related to vaccination, such as whether paid leave is provided for HCP to take off from work and recover from any side effects Start Printed Page 42484 experienced after taking the vaccine, believing this would make it easier for HCP to obtain vaccination.
Response: We appreciate the commenters' suggestions to collect additional information related to vaccinations, however CMS does not presently have the statutory authority to collect information related to paid leave or the side effects experienced after taking the vaccine.
Comment: A few commenters recommended the measure should include all personnel in the facility, such as social services, dietary, and housekeeping, not just personnel who have direct contact with residents.
Response: We proposed to include all HCP within the facility, such as social services, dietary and housekeeping, and refer readers to section VI.C.2.e. of the FY 2022 SNF proposed rule and to the Instructions for Completion of the Weekly Healthcare Personnel COVID-19 Vaccination Cumulative Summary for Long-Term Care Facilities (57.219, REV 3) at https://www.cdc.gov/nhsn/forms/instr/57.219-toi-508.pdf which details all HCP included in the measure.
Comment: One commenter stated the COVID-19 Vaccination Coverage among HCP is superfluous given the fact that CMS also proposed the SNF HAI measure which they believe to be a better indicator of a SNF's overall infection prevention practices.
Response: We disagree with the commenter's statement that the COVID-19 Vaccination Coverage among HCP measure is superfluous since the measure and the SNF HAI measure each assess distinct aspects of infection prevention. The COVID-19 Vaccination among HCP measure assesses the percentage of HCP in the facility who have received a complete vaccination course for SARS-CoV-2. The SNF HAI measure assesses the percentage of healthcare acquired infections that result in a hospitalization. While it is true that the SNF HAI measure may capture a subset of the COVID-19 cases that result in hospitalization, we believe both measures are distinct and necessary to assess SNFs' practices to mitigate hospitalizations for infections. Additionally, we believe it is important for patients and caregivers to have the COVID-19 Vaccination Coverage among HCP measure data to help them more directly assess how a SNF is mitigating the risk of COVID-19 transmission.
Comment: One commenter was encouraged by the CDC's measure validity testing following the MUC formal comment period earlier this year and the measure specifications subsequently delineated by the CDC in March 2021. Given the measure's potential to generate actionable data on vaccination rates, they think it is important for CMS, in collaboration with the CDC, to continue to hone the measure as it is submitted for NQF endorsement in the future.
Response: We thank the commenter for their support and we will continue to collaborate with the CDC. The CDC, in collaboration with CMS, are planning to submit the measure for consideration in the NQF Fall 2021 measure cycle.
A number of commenters wrote in support of the measure's concept and the need to encourage widespread vaccination among HCP. However, there were also several concerns with the measure, including burden, lack of access to the vaccine, concerns of staff intimidation if they elect not to receive the vaccine, the fact that it is unknown whether a booster vaccination will be necessary, and concern that the vaccinations have not received full FDA approval. We address each of these comments separately below:
Comment: A couple of commenters spoke to the fact that COVID-19 vaccination administration has been fragmented and challenging and were concerned whether vaccine supply would remain sufficient across the nation to ensure all HCP could receive it.
Response: As part of its national strategy to address COVID-19, the current administration stated that it would work with states and the private sector to execute an aggressive vaccination strategy. The goal of the U.S. government is to ensure that every American who wants to receive a COVID-19 vaccine can receive one. While we acknowledge that vaccine supply was initially limited, more than 20 states are no longer ordering all the vaccine doses allocated to them due to decline in demand,[90] and more than 1,000 counties are reporting a surplus of vaccine appointments.[91] We understand that vaccine availability may vary based on location, and vaccination and medical staff authorized to administer the vaccination may not be readily available in all areas. Supply distribution is the responsibility of each state, and SNFs should continue to consult state and local health departments to understand the range of options for how vaccine provision can be made available to HCP.
Comment: A couple of commenters expressed concern over the potential for inequality among SNFs because one-dose vaccines are not equally available across the nation. They stated some SNFs would be at a disadvantage because of the 4-week waiting period between doses of the two-dose vaccines to reach complete vaccination status.
Response: This measure provides information to patients about the extent to which HCP have completed a COVID-19 vaccination course during a defined period of time. Given this goal, geographic variation in vaccine availability, including the types of vaccines available, ultimately does not make the information captured by this measure any less valuable to stakeholders.
Because we proposed to begin reporting the COVID-19 Vaccination Coverage among HCP measure using one quarter of data, there will be time during each quarter for persons receiving the two-dose vaccine to reach complete vaccination status. In the event that an HCP does not complete a vaccination course during a reporting period, they would still be captured when the measure is updated in the subsequent quarter, assuming the HCP remains eligible.
Comment: One commenter noted that CMS proposed a COVID-19 Vaccination Coverage among HCP measure in the FY 2022 Inpatient Prospective Payment System (IPPS) proposed rule and stated the numerator would be calculated based on HCP who received a completed vaccination course "since the vaccine was first available or on a repeated interval if revaccination is recommended." The commenter requested CMS provide clarification how evolving vaccine recommendations will be accounted for in the COVID-19 Vaccination Coverage among HCP measure proposed for the SNF QRP. Several other commenters questioned how vaccination boosters would factor into reporting requirements. Commenters stated it would be premature for CMS to adopt the measure because it is unknown how long the COVID-19 vaccination would be effective as well as whether and how often booster shots may be required. They noted that given the evolving nature of the COVID-19 virus, that information could change between the time a person receives a vaccine and the public reporting of the data. Commenters noted that these were important unanswered questions they thought would affect both the design and feasibility of any HCP vaccination Start Printed Page 42485 measure and would likely result in a change to the measure definition. Several commenters suggested CMS wait until expectations are clarified about maintaining employees' COVID-19 vaccinations.
Response: The COVID-19 Vaccination Coverage among HCP measure is a measure of a completed COVID-19 vaccination course (as proposed in section VI.C.2.e. of the FY 2022 SNF PPS proposed rule). A complete vaccination course may require one or more doses depending on the specific vaccine used. Currently, the need for COVID-19 booster doses has not been established, and no additional doses are currently recommended for HCP.[92] However, we believe that the numerator is sufficiently broad to include potential future boosters as part of a "complete vaccination course" and therefore the measure is sufficiently specified to address boosters.
Comment: We received several comments posing questions about the uncertainty the provider community, which we interpret to be SNFs, believe around the future of the COVID-19 vaccination due to the prevalence of misinformation about COVID-19 and the vaccines.
Response: We acknowledge that the science around the SARS-CoV-2 virus continues to evolve. We are still learning how effective the vaccines are against new variants of the virus that causes COVID-19, although current evidence suggests that the COVID-19 vaccines authorized for use in the United States offer protection against most variants currently spreading in the United States.[93] This is one of several reasons we proposed the COVID-19 Vaccination Coverage among HCP measure. The CDC will continue to monitor the effectiveness of the COVID-19 vaccines.
Comment: A number of commenters voiced concern that requiring SNFs to report this information for payment purposes could create incentives for SNF employers to coerce or intimidate HCP who decline the vaccine. They point out that vaccine hesitancy is a real challenge not only among the general public, but also among HCP. They note that some personnel have indicated a preference to wait until the vaccine receives full FDA approval before receiving it. These commenters expressed concern that adding the measure to the SNF QRP conflates the ability of a nursing home to overcome the independent, individual medical choices of its HCP with the ability of the nursing home to provide quality care to the residents living in the facility. Some commenters were concerned that healthcare workers who have not yet received the vaccine or who cannot for various reasons may be let go or have reduced hours based on an employer's desire for higher reporting. They point to the challenges in finding healthcare workers to meet demand, and that requiring vaccines will only make it worse. For these reasons, they believe CMS should delay implementation and public reporting until FY 2023 or remove the measure entirely.
Response: We appreciate that some HCP may have concerns about COVID-19 vaccinations, but the COVID-19 Vaccination Coverage among HCP measure does not mandate or require SNF HCP to complete a COVID-19 vaccination course in order to meet the measure's data reporting requirements. The SNF QRP is a pay-for-reporting program and the number of HCP who have been vaccinated in a SNF does not impact SNF's ability to successfully report the measure. Additionally, we believe it is important that the SNFs report COVID-19 Vaccination Coverage among HCP measure as soon as possible to assess the potential spread of COVID-19 among their HCP and assess the risk of transmission of COVID-19 within their facilities, and to help sustain the ability of SNFs to continue serving their communities throughout the PHE and beyond.
Comment: A few commenters were concerned that if SNFs were found to have "missing data," they would receive a monetary penalty or a reduction in reimbursement.
Response: The SNF QRP is a pay-for-reporting program and the measures under the SNF QRP are tools that measure or quantify healthcare processes, outcomes, patient perceptions, and organizational structure and/or systems that are associated with the ability to provide high-quality health care and/or that relate to one or more quality goals for health care. The rate of vaccination in a SNF is not tied to a SNF's Medicare payment.
To meet the reporting requirements for the COVID-19 Vaccination Coverage among HCP measure, we proposed that a SNF would have to report the cumulative number of HCP eligible to work in the SNF for at least one day during the reporting period and who received a complete vaccination course against SARS-CoV-2. SNFs would have to report data for the measure at least one week per month and could self-select the week. For SNFs that report more than 1 week per month, the last week of the reporting month will be used.
CMS' contractor sends informational messages to SNFs that are not meeting Annual Payment Update (APU) thresholds on a quarterly basis ahead of each submission deadline. Information about how to sign up for these alerts can be found on the SNF QRP Help web page at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Skilled-Nursing-Facility-Quality-Reporting-Program/SNF-Quality-Reporting-Program-QRP-Help.
Comment: A couple commenters expressed concern about unintended consequences and legal risks to their organization if HCP experience an adverse event related to vaccination, and therefore oppose adoption of the COVID-19 Vaccination Coverage among HCP measure into the SNF QRP.
Response: It is unclear what unintended consequences and legal risks the commenters are referring to. The SNF QRP is a pay-for-reporting program, and SNFs are assessed under the program based on whether they have met the SNF QRP's reporting requirements. The COVID-19 Vaccination Coverage among HCP measure does not require HCP to be vaccinated in order for SNFs to successfully report the measure under the SNF QRP.
Comment: One commenter raised concern about the possibility of a double jeopardy that would arise from the interplay of a SNF QRP measure on COVID-19 vaccination and the requirements of the interim final rule with comment period (the May 2021 IFC). They note that under the May 2021 IFC, a nursing home can be cited and receive a civil monetary penalty (CMP) for failure to report COVID-19 vaccination data for a given week, while under the SNF QRP, a SNF may incur a rate reduction for a full calendar year if it fails to meet the reporting requirements. Several other commenters echoed the same concerns.
Response: It is unclear what the commenter means by the term "double jeopardy", but we interpret it to mean that the commenter is concerned about being penalized twice for the same data Start Printed Page 42486 submission requirements. We disagree with the commenter, as the LTC facility requirements of participation at (requirements) at § 483.80(g) and the SNF QRP are two separate requirements. The LTC facility requirements require nursing homes to report weekly on the COVID-19 vaccination status of all residents and staff as well as COVID-19 therapeutic treatment administered to residents. As discussed in section VIII.C.2.e of this final rule, we proposed that SNFs would report the number of eligible HCP who have worked at the facility during 1 week of each month and the number of those HCP who have received a completed COVID-19 vaccination course. Each system has its own methods of validation and carry separate penalties. We proposed the COVID-19 Vaccination Coverage among HCP measure under the SNF QRP.
Comment: One commenter stated they did not support the adoption of the COVID-19 Vaccination Coverage among HCP measure into the SNF QRP because they believe it conflicts with the May 2021 IFC that specifies a similar measure using similar data sources.
Response: As described above, the regulations at § 483.80(g) finalized in the May 2021 IFC are for the LTC facilities' requirements, and are separate from the SNF QRP. The purpose of the proposed COVID-19 Vaccination Coverage among HCP measure is different from the vaccination information reporting requirement in the May 2021 IFC. The proposed SNF QRP COVID-19 Vaccination Coverage among HCP measure will allow for the collection of this data under the SNF QRP and subsequent public reporting of facility-level HCP vaccination rates on Care Compare so that Medicare beneficiaries can make side-by-side facility comparisons to facilitate informed decision making in an accessible and user-friendly manner. The measure's purpose is distinct from those laid out in the May 2021 IFC which are: To update the LTC facilities' requirements to address the issues of resident and staff vaccination education and the reporting of COVID-19 vaccinations and therapeutic treatments to the CDC; to ensure that all LTC facility residents and the staff that care for them are provided ongoing access to vaccination against COVID-19; to assist surveyors to determine individual facilities that may need to have focused infection control surveys; to monitor broader community uptake and to allow the CDC to identify and alert CMS to facilities that may need additional support in regards to vaccine administration and education.
Comment: One commenter stated that since the May 2021 IFC was released, they have been reporting staff and resident vaccination rates weekly via NHSN's Weekly HCP and Resident COVID-19 Vaccination Module. The proposal to add the COVID-19 Vaccination Coverage among HCP measure to the SNF QRP uses the same reporting process but at a different frequency. This commenter recommended CMS align the reporting requirements at § 483.80(g) with the COVID-19 Vaccination Coverage among HCP measure reporting requirements or explain how to manage competing requirements in different rules. Another commenter was unclear which rule they should follow. Another commenter stated they support the requirement in this rule to report monthly but are concerned that once the PHE is lifted, it would be overly burdensome to ask providers to report every week. They requested that CMS respond and explain how to manage competing requirements in different rules.
Response: The requirements finalized at § 483.80(g) are mandatory for participating in Medicare and are separate from the SNF QRP. Each of the requirements is met by reporting through the NHSN's Weekly HCP COVID-19 Vaccination Module. We are clarifying that a SNF that submits four weeks of data to meet the requirements of participation at § 483.80(g) would also meet the data submission requirement for the COVID-19 Vaccination Coverage among HCP for the SNF QRP.
Comment: A number of commenters stated it is premature to begin tracking COVID-19 vaccinations because the COVID-19 vaccines are authorized through an EUA and do not have full FDA approval at this time. One commenter acknowledged that they were confident in the safety and efficacy of the three current vaccines but still finds it to be incongruous to adopt a measure into Federal Quality Reporting Programs that assess the use of a product that has not yet received full Federal approval. Several commenters stated the measure should not be adopted until full approval by FDA across all existing submitted vaccines under EUAs. Another commenter stated that until FDA approves the vaccines, they do not have control over the vaccination status of their employees.
Response: The COVID-19 vaccines are authorized by the FDA for use through an Emergency Use Authorization (EUA). We refer readers to the FDA website for additional information related to FDA process for evaluating an EUA request at https://www.fda.gov/vaccines-blood-biologics/vaccines/emergency-use-authorization-vaccines-explained. The Equal Employment Opportunity Commission (EEOC) released updated and expanded technical assistance on May 28, 2021.[94] Specifically the EEOC stated the Federal equal employment opportunity (EEO) laws do not prevent an employer from requiring all employees physically entering the workplace to be vaccinated for COVID-19, so long as the employer complies with the reasonable accommodation provisions of the Americans with Disabilities Act (ADA) and Title VII of the Civil Rights Act of 1964 and other EEO considerations. In addition, FDA is closely monitoring the safety of the COVID-19 vaccines authorized for emergency use. We believe that due to the continued PHE and the ongoing risk of infection transmissions in the SNF population, the benefits of finalizing this measure in this year's final rule are essential for patient safety.
Comment: We received numerous comments requesting that CMS delay the adoption of the COVID-19 Vaccination Coverage among HCP measure until it has received NQF endorsement. Commenters were concerned that since the measure has not been fully specified, tested, or endorsed by the NQF, then it may not be thoroughly tested and vetted, and may impact patients' certainty that the data they rely on are reliable. Other commenters included language from the Post-Acute Care/Long-term Care Workgroup (Workgroup) of the Measures Application Partnership (MAP) meeting transcript to support their position. They all urged the agency, in addition to seeking NQF endorsement, to fully develop and test the measure for reliability and validity before implementing it in the SNF QRP.
Response: Given the novel nature of the SARS-CoV-2 virus, and the significant and immediate health risk it poses in SNFs, we believe it is necessary to adopt this measure as soon as possible. Additionally, given the results from CDC's preliminary validity testing of the data elements required for the measure numerator (described further in section VI.C.2.c. of the FY 2022 SNF PPS proposed rule), the alignment between the denominator of this measure and the denominator of the Influenza Vaccination among HCP Start Printed Page 42487 measure (NQF#0431), and the MAP's determination that the measure has face validity, CMS proposes the COVID-19 Vaccination Coverage among HCP measure beginning with the FY 2023 SNF QRP. As noted previously, the CDC, in collaboration with CMS, are planning to submit the measure for consideration in the NQF Fall 2021 measure cycle.
Comment: A commenter stated they did not believe CMS had the statutory authority to add the COVID-19 Vaccination Coverage among HCP measure to the SNF QRP. The commenter went on to state that section 1899B(a)(1)(B) of the IMPACT Act is intended to support interoperable patient care measures to compare outcomes across post-acute provider settings. They do not believe the proposed staff vaccination measure is a patient care measure.
Response: We believe the commenter is referring to section 1899B(a)(1)(B) of the Act. We disagree with the commenter that we lack the statutory authority to propose this measure. Section 1899B(d)(1) of the Act requires the Secretary to specify resource use and other measures. Section 1899B(a)(1)(B) requires, in part, that data on resource use and other measures under section 1899B(d)(1) of the Act facilitate coordinated care and improve Medicare beneficiary outcomes. Remaining COVID-19 free while receiving SNF care is critically important for Medicare beneficiaries, and thus a measure that increases the likelihood of this outcome would be considered a patient care measure. As illustrated in Medicare claims and encounter data,[95] the number of Medicare beneficiaries hospitalized with COVID-19 in the last week of December 2020 was over 50,000, and the number of COVID-19 cases exceeded 4.3 million as of April 24, 2021. We believe that the toll the COVID pandemic has taken on Medicare beneficiaries demonstrates the need for increased action to mitigate the effects of the ongoing pandemic.
Section 1899B(a)(1)(B) of the Act also requires, in part, that data on resource use and other measures under section 1899B(d)(1) of the Act be standardized and interoperable so as to allow for the exchange of such data among PAC providers, including SNFs. We have proposed the COVID-19 Vaccination Coverage among HCP measure under the IRF QRP in the FY 2022 IRF PPS proposed rule (86 FR 19105 through 19108), and the LTCH QRP under the FY 2022 IPPS/LTCH PPS proposed rule (86 FR 25610 through 25613) consistent with these requirements. Further, this measure would facilitate patient care and care coordination during the discharge planning process. A discharging hospital or facility, in collaboration with the patient and family, could use this measure to coordinate care and ensure patient preferences are considered in the discharge plan. Patients at high risk for negative outcomes due to COVID-19 (perhaps due to underlying conditions) can use healthcare provider vaccination rates when they are selecting a SNF for next-level care.
Comment: A commenter noted that CMS, to date, has restricted all measures developed under section 1899B(a)(1)(B) of the Act to include only Medicare beneficiaries accessing their post-acute care benefit to align with the other post-acute care settings. They recommended not finalizing the COVID-19 Vaccination Coverage among HCP measure because it is not restricted to staff providing care to post-acute care residents and would be nearly impossible to collect.
Response: To date, we have developed measures under section 1899B of the Act to include only Medicare beneficiaries accessing their post-acute care benefit. We proposed the measure as specified by the CDC, which includes all of the staff within the facility because all staff within the facility place patients receiving post-acute care (including SNF residents) at risk for getting COVID-19. This is true whether or not they are providing direct care to post-acute care patients.
In regard to the comment about the near impossibility of collecting information exclusively among staff providing care to post-acute care residents, we agree. This is one of the reasons why the measure is specified to capture the information on all healthcare staff in the SNF, including personnel, such as dietary staff, administrators, or social workers. While it may be easy to identify SNF direct care staff who provide care to SNF residents, it would be nearly impossible to ensure other personnel, such as dietary staff, administrators, or social workers, interact exclusively with SNF patients.
Comment: We heard from several commenters who found the COVID-19 Vaccination Coverage measure among HCP was not aligned with the Influenza Vaccination Coverage among HCP (NQF #0431) measure as CMS stated in the proposed rule. They pointed out that circumstances around the use of the COVID-19 vaccine are not entirely comparable to those of the influenza vaccine.
Response: We agree that there are key differences between the Influenza Vaccination among HCP measure and the COVID-19 Vaccination Coverage among HCP measure. We acknowledge that even though the CDC modeled the COVID-19 Vaccination Coverage among HCP measure after the Influenza Vaccination among HCP measure, FDA-approved influenza vaccines and the authorized COVID-19 vaccines differ in multiple ways. The reporting requirements for the numerator of the COVID-19 Vaccination Coverage among HCP measure that one commenter listed are due to the fact that some COVID-19 vaccines require two doses to reach full vaccination status, while some COVID-19 vaccines require only one dose. The measures are aligned with respect to the reporting mechanism used to report data (the NHSN) and key components of the measure specifications (for example, the definition of the denominator), but the measures allow for important differences to reflect the reality that the circumstances around vaccine administration (that the commenter points out) are not identical.
Comment: Several commenters pointed to the fact that SNFs have many questions about the specifics of the COVID-19 Vaccination Coverage among HCP measure such as what the long-term plans for using the measure in the SNF QRP are. Another commenter thought the measure seemed unnecessary based on the current vaccination push and the fact that due to the Federal Vaccination Schedule, healthcare workers would already have received the vaccination. This commenter did not believe it addressed many of the unknowns still ahead regarding the virus.
Response: We interpret the commenter's reference to the "Federal Vaccination Schedule" to be referring to the eligibility criteria during the initial rollout of the COVID-19 vaccine. When the U.S. supply of COVID-19 vaccine was limited, CDC provided recommendations to Federal, state, and local governments about who should be vaccinated first. While CDC made recommendations for who should be offered the COVID-19 vaccines first, each state had its own plan. CMS acknowledges that healthcare workers were given priority in receiving the vaccine, but as reported by Medscape Start Printed Page 42488 Medical News on June 28, 2021,[96] Federal data show that one in four hospital workers across the United States are still unvaccinated, and only one in every three hospital workers are vaccinated in the nation's 50 largest health systems. We believe it is critical to measure staff vaccination rates among SNFs even as vaccinations become more common, especially in light of the vaccine hesitancy other comments have pointed out.
In response to the comment asking about the long-term plans for using the measure, as described in sections VII.C.2.e and VII.H.3. of this final rule, we proposed to adopt the COVID-19 Vaccination Coverage among HCP measure into the SNF QRP and publicly report on SNF performance. Once a measure is adopted under the SNF QRP, the measure will remain in effect until CMS proposes that it be removed, suspended, or replaced. We refer readers to the FY 2016 SNF PPS final rule (80 FR 46431 through 46432) for details on this policy.
Comment: A commenter questioned whether the COVID-19 Vaccination among HCP measure aligned with the Merit-based Incentive Payment System (MIPS) measure that was reviewed by the MAP and assesses patients who received at least one dose (in addition to a complete course).
Response: We understand the commenter to be questioning whether this measure is similar to the measure considered for another quality reporting program, the Merit-based Incentive Payment System (MIPS) for clinicians. If so, MUC—0045, the SARS-Co-V-2 Vaccination by Clinician measure differs from the COVID-19 Vaccination Coverage among HCP measure. Most notably, the SARS-CoV-2 Vaccination by Clinician measure assesses the proportion of patients who received at least one SARS-CoV-2 vaccination while the COVID-19 Vaccination Coverage among HCP measure assesses the proportion of HCP who complete a SARS-CoV-2 vaccination course.
Comment: Commenters pointed out that the Influenza Vaccination Coverage among HCP (NQF #0431) measure utilizes providers working in the facility for the denominator whereas the proposed COVID-19 metric utilizes providers eligible to work in the facility. Several commenters requested that CMS revise the COVID-19 Vaccination Coverage among HCP measure denominator to include eligible providers who have worked at the facility during the period being measured, similar to the influenza measure. The commenters believe this would be important due to differences across states as to whom would be considered "eligible" to work due to laws such as the Family Medical Leave Act (FMLA) and state-level laws associated with defining employee status.
Response: As described in section VII.G.3. of this final rule, we proposed the COVID-19 Vaccination Coverage among HCP measure to include HCP who work regularly in the SNF, and to require SNFs to use the specifications and data collection tools for the proposed COVID-19 Vaccination Coverage among HCP as required by CDC as of the time that the data are submitted. Subsequent to the publication of the FY 2022 SNF PPS proposed rule on April 8, 2021, the CDC released the Instructions for Completion of the Weekly Healthcare Personnel COVID-19 Vaccination Cumulative Summary for Long-Term Care Facilities (57.219, REV3) which are available at https://www.cdc.gov/nhsn/forms/instr/57.219-toi-508.pdf . The document defines HCP eligible to have worked to include those scheduled to work in the facility at least one day every week. The document instructs SNFs to count any HCP working part of a day, as well as those that may be on temporary leave during the week of data collection. Temporary leave was further defined as less than or equal to 2 weeks in duration. Because the measurement period covered by the Influenza Vaccination Coverage among HCP (NQF #0431) measure is quite long (the entire 6 month influenza season), such absences do not impact the Influenza Vaccination Coverage among HCP (NQF #0431) measure denominator. However, in order to provide more timely measurement of COVID-19 vaccination coverage while also reducing the burden of data collection for SNFs, we proposed the measurement period of the COVID-19 Vaccination among HCP measure to be only one week, considerably shorter than the time period covered by the Influenza Vaccination Coverage among HCP (NQF #0431) measure, and a number of regularly working HCP who would be counted within the 6-month period of the Influenza Vaccination Coverage Measure may be absent during this shortened period. Therefore, HCP who regularly work in the SNF, but may be temporarily absent for up to 2 weeks, are still to be included in the COVID-19 Vaccination Coverage among HCP measure as these regular workers will be working during other weeks of the reporting month. While differences may exist across states in employment eligibility definitions, the CDC definition for purposes of this measure includes HCP eligible to have worked and scheduled to work in the facility at least one day during the week of data collection. This approach provides a consistent definition of eligibility which is necessary for national and regional data analyses.
Comment: One commenter provided several recommendations for revising the denominator of the COVID-19 Vaccination Coverage among HCP measure. They stated there are several contraindications or exclusions that go beyond allergies to the ingredients of the vaccine, and therefore these persons should be excluded from the denominator as well. They specifically point to individuals who have been vaccinated within the last 2 weeks and individuals who have received monoclonal antibody or another COVID-19 therapy and individuals with an active COVID-19 infection as persons who should be excluded from the measure. They also urged CMS to ensure that the regulatory language has the flexibility to accommodate these and any future changes.
Response: We thank the commenter for the recommendations. The CDC website describes a number of clinical considerations for the use of COVID-19 vaccines on its website at https://www.cdc.gov/vaccines/covid-19/downloads/summary-interim-clinical-considerations.pdf. These considerations are separate from the contraindications to the vaccines. Contraindications to the vaccines can be found in the FDA Fact Sheets for the authorized COVID-19 vaccines, which are accessible through the FDA web pages for those vaccines.[97 98 99] Therefore, we disagree with the commenter and do not believe the definition of the denominator needs to be changed.
Comment: One commenter stated that if CMS proceeded with finalizing the measure, they strongly encourage the agency to consider including all HCP in the denominator, at least for an initial reporting period and to allow for Start Printed Page 42489 consistent cross-provider reporting and accurate measurement and comparisons. They also stated CMS should include a clear explanation in public reporting that the measure includes HCP with contraindications.
Response: We interpret the commenter to be stating that the denominator should include HCP with and without contraindications to the vaccination. We believe that excluding HCP with contraindications from the measure strikes an appropriate balance between obtaining accurate estimates of vaccine rates among HCP within SNFs and not holding a SNF accountable for HCP with a COVID-19 vaccination contraindication, as the number of HCP with contraindications or exclusions from vaccination is expected to be low.
Comment: One commenter raised a question about guidance to state survey agencies found in QSO-21-19-NH.[100] In it, they pointed out a discrepancy in how CMS defined "staff" for COVID-19 vaccination reporting and the definition provided for HCP under the proposed quality measure. They are concerned about the confusion it will cause providers.
Response: We interpret the commenter's point to be about the definitions for purposes of reporting data to the NHSN to meet the LTC facility requirements at § 483.80(g) and the requirements for the SNF QRP. Our May 11, 2021 guidance, QSO-21-19-NH, defines "staff" to mean individuals who work in the facility on a regular (that is, at least once a week) basis, including individuals who may not be physically in the LTC facility for a period of time due to illness, disability, or scheduled time off, but who are expected to return to work. This also includes individuals under contract or arrangement, including hospice and dialysis staff, physical therapists, occupational therapists, mental health professionals, or volunteers, who are in the facility on a regular basis, as the vaccine is available. The instructions for completing the NHSN Weekly Healthcare Personnel COVID-19 Vaccination Cumulative Summary for Long-Term Care Facilities[101] defines "Number of HCP that were eligible to have worked at this facility for at least 1 day during the week of data collection" to include employees, contractors, or students, trainees, and volunteers who are scheduled to work in the facility at least one day every week. Working any part of a day is considered as working 1 day. HCP are to be included even if they are on temporary leave during the week of data collection. Temporary leave is defined as less than or equal to 2 weeks in duration. Examples of temporary leave may include sick leave or vacation. In instances where temporary leave extends past 2 weeks, the healthcare worker should not be included in question #1 for the current week of data collection. We believe the NHSN instructions to be a clarification of the QSO-21-19-NH memo, provided to facilitate completion of the module in a consistent manner.
Comment: One commenter had questions on what "fully vaccinated" meant.
Response: The term "fully vaccinated" is not used in the proposed COVID-19 Vaccination Coverage among HCP measure. We proposed the numerator for the COVID-19 Vaccination Coverage among HCP measure to include a complete vaccination course as defined in section VI.C.2.e. of the FY 2022 SNF PPS proposed rule. We refer the commenter to the CDC's website where the term "fully vaccinated" is defined at https://www.cdc.gov/coronavirus/2019-ncov/vaccines/fully-vaccinated.html.
After careful consideration of the public comments we received, we are finalizing our proposal to adopt the COVID-19 Vaccination Coverage among Healthcare Personnel (HCP) measure beginning with the FY 2023 SNF QRP as proposed.
3. Update to the Transfer of Health (TOH) Information to the Patient—Post-Acute Care (PAC) Measure Beginning With the FY 2023 SNF QRP
We proposed to update the Transfer of Health Information to the Patient—Post-Acute Care (PAC) measure denominator to exclude residents discharged home under the care of an organized home health service or hospice. This measure assesses for and reports on the timely transfer of health information, specifically transfer of a medication list. We adopted this measure in the FY 2020 SNF PPS final rule (84 FR 38761 through 38764) beginning with the FY 2022 SNF QRP. It is a process measure that evaluates for the transfer of information when a resident is discharged from his or her current PAC setting to a private home/apartment, board and care home, assisted living, group home, transitional living, or home under the care of an organized home health service organization or hospice.
This measure, adopted under section 1899B(c)(1)(E) of the Act, was developed to be a standardized measure for the IRF QRP, LTCH QRP, SNF QRP, and Home Health (HH) QRP. The measure is calculated by one standardized data element that asks, "At the time of discharge, did the facility provide the resident's current reconciled medication list to the resident, family, and/or caregiver?" The discharge location is captured by items on the Minimum Data Set (MDS).
Specifically, we proposed to update the measure denominator. Currently, the measure denominators for both the TOH-Patient and the TOH-Provider measure assess the number of residents discharged home under the care of an organized home health service organization or hospice. In order to align the measure with the IRF QRP, LTCH QRP and HH QRP and avoid counting the resident in both TOH measures in the SNF QRP, we proposed to remove this location from the definition of the denominator for the TOH-Patient measure. Therefore, we proposed to update the denominator for the TOH-Patient measure to only discharges to a private home/apartment, board and care home, assisted living, group home, or transitional living. For additional technical information regarding the TOH-Patient measure, we refer readers to the document titled "Final Specifications for SNF QRP Quality Measures and Standardized Patient Assessment Data Elements" available at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Downloads/Final-Specifications-for-SNF-QRP-Quality-Measures-and-SPADEs.pdf.
We invited public comment on our proposal to update the denominator of the Transfer of Health (TOH) Information to the Patient—Post-Acute Care (PAC) measure (TOH-Patient-PAC measure) beginning with the FY 2023 SNF QRP.
The following is a summary of the public comments received on our proposal to update the denominator of the TOH Information to the Patient—PAC measure beginning with the FY 2023 SNF QRP and our responses:
Comment: We received overwhelming support for our proposal to update the TOH-Patient-PAC measure's denominator to remove the inclusion of "home under care of an organized home health service organization or hospice." Provider and trade associations agreed that the update will reduce denominator redundancy in the two TOH Start Printed Page 42490 Information—PAC measures. One commenter stated that the update will provide a refined measure that more accurately accounts for the SNF's performance in this area. A few commenters also were appreciative of CMS' review of measures to reduce unnecessary provider burden.
Response: We appreciate the commenters' support.
Comment: A few commenters stated that it was premature to introduce this measure beginning with the FY 2023 SNF QRP since the assessment data would not be available to calculate performance. Since the TOH-Patient measure requires the use of MDS item A2105—Discharge Status, an item that is currently not available on the assessment tool used by SNFs (the MDS V1.17.2) commenters did not believe the information could be collected. They noted that in the IFC published on May 8, 2020 entitled "Medicare and Medicaid Programs, Basic Health Program, and Exchanges; Additional Policy and Regulatory Revisions in Response to the COVID-19 Public Health Emergency and Delay of Certain Reporting Requirements for the Skilled Nursing Facility Quality Reporting Program" (85 FR 27550), CMS delayed collection of MDS item A2105—Discharge Status until a particular point in time after the PHE has ended. Therefore, commenters requested that CMS consider reinstating the delay of this measure as originally stated in the May 8, 2020 IFC.
Response: We acknowledge that the current version of the MDS, MDS 3.0 v1.17.2, which SNFs use to submit data to meet the requirements of the SNF QRP, does not currently include the data elements needed to report the TOH-Patient-PAC measure which we finalized for data collection beginning October 1, 2020 (84 FR 38761 through 38764). In the May 8, 2020 IFC (85 FR 27550), we delayed data collection for certain SNF QRP items, including the MDS item A2105, until the October 1 date that is at least two full fiscal years after the end of the PHE for COVID-19. However, because it is uncertain when the PHE will end, we proposed to make the measure denominator specification change effective FY 2023. Therefore, when the PHE ends, and the MDS item A2105—Discharge Status collection begins, the measure update would already be in place.
Comment: One commenter opposed our proposal to update the denominator specifications for the TOH-Patient-PAC measure. The commenter was concerned that revising the denominator would remove the responsibility of the SNF to provide the medication list to the "patient, family, or caregiver" when the patient is transferred to home health or hospice providers. The commenter believes that the current medication list should be provided to the resident and family/caregivers regardless of the discharge location because family caregivers are often involved in assisting the person they are caring for with their medications.
Response: The TOH-Patient-PAC data element under the TOH-Patient-PAC measure asks about the transfer of a reconciled medication list to the patient, family, and/or caregiver. While residents discharged home under the care of an organized home health service organization or hospice will no longer be included in the denominator of the TOH-Patient-PAC measure to reduce redundancy with the TOH-Provider-PAC measure, we acknowledge the importance of family and/or caregivers and encourage care collaboration between the SNF and the family or caregiver when authorized by the patient. SNFs are required under § 483.21(c)(2)(iii) to provide a resident at discharge with a discharge summary that includes, but is not limited to, reconciliation of all pre-discharge medications with the resident's post-discharge medications (both prescribed and over-the-counter). We refer the commenter to the FY 2020 SNF PPS final rule (84 FR 38761 through 38764) for additional information about this process measure.
Comment: One commenter requested clarity on the measure and the problem CMS is aiming to resolve.
Response: We refer the reader to the FY 2020 SNF PPS proposed and final rules (84 FR 17638 through 17643 and 84 FR 38761 through 38764, respectively) where the TOH-Patient-PAC measure was proposed and finalized. For additional technical information regarding the TOH-Patient-PAC measure, we refer readers to the document titled "Final Specifications for SNF QRP Quality Measures and Standardized Patient Assessment Data Elements" available at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Downloads/Final-Specifications-for-SNF-QRP-Quality-Measures-and-SPADEs.pdf.
We refer the reader to section VI.C.3. of the FY 2022 SNF proposed rule where we described the issue this proposal addresses. Currently, the measure denominators for both the TOH-Patient and the TOH-Provider measure assess the number of residents discharged home under the care of an organized home health service organization or hospice. In order to align the measure with the IRF QRP, LTCH QRP and HH QRP and avoid counting the resident in both TOH measures in the SNF QRP, we proposed to remove this location from the definition of the denominator for the TOH-Patient measure.
After careful consideration of the public comments we received, we are finalizing our proposal to update the denominator for the Transfer of Health (TOH) Information to the Patient-Post-Acute Care (PAC) measure under section 1899B(c)(1)(E) of the Act beginning with the CY 2023 SNF QRP as proposed.
D. SNF QRP Quality Measures Under Consideration for Future Years: Request for Information (RFI)
We solicited input on the importance, relevance, appropriateness, and applicability of each of the measures and concepts under consideration listed in Table 25 for future years in the SNF QRP.

Start Printed Page 42491
We received several comments on this RFI, which are summarized below:
Comment: Most commenters supported the inclusion of all the proposed measures listed in Table 25. One commenter stated that all of the measures and measure concepts are important and relevant for assessing quality of care delivered to SNF patients.
Many commenters supported the concept of frailty, and one commenter stated that frailty assessments provide a means of identifying older adults most vulnerable to adverse health outcomes.
Commenters were generally supportive of the measure concept for shared decision-making process and pointed out it was important to ensuring care delivered in a SNF was in line with the person's goals and values. Other commenters questioned how it could be captured in the SNF QRP. One commenter shared concerns about using shared decision-making as a quality measure, and recommended CMS only use claims-based quality measures.
Several commenters supported the concept of patient reported outcomes (PROs) while others were uncertain what CMS intends with the term patient reported outcomes. One commenter stressed the importance of PROs since they determine outcomes based on information obtained directly from patients, and therefore provide greater insight into patients' experience of the outcomes of care. Another commenter echoed that and stated that patients and caregivers are the best sources of information reflecting the totality of the patient experience.
Several commenters were supportive of the inclusion of pain management quality measures because pain is a common occurrence with SNF residents and may be under recognized and undertreated. One commenter stated that the development of an appropriate pain assessment and pain management processes measure is a clinically challenging domain that requires much more attention. Another commenter agreed stating that it is an area to focus on since given the current opioid epidemic, appropriate pain management has become a delicate and challenging subject.
Commenters were generally supportive of the concept of health equity in quality measurement. They agree that closing the health equity gap is essential to ensure optimal health services and outcomes to all Americans regardless of individual characteristics, and one commenter noted that health equity is a vital quality measure to ensure that long term care is equal for all residents.
A couple of commenters encouraged CMS to remove topped out measures and low occurrence measures to ensure it remains relevant to quality and performance. Commenters also suggested other concepts for quality measurement in the SNF QRP such as: Nutritional status, cognitive status, and advance directives.
Response: We appreciate the input provided by commenters. While we will not be responding to specific comments submitted in response to this RFI in this final rule, we intend to use this input to inform our future measure development efforts.
E. Fast Healthcare Interoperability Resources (FHIR) in Support of Digital Quality Measurement in Quality Programs—RFI
1. Solicitation of Comments
We sought input on the following steps that would enable transformation of CMS' quality measurement enterprise to be fully digital.
- What EHR/IT systems do you use and do you participate in a health information exchange (HIE)?
- How do you currently share information with other providers?
- In what ways could we incentivize or reward innovative uses of health information technology (IT) that could reduce burden for post-acute care settings, including but not limited to SNFs?
- What additional resources or tools would post-acute care settings, including but not limited to SNFs, and health IT vendors find helpful to support the testing, implementation, collection, and reporting of all measures using FHIR standards via secure APIs to reinforce the sharing of patient health information between care settings?
- Would vendors, including those that service post-acute care settings, such as SNFs, be interested in or willing to participate in pilots or models of alternative approaches to quality measurement that would align standards for quality measure data collection across care settings to improve care coordination, such as sharing patient data via secure FHIR API as the basis for calculating and reporting digital measures?
While we will not be responding to specific comments submitted in response to this RFI in this final rule, we appreciate all of the comments on and interest in this topic. We believe that this input is very valuable in the continuing development of our transition to digital quality measurement in CMS quality programs. We will continue to take all comments into account as we develop future regulatory proposals or future subregulatory policy guidance for our digital quality measurement efforts.
F. Closing the Health Equity Gap in Post-Acute Care Quality Reporting Programs—RFI
1. Solicitation of Public Comment
Under authority of the IMPACT Act and section 1888(e)(6) of the Act, we solicited comment on the possibility of revising measure development, and the collection of other Standardized Patient Assessment Data Elements that address gaps in health equity in the SNF QRP. Any potential health equity data collection or measure reporting within a CMS program that might result from public comments received in response to this solicitation would be addressed through a separate notice-and-comment rulemaking in the future.
Specifically, we invited public comment on the following:
- Recommendations for quality measures, or measurement domains that address health equity, for use in the SNF QRP.
- As finalized in the FY 2020 SNF PPS final rule (84 FR 38805 through 38817), SNFs must report certain standardized patient assessment data elements on SDOH, including race, ethnicity, preferred language, interpreter services, health literacy, transportation and social isolation.[102] We solicited guidance on any additional items, including standardized patient assessment data elements that could be used to assess health equity in the care of SNF residents, for use in the SNF QRP.
- Recommendations for how CMS can promote health equity in outcomes among SNF residents. For example, we are interested in feedback regarding whether including facility-level quality measure results stratified by social risk factors and social determinants of health (for example, dual eligibility for Medicare and Medicaid, race) in confidential feedback reports could allow facilities to identify gaps in the quality of care they provide. (For example, methods similar or analogous to the CMS Disparity Methods[103] which provide hospital-level confidential results stratified by dual eligibility for condition-specific readmission measures, which are currently included in the Hospital Readmission Reduction Start Printed Page 42492 Program (see 84 FR 42496 through 42500)).
- Methods that commenters or their organizations use in employing data to reduce disparities and improve patient outcomes, including the source(s) of data used, as appropriate.
- Given the importance of structured data and health IT standards for the capture, use, and exchange of relevant health data for improving health equity, the existing challenges providers' encounter for effective capture, use, and exchange of health information, including data on race, ethnicity, and other social determinants of health, to support care delivery and decision making.
While we will not be responding to specific comments submitted in response to this Health Equity RFI in this final rule, we appreciate all of the comments and interest in this topic. We will continue to take all concerns, comments, and suggestions into account as we continue work to address and develop policies on this important topic. It is our hope to provide additional stratified information to providers related to race and ethnicity if feasible. The provision of stratified measure results will allow PAC providers to understand how they are performing with respect to certain patient risk groups, to support these providers in their efforts to ensure equity for all of their patients and to identify opportunities for improvements in health outcomes.
G. Form, Manner, and Timing of Data Submission Under the SNF QRP
1. Background
We refer readers to the regulatory text at 42 CFR 413.360(b) for information regarding the current policies for reporting SNF QRP data.
2. Schedule for Data Submission of the SNF HAI Measure Beginning With the FY 2023 QRP
The SNF HAI measure, which we discuss in section VII.C.1. of this final rule, is a Medicare FFS claims-based measure. Because claims-based measures can be calculated based on data that have already been submitted to the Medicare program for payment purposes, no additional information collection would be required from SNFs. We proposed to use 1 year of FY 2019 claims data (October 1, 2018 through September 30, 2019) for the FY 2023 SNF QRP. We proposed to use FY 2019 data to calculate this measure because it is the most recent fiscal year of data that has not been exempted due to the PHE. Beginning with the FY 2024 SNF QRP, compliance with APU reporting requirements would use FY 2021 claims data (October 1, 2020 through September 30, 2021) and advance by one FY with each annual refresh. Due to the fact that Q1 and Q2 2020 data were excepted by CMS related to the COVID-19 PHE, these quarters of data would not be used for purposes of the QRP. For information on public reporting of the SNF HAI measure, we refer you to Table 29 in section VII.H.4.c. of this final rule.
We invited public comment on this proposal.
The following is a summary of the public comments received on the proposed Schedule for Data Submission of the SNF HAI measure beginning with the FY 2023 QRP and our responses:
Comment: One commenter was supportive of the measure's schedule for data submission.
Response: We thank this commenter for their support of the SNF HAI data submission schedule.
Comment: Another commenter supported the collection of SNF HAI data, but does not want CMS to report it publicly until the PHE has expired.
Response: We thank this commenter for their support. Any comments related to SNF HAI public reporting will be addressed in section VII.H.2. of this final rule.
After careful consideration of the public comments we received, we are finalizing the proposed schedule for data submission of the SNF HAI measure beginning with the FY 2023 SNF QRP as proposed.
3. Method of Data Submission for COVID-19 Vaccination Coverage Among Healthcare Personnel (HCP) Measure
As discussed in section VII.C.2 of this final rule, we proposed to require that SNFs submit data on the COVID-19 Vaccination Coverage among HCP measure through the Centers for Disease Control and Prevention (CDC)/National Healthcare Safety Network (NHSN). The NHSN is a secure, internet-based surveillance system maintained by the CDC that can be utilized by all types of healthcare facilities in the United States, including acute care hospitals, long-term acute care hospitals, psychiatric hospitals, rehabilitation hospitals, outpatient dialysis centers, ambulatory surgery centers, and SNFs. The NHSN enables healthcare facilities to collect and use vaccination data, and information on other adverse events. NHSN collects data via a Web-based tool hosted by the CDC (http://www.cdc.gov/). The NHSN is provided free of charge. We proposed for SNFs to submit the data needed to calculate the COVID-19 Vaccination Coverage among Healthcare Personnel measure using the NHSN's standard data submission requirements. CDC/NHSN requirements include adherence to training requirements, use of CDC measure specifications, data element definitions, data submission requirements and instructions, data submission timeframes, as well as NHSN participation forms and indications to CDC allowing CMS to access data for this measure for the SNF quality reporting program purposes. Detailed requirements for NHSN participation, measure specifications, and data collection can be found at http://www.cdc.gov/nhsn/. We proposed to require SNFs to use the specifications and data collection tools for the proposed COVID-19 Vaccination Coverage among Healthcare Personnel measure as required by CDC as of the time that the data are submitted.
We invited public comment on this proposal. The following is a summary of the public comments received on the proposed Method of Data Submission for COVID-19 Vaccination Coverage among Healthcare Personnel measure and our responses:
Comment: One commenter requested that CMS provide further information on how reporting to a system maintained by the CDC would be shared with CMS for purposes of determining SNF QRP reporting compliance. They questioned how the SNF QRP compliance rate would be calculated since the measure is not submitted through the MDS. Another commenter recommended the use of the COVID-19 Module of the NHSN to report healthcare employee vaccination rates, rather than requiring a separate reporting process through the SNF QRP.
Response: We interpret the commenter to be referring to the SNF QRP reporting requirements for the SNF Annual Payment Update (APU). As explained in section VII.G.3. of this final rule, the mechanism through which the data for calculating the COVID-19 Vaccination Coverage among HCP measure would be the Weekly Healthcare Personnel COVID-19 Vaccination Cumulative Summary for Long-Term Care Facilities Module[104] of the NHSN. There is no "separate" submission system. The NHSN collects the data submitted by SNFs, calculates the summary score, and transmits the information to CMS on a quarterly basis. CMS would use that information to determine whether a SNF has met the Start Printed Page 42493 SNF QRP reporting requirements for the COVID-19 Vaccination among HCP measure.
Comment: One commenter raised concerns about implementing a measure based on NHSN data. They explained that SNFs have experienced problems in the past year using the NHSN for reporting COVID-19 related data because they were unaware that they had made errors. They stated there was no process in place for SNF providers to receive feedback on data submissions and correct any errors before the data was made public and assessed. Given the importance of identifying potential errors and making corrections, they are concerned SNFs will be unfairly penalized.
Response: SNFs will have access to provider reports on their NHSN measure performance prior to the submission deadline. Additionally, CMS' contractor sends informational messages to SNFs that are not meeting Annual Payment Update (APU) thresholds on a quarterly basis ahead of each submission deadline. Information about how to sign up for these alerts can be found on the SNF QRP Help web page at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Skilled-Nursing-Facility-Quality-Reporting-Program/SNF-Quality-Reporting-Program-QRP-Help.
Comment: Several commenters expressed concerns about the administrative burden associated with reporting of the measure through NHSN and other systems. They pointed to other reporting systems being used around the country and stated that this would be duplicative reporting. Several commenters referenced the Department of Health and Human Services TeleTracking system, and various state agencies and databases. They stated that having to utilize these systems in addition to the NHSN and its reporting period utilizes additional resources and will require multiple tracking strategies to keep up. They urged CMS to use data from these systems without requiring additional data collection in the NHSN.
Response: The TeleTracking system was one system that was used to manage the critical first months of the PHE for COVID-19, as it was critical that the Federal Government received data to facilitate planning, monitoring, and resource allocation during the COVID-19 Public Health Emergency (PHE). The TeleTracking system collects a number of data points, such as ventilators in the facility, ventilators in use, ICU beds available and ICU beds occupied. However, the TeleTracking system was not used for the SNF QRP. We proposed to use the NHSN COVID-19 Modules for tracking COVID-19 vaccination Coverage among HCP across all sites of service, including SNFs as most of the state Immunization Information Systems do not include the information needed to calculate the COVID-19 Vaccination Coverage among HCP. Additionally, the CDC has developed a Data Tracking Worksheet to assist SNFs collect information for the COVID-19 Vaccination Coverage among HCP measure. After entering the COVID-19 vaccination data for each HCP into the Tracking Worksheet and selecting a week, the data to be entered into the NHSN would automatically be calculated on the Reporting Summary.[105]
Comment: One commenter encouraged CMS to evaluate both methods of how data are submitted (that is, the TeleTracking system and the NHSN) and select just one standardized data reporting system and process. This commenter was in favor of using the NHSN to report the COVID-19 Vaccination Coverage among HCP measure because all care settings are using it to report the Influenza Vaccination Coverage measure among HCP and discontinuing COVID-19 vaccination reporting to the HHS tracking system.
Response: We proposed using the NHSN COVID-19 Modules for tracking COVID-19 Vaccination Coverage among HCP across all sites of service, including SNFs because most of the state Immunization Information Systems do not include the information needed to calculate the COVID-19 Vaccination Coverage among HCP measure.
Comment: A few commenters commented on CMS's statement that the COVID-19 Vaccination Coverage among HCP measure was modeled after the Influenza Vaccination Coverage among HCP measure. They believe there are key differences between the two measures, such as how the vaccines are administered and data are collected. Another provider listed the different reporting requirements for the numerator for the COVID-19 vaccination as compared to the influenza vaccination.
Response: We acknowledge that there are implementation differences between the two measures, even though the CDC modeled the COVID-19 Vaccination Coverage among HCP measure after the Influenza Vaccination Coverage among HCP measure. It is true that the influenza vaccine and the COVID-19 vaccine are not identical, and therefore the administration of these vaccines will not be identical. The key differences between the reporting requirements for the numerator of the COVID-19 Vaccination Coverage among HCP measure that the one commenter listed out are due to the fact that 2 of the 3 available COVID-19 vaccines require 2 doses to reach full vaccination status, and the 3rd available COVID-19 vaccine requires only 1 dose.
Comment: One commenter stated that the reporting burden for the COVID-19 Vaccination Coverage among HCP measure would be high since certain health care settings, including SNFs, do not currently use the NHSN to report data for the SNF QRP. Adopting the measure would require adjustments in workflow for which CMS would need to provide significant technical support.
Response: We disagree with the commenter, as SNFs are currently required to submit COVID-19 HCP vaccination data through the CDC's NHSN Long-term Care Facility COVID-19 Module of the NHSN. We refer readers to § 483.80(g). Therefore we believe there will be no additional burden imposed with the adoption of the SNF QRP measure.
Comment: One commenter attributed the burden of reporting to the fact that the commenter keeps employee health records separate from their electronic health records (EHRs) due to health privacy concerns. Other commenters attributed the burden of reporting to the fact that they cannot or have not routinely collected recorded information about medical contraindications or the reason for the employees' declination in their employee health records. They stated that because the indications and contraindications for receiving the vaccine have changed frequently, and ongoing findings and studies will continue to do so, collecting this information will be even more difficult to track. One commenter stated it will be challenging for providers to obtain the full count of adult students/trainees and volunteers associated with the healthcare system, as these individuals are not always captured or identified as such in their HR databases. Therefore attempting to identify, collect, and extract data on employee vaccinations are inherently difficult and burdensome.
Response: SNFs have experience tracking information and collecting data to inform their care approaches and business practices and have been collecting information related to COVID-19 infections and vaccinations. While SNFs will not have the burden of Start Printed Page 42494 registering and learning how to use the NHSN, we acknowledge there will be burden with collecting the required information. However, we believe it will be minimal because SNFs already have experience successfully reporting information using the NHSN reporting modules. We refer readers to section XI.A.5. of this final rule for an estimate of burden related to the COVID-19 Vaccination Coverage among HCP measure. The data sources for the number of HCP who have received COVID-19 vaccines may include HCP health records and paper and/or electronic documentation of vaccination given at the healthcare facility, pharmacy, or elsewhere. Further, HCP receiving vaccination elsewhere may provide documentation of vaccination. Additionally, the CDC has provided a number of resources including a tool called the Data Tracking Worksheet for COVID-19 Vaccination among Healthcare Personnel to help SNFs log and track this information.[106]
We also understand the commenter to state that the contraindications and precautions for the COVID-19 vaccine are changing as more studies are released. We would like to clarify that the contraindications have not changed. There are additional considerations around timing of the vaccine and which vaccine might be more appropriate for persons with underlying medications that are more clearly understood now. A summary of interim clinical considerations can be found at https://www.cdc.gov/vaccines/covid-19/downloads/summary-interim-clinical-considerations.pdf.
Comment: We received a comment in response to the proposed adoption of the COVID-19 Vaccination Coverage among HCP measure for the SNF QRP recommending CMS assess Immunization Information Systems (IIS).
Response: We understand Immunization information systems (IIS) to be confidential, population-based, computerized databases that record immunization doses administered by participating providers to persons residing within a given geopolitical area but these systems are not standardized across all SNFs. The Department of HHS has an Immunization Information Systems Support Branch (IISSB), that facilitates the development, implementation, and acceptance of these systems, but they are overseen by the states and/or organizations who develop them. CMS proposed using the NHSN COVID-19 Modules for collecting data on the COVID-19 Vaccination Coverage among HCP across all sites of service, including SNFs.
After careful consideration of the public comments we received, we are finalizing the method of data submission for COVID-19 Vaccination Coverage among Healthcare Personnel measure as proposed.
4. Schedule for Data Submission of the COVID-19 Vaccination Coverage Among Healthcare Personnel Measure Beginning With the FY 2023 SNF QRP
As discussed in section VII.C.2. of this final rule, we proposed to adopt the COVID-19 Vaccination Coverage among HCP quality measure beginning with the FY 2023 SNF QRP. Given the time-sensitive nature of this measure in light of the PHE, we proposed an initial data submission period from October 1, 2021 through December 31, 2021. Starting in CY 2022, SNFs would be required to submit data for the entire calendar year beginning with the FY 2024 SNF QRP.
SNFs would submit data for the measure through the CDC/NHSN web-based surveillance system. SNFs would use the COVID-19 vaccination data collection module in the NHSN Long-term Care (LTC) Component to report the cumulative number of HCP eligible to work in the healthcare facility for at least 1 day during the reporting period, excluding persons with contraindications to COVID-19 vaccination (denominator) and the cumulative number of HCP eligible to work in the SNF for at least 1 day during the reporting period and who received a complete vaccination course against COVID-19 (numerator). SNFs would submit COVID-19 vaccination data through the NHSN for at least 1 week each month and the CDC would report to CMS quarterly. We invited public comment on this proposal. The following is a summary of the public comments received on the proposed Schedule for Data Submission of the COVID-19 Vaccination Coverage among Healthcare Personnel Measure beginning with the FY 2023 SNF QRP and our responses:
Comment: One commenter requested that CMS clarify when SNFs should submit vaccination data so the data reported will be consistent among all SNFs.
Response: We proposed SNFs submit vaccination data 1 week out of every month, but with the option for SNFs to choose which week to report.
Comment: We received several comments requesting that CMS consider easing the reporting frequency for the COVID-19 Vaccination Coverage among HCP measure. They stated that reporting vaccinations 1 week per month, rather than one time per quarter is burdensome. A couple of providers support quarterly reporting since the Influenza Vaccination among HCP measure uses quarterly reporting.
Response: We want to clarify that the COVID-19 Vaccination Coverage among HCP measure is reported to the CDC through the NHSN at least 1 week per month. Each quarter the CDC averages the 3 weeks of data collected over the 3 months and sends a quarterly average vaccination rate for each provider to CMS. We proposed a reporting schedule of 1 week per month to provide vaccination coverage data on a more timely basis than the Influenza Vaccination Coverage among HCP (NQF #0431), while also reducing the burden on SNFs that weekly reporting of this information would have been.
Comment: A commenter stated that CMS did not explain the feedback reports and the timeline for feedback on the COVID-19 Vaccination Coverage among HCP measure as required by the IMPACT Act.
Response: Historically, we have provided the following types of confidential provider feedback reports that give providers opportunity to review and correct data: (1) Review and Correct, which allows providers to review and correct their data for any given CY quarter, as early as one day following the end of the given quarter, but prior to the data submission deadline for that quarter, which falls approximately 4.5 months after the end of the quarter; and (2) Provider Preview Report, the purpose of which is to allow providers to preview their quality measure scores that will be publicly posted for the upcoming refresh of Care Compare, and also allows providers to request a formal review of the data contained within, should the provider disagree with the reported measure results.
We also provide Quality Measure Reports (Facility and Patient-Level), the purpose of which is to allow providers to improve quality based on the most up-to-date data they have entered and/or modified within our systems. This report type is not related to public reporting, and is produced solely for the benefit of quality improvement. Quality Measure Reports are not related to public reporting and do not observe the quarterly data submission deadlines of assessment-based data, and will continue to capture and include any and all data entered and/or modified beyond any data submission deadline. We Start Printed Page 42495 provide Quality Measure Reports in order to give providers, including SNFs, the most accurate picture of quality within their facility, allowing for the improvement of quality. While we have historically added new measures to the Quality Measure reports prior to public reporting, the Quality Measure reports are not related to public reporting. Because we believe it is in the best interest of Medicare beneficiaries that we publicly report the results of the COVID-19 Vaccination HCP measures as soon as is feasible, in this instance, we are not able to add this measure to the Quality Measure reports prior to public reporting. Instead, we plan to add this new measure to the Quality Measure reports in fall 2022, at the earliest, which will in no way affect a SNF's ability to review and/or correct their data for this measure, nor will it affect a SNF's ability to preview the COVID-19 Vaccination HCP data prior to the public posting of this data.
The COVID-19 Vaccination HCP measure is stewarded by the CDC NHSN. To date, we have never added any of the CDC NHSN measures to the Review and Correct report, as the data for these measures are at the CDC. In lieu of this, the CDC makes accessible to PAC providers, including SNFs, reports that are similar to the Review and Correct reports that allow for real-time review of data submissions for all CDC NHSN measures adopted for use in the CMS PAC QRPs, including the SNF QRP. These reports are referred to as the "CMS Reports" within the Analysis Reports page in the NHSN Application. Such a report exists for each CDC/NHSN measure within each of the PAC programs, and each report is intended to mimic the data that will be sent to CMS on their behalf. This report will exist to serve the same "review and correct" purposes for the COVID-19 Vaccination Coverage among HCP measure. The CDC publishes reference guides for each facility type (including SNF) and each NHSN measure, which explain how to run and interpret the reports.
We will provide SNFs with a preview of SNF performance on the COVID-19 Vaccination Coverage among HCP measure, available on the SNF Provider Preview Report, which will be issued approximately 3 months prior to displaying the measure on Care Compare. As always, SNFs will have a full 30 days to preview their data. Should a SNF disagree with their measure results, they can request a formal review of their data by CMS. Instruction for submitting such a request are available on the SNF Quality Reporting Public Reporting website at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Skilled-Nursing-Facility-Quality-Reporting-Program/SNF-Quality-Reporting-Program-Public-Reporting.
After careful consideration of the public comments we received, we are finalizing the schedule for data submission of the COVID-19 Vaccination Coverage among Healthcare Personnel measure beginning with the FY 2023 SNF QRP as proposed.
5. Consolidated Appropriations Act and the SNF QRP
On December 27, 2020, Congress enacted the Consolidated Appropriations Act, 2021 (CAA) (Pub. L. 116-260). Section 111(a)(3) of Division CC of the CAA amends section 1888 of the Act by adding a new paragraph (h)(12), which requires the Secretary to apply a process to validate the measures submitted under the SNF VBP and the measures and data submitted under the SNF QRP as appropriate, which may be similar to the process specified under the Hospital Inpatient Quality Reporting (IQR) Program for validating inpatient hospital measures. We plan to develop a process for validating the SNF QRP measures and data and implement this policy as soon as technically feasible. We will provide more details and seek public comment in future rulemaking. For more information on the SNF VBP please refer to section VIII. of this rule.
H. Policies Regarding Public Display of Measure Data for the SNF QRP
1. Background
Section 1899B(g) of the Act requires the Secretary to establish procedures for making the SNF QRP data available to the public, including the performance of individual SNFs, after ensuring that SNFs have the opportunity to review their data prior to public display. SNF QRP measure data are currently displayed on the Nursing homes including rehab services website within Care Compare and the Provider Data Catalog. Both Care Compare and the Provider Data Catalog replaced Nursing Home Compare and Data.Medicare.gov, which were retired in December 2020. For a more detailed discussion about our policies regarding public display of SNF QRP measure data and procedures for the opportunity to review and correct data and information, we refer readers to the FY 2017 SNF PPS final rule (81 FR 52045 through 52048).
2. Public Reporting of the Skilled Nursing Facility Healthcare-Associated Infections Requiring Hospitalization Measure Beginning With the FY 2023 SNF QRP
We proposed public reporting for the SNF HAI measure beginning with the April 2022 Care Compare refresh or as soon as technically feasible using data collected from discharges in FY 2019 beginning October 1, 2018 through September 30, 2019. Provider preview reports would be distributed in January 2022. A SNF's HAI rates would be displayed based on 1 fiscal year of data. Since we cannot publicly report data from Q1 and Q2 of 2020 due to the PHE, we proposed to use data collected from discharges in FY 2021 (October 1, 2020 through September 30, 2021) for public reporting of the SNF HAI measure in the October 2022 Care Compare refresh. Thereafter, the SNF HAI measure would be calculated using four quarters of FY data for the annual refresh on Care Compare. Claims-based measures are only refreshed on Care Compare annually. To ensure statistical reliability of the data, we proposed assigning SNFs with fewer than 25 eligible stays during a performance period to a separate category: "The number of resident stays is too small to report." Eligible stays meet the measure's denominator inclusion criteria, and we refer readers to the Skilled Nursing Facility Healthcare-Associated Infections Requiring Hospitalization for the Skilled Nursing Facility Quality Reporting Program Technical Report available at https://www.cms.gov/files/document/snf-hai-technical-report.pdf/ for more details. If a SNF had fewer than 25 eligible stays, the SNF's performance would not be publicly reported for the measure for that performance period. We refer readers to CMS's SNF QRP Public Reporting web page for more information available at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Skilled-Nursing-Facility-Quality-Reporting-Program/SNF-Quality-Reporting-Program-Public-Reporting.
We invited public comment on this proposal for the public display of the SNF HAI measure on Care Compare. The following is a summary of the public comments received on our proposal for the public display of the SNF HAI measure on Care Compare and our responses:
Comment: Several commenters supported the proposed public reporting schedule.
Response: We appreciate our commenters for their support in the Start Printed Page 42496 public display schedule of the SNF HAI measure.
Comment: A couple of commenters recommended delaying SNF HAI measure adoption due to concerns that FY 2021 will include COVID-19 data and therefore not be comparable to FY 2019 non-COVID-19 data. Commenters suggested delaying public reporting until after the end of the PHE to avoid penalizing SNFs.
Response: As long as SNFs report their HAI rates, which will occur at no additional burden since the measure is claims-based, they will satisfy the reporting requirements for the measure. To clarify, we do not intend to use FY 2019 data as a benchmark for comparison against FY 2021 data. Instead, the measure identifies SNFs that have notably higher rates of HAIs that are acquired during SNF care and result in hospitalization, when compared to the performance of other SNFs in the United States in the same time period. COVID-19 has heightened the importance of infection prevention and control programs and the need to report HAI data. Evidence suggests that higher COVID-19 transmission in healthcare settings, including SNFs, is associated with poorer infection control, staff rotations between multiple SNFs, and inadequate patient COVID-19 screenings.[107 108] We will continue to evaluate the impact of the PHE and explore the impact of COVID-19 on quality reporting.
Comment: One commenter opposed CMS excluding SNFs with fewer than 25 admissions from public reporting of the SNF HAI measure.
Response: Infection control in small SNFs is as essential as in larger SNFs. We proposed the minimum reporting threshold to ensure sufficient reliability and to mitigate the risk of exposing personally identifiable information (PII) and protected health information (PHI). This proposal of minimum threshold for public reporting is in alignment with the existing SNF QRP claims-based measures, specifically the Discharge to Community (DTC) and Potentially Preventable 30-Day Post-Discharge Readmission (PPR) measures.
After careful consideration of the public comments we received, we are finalizing the proposal to publicly report the SNF HAI measure beginning with the April 2022 refresh as proposed.
3. Public Reporting of the COVID-19 Vaccination Coverage Among Healthcare Personnel (HCP) Measure Beginning With the FY 2023 SNF QRP
We proposed to publicly report the COVID-19 Vaccination Coverage among Healthcare Personnel measure beginning with the October 2022 Care Compare refresh or as soon as technically feasible using data collected for Q4 2021 (October 1, 2021 through December 31, 2021). If finalized as proposed, a SNF's HCP COVID-19 vaccination coverage rate would be displayed based on one quarter of data. Provider preview reports would be distributed in July 2022. Thereafter, HCP COVID-19 vaccination coverage rates would be displayed based on one quarter of data updated quarterly. Subsequent to this, one additional quarter of data would be added to the measure calculation during each advancing refresh, until the point four full quarters of data is reached. Thereafter, the measure would be reported using four rolling quarters of data.
We invited public comment on this proposal for the public display of the COVID-19 Vaccination Coverage among HCP measure on Care Compare. The following is a summary of the public comments received on our proposal for the public display of the COVID-19 Vaccination Coverage among HCP measure on Care Compare and our responses:
Comment: Several commenters supported the proposal to publicly report the COVID-19 Vaccination Coverage among HCP measure beginning with the October 2022 Care Compare refresh or as soon as technically feasible. The commenters stated that publishing facility-level data on HCP vaccination rates would also provide additional information about SNFs pandemic response and readiness efforts.
Response: We thank the commenters for their support and agree that publishing facility-level data on HCP vaccination rates would also provide additional information about SNFs' pandemic response and readiness efforts.
Comment: One commenter suggested reporting the percentage of HCP that had received their dose, broken out by first and second dose, as well as the percentage of all facility staff that have received their dose, broken out by first and second dose.
Response: We believe the value of the measure is in knowing the number of HCP who have completed their vaccination course as accumulating evidence indicates fully vaccinated people are able to participate in most activities with very low risk of acquiring or transmitting SARS-CoV-2.[109]
Comment: A commenter requested that CMS reconsider how the measure is calculated for public reporting. They supported the concept of reporting one quarter of data. They recommend that after the first refresh, rather than calculating a summary measure of the COVID-19 vaccination coverage from the 3 monthly modules of data reported for the quarter during each refresh and adding one additional quarter of data to the measure calculation during each advancing refresh, until the point that four full quarters of data is reached, to use an alternate approach. They recommend updating the information monthly with only the most recent data, such that the measure would be consumed as the most recent quarter of data refreshed quarterly. They caution that averaging over 12 months would result in the dilution of the most recent, and potentially more meaningful information, and may actually discourage higher provider vaccine uptake rates since it would be harder to change performance on this measure.
Response: We agree with the commenters' concern with regard to timely display of publicly reported data. We believe it is important to make the most up-to-date data available to beneficiaries, which will support them in making essential decisions about health care. We agree with these concerns, and find that it is appropriate to revise the public reporting policy for this measure to use quarterly reporting, as opposed to averaging over four rolling quarters, which allows the most recent quarter data to be displayed for the reasons outlined by the commenter. This revision would result in publishing information that is more up to date and would not affect the data collection schedule established for submitting data to NHSN for the COVID-19 vaccination Start Printed Page 42497 measure. This revision would simply update the way the measure's data are displayed for the public reporting purposes.
Comment: One commenter recommended that CMS either delay adoption of the measure for at least 1 year (that is, until October 1, 2022), or adopt the measure for voluntary reporting for at least the first year so it would not appear as though the Administration supported mandatory vaccinations.
Response: We believe that the unprecedented risks associated with the COVID-19 PHE warrant direct and prompt attention and, that it is important to begin publicly reporting this measure as proposed. However, as discussed in section VII.C.2.e. of this final rule, the COVID-19 Vaccination Coverage among HCP measure does not require SNF HCP to be vaccinated in order for SNFs to report the measure under the SNF QRP.
Comment: One commenter stated that several state legislatures were considering laws to prohibit an employer from forcing employees to be vaccinated for COVID-19, while other states are considering legislation to specifically authorize employer-mandated vaccinations. The commenter is concerned that provider performance on the measure could vary significantly based on differing state laws.
Response: We believe that the unprecedented risks associated with the PHE for COVID-19 warrant direct attention. Further, the COVID-19 Vaccination Coverage among HCP measure does not require providers to adopt mandatory vaccination policies. To support a comprehensive vaccine administration strategy, we encourage SNFs to engage in the provision of appropriate and accessible education and vaccine-offering activities. Many SNFs across the country are educating staff, patients, and patient representatives, participating in vaccine distribution programs, and reporting vaccine administration. The CDC has a number of resources[110] available to providers to assist in building vaccine confidence.
Consistent vaccination reporting by SNFs via the NHSN will help patients and their caregivers identify SNFs that have potential issues with vaccine confidence or slow uptake among staff. Implementation of COVID-19 vaccine education and vaccination programs in SNFs will help protect patients and staff, allowing for an expedited return to more normal routines, including timely preventive healthcare; family, caregiver, and community visitation; and group and individual activities.[111]
Comment: Several commenters questioned whether the COVID-19 Vaccination Coverage among HCP measure's information will be of value in 2023 and beyond given the time associated with data collection, submission, and validation. While they support the rights of consumers to access real-time meaningful data to help inform healthcare decision-making, they believe that the use of a single, dated measure is not a true reflection of the safety or quality of care delivered at the SNF.
Response: We disagree with the commenter and believe the measure should be publicly reported. As far as the timeliness of the reporting, the SNF QRP public display policies, as finalized in the FY 2017 SNF PPS final rule (81 FR 52041), allows 4.5 months after the end of the reporting quarter for SNFs to submit SNF QRP data. A number of administrative tasks must then occur in sequential order between the time SNF QRP data are submitted and are reported in Care Compare to ensure the validity of the data and to allow SNFs sufficient time to appeal any determinations of APU non-compliance. We have streamlined the process as much as possible, but must take these steps to ensure we are publishing accurate data. Additionally, the COVID-19 Vaccination Coverage among HCP measure will be one of several measures on Care Compare that patients and caregivers can use to make informed healthcare decisions. As with all other measures, we will routinely monitor this measure's performance, including assessing performance gaps across SNFs, and ensure the measure remains valid, reliable, and useful to consumers.
Comment: One commenter stated that since the COVID-19 vaccination rates for both staff and residents are now posted on the nursing home site at data.cms.gov (as a result of the new reporting requirements at § 483.80(g)) that adding the COVID-19 Vaccination Coverage among HCP measure to the SNF QRP for the stated purpose of transparency appears to be duplicative, unnecessary, and potentially more confusing. One commenter urged the CDC and CMS to use the data collected as a result of the change made to LTC Requirements of Participation at § 483.80(g) to publish on Care Compare since they believe it would provide a more accurate and comprehensive measure of HCP vaccination. Another commenter urged CMS to direct consumers to use the TeleTracking system to find vaccination rates.
Response: We disagree with these comments. The Care Compare provides a user-friendly interface that patients and caregivers can use to make informed decisions about healthcare based on cost, quality of care, volume of services, and other data, while also giving them the option to compare SNFs using this information. The data found on data.cms.gov and in the TeleTracking system do not have these features.
Comment: Another commenter questioned whether incorporating 2021 vaccination rates for HCP into quality ratings on Medicare Compare in 2023 would provide valuable information to SNF residents and their families.
Response: We are interpreting the commenter's question to be about the COVID-19 Vaccination Coverage among HCP measure and the timeline for reporting it on Care Compare. We proposed to report the inaugural COVID-19 Vaccination Coverage among HCP measure beginning with the October 2022 Care Compare refresh or as soon as technically feasible using data collected for Q4 2021 (October 1, 2021 through December 31, 2021). If finalized as proposed, provider preview reports would be distributed in July 2022.
Comment: A commenter did not support the proposal to use a shortened reporting timeframe of October 2021-December 2021 to meet the APU reporting requirements for FY 2023.
Response: We interpret the commenter to be referring to the SNF QRP reporting requirements to meet the compliance threshold for the FY 2023 Annual Payment Update. Our proposal to use of one quarter of data for the initial year of quality reporting for a new measure is consistent with the approach finalized in the FY 2016 SNF PPS final rule (80 FR 46389 to 46777) for all new measures in their first year of data reporting.
Comment: Commenters had differing opinions on whether the information obtained from the COVID-19 Vaccination Coverage among HCP measure would be helpful to consumers. Some stated that it does little to guide patients and their caregivers in the discharge planning process or to distinguish SNFs from one another. Another commenter acknowledged the value of this information for public Start Printed Page 42498 health and educational purposes, but still believes it would not be appropriate at this time to report publicly on MUC20-044 for the purposes of assessing SNF quality performance.
Response: We interpret the commenter to be referring to the CMS 2020 Measures Under Consideration (MUC) list and specifically the SARS-CoV-2 Vaccination Coverage among HCP measure (MUC20-044), whose name was subsequently changed to the COVID-19 Vaccination Coverage among HCP measure. This measure is important at this time because, as illustrated in Medicare claims and encounter data, the number of Medicare beneficiaries diagnosed with COVID-19 exceeded 4.3 million as of April 24, 2021.[112] We believe that the toll the COVID-19 pandemic has taken on Medicare beneficiaries, including SNF residents, demonstrates the need for increased action to mitigate the effects of the ongoing pandemic. Additionally, public reporting of this measure will inform patients and families of more recent information on quality of care provided in SNFs so patients and caregivers are able to make informed choices about critical dimensions of quality.
After careful consideration of the public comments we received, we are finalizing our proposal to publicly report the COVID-19 Vaccination Coverage among Healthcare Personnel (HCP) measure beginning with the October 2022 Care Compare refresh or as soon as technically feasible using data collected for Q4 2021 (October 1, 2021 through December 31, 2021). However, based on public comment, we will not finalize our plan to add one additional quarter of data during each advancing refresh, until the point that four full quarters of data is reached and then report the measure using four rolling quarters of data. We will instead only report the most recent quarter of data. This revision would result in publishing more meaningful information that is up to date.
4. Public Reporting of Quality Measures in the SNF QRP With Fewer Quarters Due to COVID-19 Public Health Emergency (PHE) Exemptions
a. COVID-19 Public Health Emergency Temporary Exemptions
Under the authority of section 319 of the Public Health Service Act, the Secretary of Health and Human Services declared a public health emergency (PHE) effective as of January 27, 2020. On March 13, 2020, subsequent to a presidential declaration of national emergency under the Stafford Act, the Secretary invoked section 1135(b) of the Act (42 U.S.C. 1320b-5) to waive or modify the requirements of titles XVIII, XIX, and XXI of the Act and regulations related to the PHE for COVID-19, effective as of March 1, 2020.[113] On March 27, 2020, we sent a guidance memorandum under the subject title, "Exceptions and Extensions for Quality Reporting Requirements for Acute Care Hospitals, PPS-Exempt Cancer Hospitals, Inpatient Psychiatric Facilities, Skilled Nursing Facilities, Home Health Agencies, Hospices, Inpatient Rehabilitation Facilities, Long-Term Care Hospitals, Ambulatory Surgical Centers, Renal Dialysis Facilities, and MIPS Eligible Clinicians Affected by COVID-19" to the Medicare Learning Network (MLN) Connects Newsletter and Other Program-Specific Listserv Recipients,[114] hereafter referred to as the March 27, 2020 CMS Guidance Memo. In that memo we granted an exception to the SNF QRP reporting requirements from Q4 2019 (October 1, 2019 through December 31, 2019), Q1 2020 (January 1, 2020 through March 31, 2020), and Q2 2020 (April 1, 2020 through June 30, 2020). We also stated that we would not publicly report any SNF QRP data that might be greatly impacted by the exceptions from Q1 and Q2 of 2020. This exception impacted the schedule for public reporting that would have included those two quarters of data.
SNF quality measures are publicly reported on Care Compare. Care Compare uses four quarters of data for MDS assessment-based measures and eight quarters for claims-based measures. Table 26 displays the original schedule for public reporting of SNF QRP measures.[115]
Start Printed Page 42499
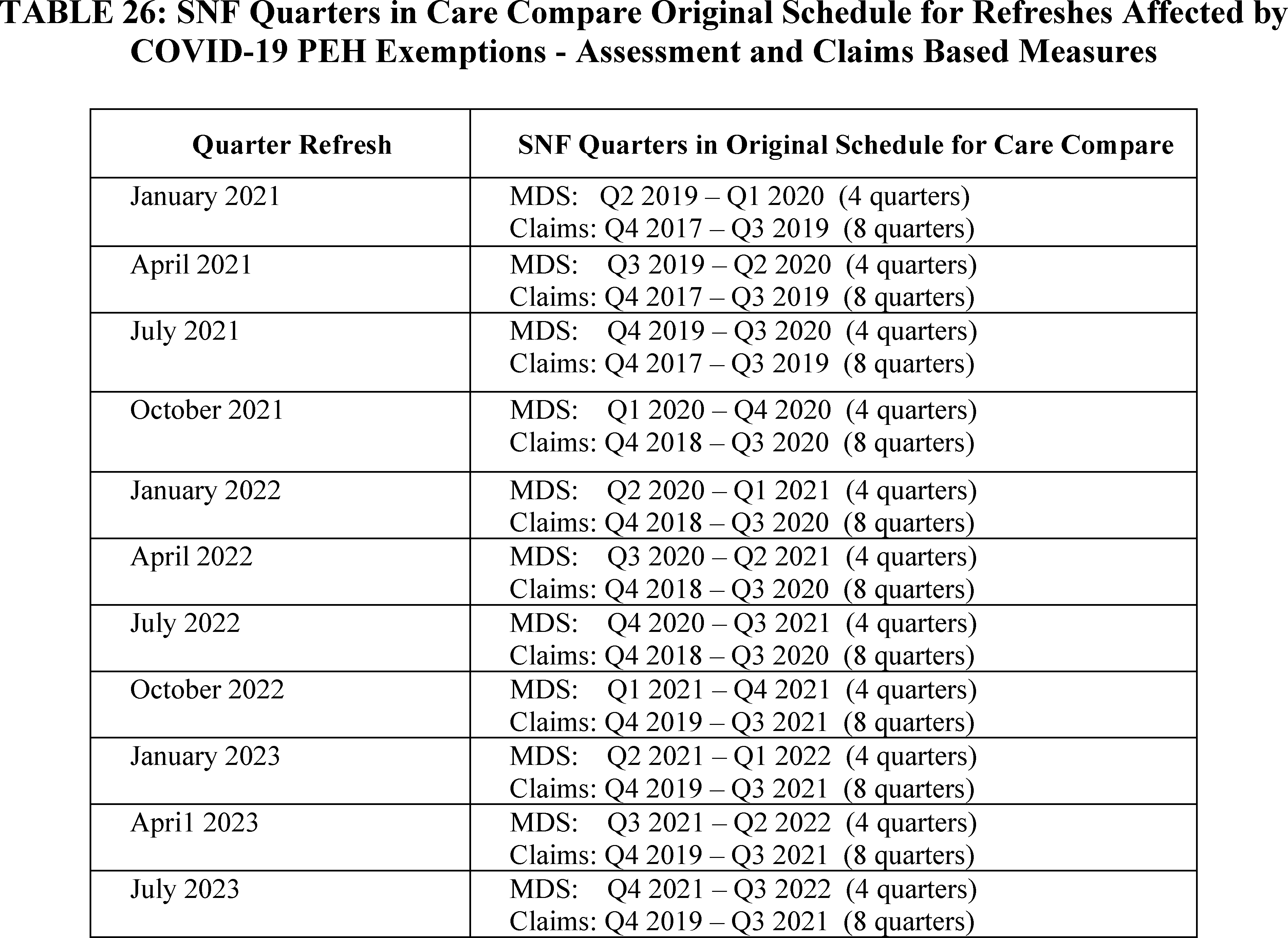
During 2020, we conducted testing to inform decisions about publicly reporting data for those refreshes which include partially and/or fully exempt data (discussed below). The testing helped us develop a plan for posting data that are as up-to-date as possible and that also meet acceptable standards for public reporting. We believe that the plan allows us to provide consumers with helpful information on the quality of SNF care, while also making the necessary adjustments to accommodate the exemption provided SNFs. The following sections provide the results of our testing, and explain how we used the results to develop plans for accommodating exempt and partially-exempt data in public reporting.
b. Exempted Quarters
In the March 27, 2020 Medicare Learning Network (MLN) Newsletter on Exceptions and Extensions for Quality Reporting Program (QRP) Requirements, we stated that we would not report any PAC quality data that might be greatly impacted by the exemptions granted for Quarter 1 and Quarter 2 of 2020. Given the timing of the PHE onset, we determined that we would not use SNF MDS assessments or SNF claims from Quarter 1 and Quarter 2 of 2020 for public reporting, but that we would assess the COVID-19 PHE impact on data from Quarter 4 2019. Before proceeding with the October 2020 refresh, we conducted testing to ensure that, despite the voluntary nature of reporting for that quarter, public reporting would still meet our public reporting standards. We found the level of reporting, measured in the number of eligible stays and providers, and the reported outcomes, to be in line with levels and trends observed in FY 2018 and FY 2019. We note that Quarter 4 2019 ended before the onset of the COVID-19 pandemic in the United States. Thus, we proceeded with including these data in SNF QRP measure calculations for the October 2020 refresh.
c. Update on Data Freeze and Proposal for January 2022 Public Reporting Methodology for SNF Claims-Based and MDS Assessment-Based Measures
In addition to the January 2021 refresh, there are several other forthcoming refreshes for which the original public reporting schedules included exempted quarters of SNF QRP data. The impacted refreshes for MDS assessment and claims based measures are outlined in (Table 26). We determined that freezing the data displayed on the website with the October 2020 refresh values—that is, hold data constant after the October 2020 refresh data on the website without subsequent update—would be the most straightforward, efficient, and equitable approach for SNFs. Thus, we decided that, for as many refreshes as necessary, we would hold data constant on the website with the October 2020 data, and communicate this decision to the public.
Because October 2020 refresh data will become increasingly out-of-date and thus less useful for consumers, we analyzed whether it would be possible to use fewer quarters of data for one or more refreshes and thus reduce the number of refreshes that continue to display October 2020 data. Using fewer quarters of more up-to-date data requires that (1) a sufficient percentage of SNFs would still likely have enough assessment data to report quality measures (reportability); and (2) fewer quarters would likely produce similar measure scores for providers, with similar reliability, and thus not unfairly represent the quality of care SNFs provide during the period reported in a given refresh (reliability). Start Printed Page 42500
To assess these criteria, we conducted reportability and reliability analysis using 3 quarters of data in a refresh, instead of the standard 4 quarters of data for reporting assessment-based measures and using 6 quarters instead of 8 for claims-based measures. Specifically, we used historical data to calculate MDS assessment based and SNF claims based quality measures under two scenarios:
1. Standard Public Reporting (SPR) Base Scenario: We used four quarters of CY 2019 data as a proxy alternative for the exempted quarters in CY 2020 in order to compare results. For assessment-based measures, the quarters used in this scenario are Q1 through Q4 2019. For claims-based measures, the quarters used in this scenario are Q1 2018 through Q4 2019.
2. COVID-19 Affected Reporting (CAR) Scenario: We calculated SNF QRP measures using 3 quarters (Q2 2019 through Q4 2019) of SNF QRP data for assessment-based measures, and 6 quarters (Q1 2018 through Q4 2018 and Q3 2019 through Q4 2019) for claims-based measures. The CAR scenario uses the most recently available data to simulate the public health emergency reality where quarters 1 and 2 of a calendar year must be excluded from calculation. Quarterly trends in MDS assessment-based and claims based measures indicate that these measures do not exhibit substantial seasonal variation.
To assess performance in these scenarios, we calculated the reportability as the percent of SNFs meeting the case minimum for public reporting (the public reporting threshold). To test the reliability of restricting the SNFs included in the SPR Base Scenario to those included in the CAR Scenario, we performed three tests on the set of SNFs included in both scenarios. First, we evaluated measure correlation using the Pearson and Spearman correlation coefficients, which assess the alignment of SNFs' provider scores. Second, for each scenario, we conducted a split-half reliability analysis and estimated intraclass correlation (ICC) scores, where higher scores imply better internal reliability. Modest differences in ICC scores between both scenarios would suggest that using fewer quarters of data does not impact the internal reliability of the results. Third, we estimated reliability scores where a higher value indicates that measure scores are relatively consistent for patients admitted to the same SNF and variation in the measure reflects true differences across providers. To calculate the reliability results, we restricted the SNFs included in the SPR scenario to those included in the CAR scenario.
Our testing indicated that the expected impact of using fewer quarters of data on reportability and reliability of MDS assessment-based and claims based measures is acceptable.
We proposed to use the CAR scenario as the approach for the following affected refreshes for MDS assessment-based measures, the affected refresh is the January 2022 refresh; for claims-based measures, the affected refreshes occur from January 2022 through July 2023. For the earlier four affected refreshes (January, April, July, and October 2021), we decided to hold constant the Care Compare website with October 2020 data. We communicated this decision in a Public Reporting Tip Sheet, which is located at https://www.cms.gov/files/document/snfqrp-covid19prtipsheet-october2020.pdf.
Our proposal of the CAR approach for the affected refreshes would allow us to begin displaying more recent data in January 2022, rather than continue displaying October 2020 data (Q1 2019 through Q4 2019 for assessment-based measures, Q4 2017 through Q3 2019 for claims-based measures). We believe that resuming public reporting starting in January 2022 with fewer quarters of data can assist consumers by providing more recent quality data as well as more actionable data for SNF providers. Our testing results indicate we can achieve these positive impacts with acceptable changes in reportability and reliability. Table 27 summarizes the revised schedule (that is, frozen data) and the proposed schedule (that is, using fewer quarters in the affected refreshes) for assessment-based measures. Tables 28 and 29 summarize the revised schedule (that is, frozen data) and the proposed schedule (that is, using fewer quarters in the affected refreshes) for claims-based measures.
We invited public comment on the proposal to use the CAR scenario to publicly report SNF measures for the January 2022 through July 2023 refreshes.

Start Printed Page 42501


The following is a summary of the public comments received on the proposal to use the CAR scenario to publicly report SNF measures for the January 22 through July 2023 refreshes and our responses:
Comment: We received two comments on the proposed COVID-19 Affected Reporting (CAR) scenario methodology. One commenter supported the proposal to report fewer quarters of data. Another commenter stated that the CAR scenario appeared to adequately ensure data reportability and reliability and requested that CMS continue to monitor modified Care Compare refreshes until normal reporting resumes to ensure the CAR approach produces valid and reliable results.
Response: We thank the commenters for their support and will continue to monitor measures to identify any concerning trends as part of our routine monitoring activities to regularly assess measure performance, reliability, and reportability for all data submitted for the SNF QRP.
Comment: Most commenters expressed their appreciation for the flexibility that CMS offered to SNF providers during the early months of the COVID-19 pandemic in granting an exception to the SNF QRP reporting requirements from Q1 2020 (January 1, 2020 through March 31, 2020) and Q2 2020 (April 1, 2020 through June 30, 2020). However, a number of commenters raised concerns with CMS' proposal to utilize fewer than the standard number of quarters for public reporting of quality measures on Care Compare, since it includes SNF QRP reporting from Q3 2020 (July 1, 2020 through September 30, 2020) and Q4 2020 (October 1, 2020 through December 31, 2020). Commenters pointed out that the COVID-19 pandemic community infection rate surged repeatedly across different regions of the country, at different times, and did not begin to become under control until Q1 2021 after the first wave of COVID-19 vaccine was disseminated to SNF residents and staff. Instead, they urged CMS to exclude the entire calendar year 2020 data.
Response: While we understand that there are concerns related to the use of Q3 and Q4 2020 data, we believe that the value of the information provided to users through public reporting outweighs these concerns. Additionally, we provided a 6-month exception to Start Printed Page 42502 SNF QRP reporting requirements related to the PHE, and we believe that timeframe was sufficient for providers to adjust to the change in care patterns associated with the pandemic. We further believe that the public display of quality data is extremely important so patients and caregivers can continue to make informed healthcare choices. The continued need for access to provider quality data on Care Compare by CMS beneficiaries outweighs any potential provider impacts.
As described above, we conducted testing to inform our decisions about publicly reporting data for refreshes using Q3 and Q4 2020. As discussed in section VI.H.4.c. of the FY 2021 SNF PPS proposed rule (86 FR 20004 through 20005), the testing helped us develop a plan that we believe meets acceptable standards for public reporting. SNFs that believe they were disproportionately affected by the PHE may apply for an individual exception or extension related to the SNF QRP reporting requirements for Q3 and/or Q4 2020. Instructions for requesting an extraordinary circumstances exemption (ECE) may be found on the SNF QRP Reconsideration and Exception and Extension web page at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Skilled-Nursing-Facility-Quality-Reporting-Program/SNF-QR-Reconsideration-and-Exception-and-Extension.
Comment: One commenter believes public reporting should be frozen until the first quarter after the end of the PHE. Since the proposed public reporting schedule would utilize data submitted while the country was still under a PHE, particularly during the proposed Q3 2020 through Q1 2021 timeframes, they believe it may not reflect normal SNF performance and results both at the facility, and geographically.
Response: We disagree with the commenter about freezing the data until after the first quarter of the end of the PHE. COVID-19 has caused us to take a number of actions to further protect SNF residents. Resuming public reporting will inform patients and families of more recent information on quality of care provided in SNFs. As we progress, we will analyze SNF QRP measures for any significant changes, and take any actions needed to continue the improvement and protection of patient health and safety.
Comment: Several commenters believe that payments to their SNFs would be negatively impacted since their state Medicaid systems use quality measure data and the star ratings published on Care Compare to determine quality incentive payment rates to nursing facilities. They urged CMS not to penalize providers under the Five-Star rating system for measure performance ratings derived during Q3 2020 through Q1 2021.
Response: We acknowledge that other programs may utilize the SNF QRP for their own purposes. We proposed the COVID-19 Vaccination Coverage among HCP measure for the SNF QRP. Comments about state Medicaid programs and the Five-Star rating system are outside the scope of this final rule.
Comment: One commenter stated that due to specific CDC and CMS mandated COVID-19 infection control requirements, specific MDS items used for some measures (that is, mobility and self-care) may have been directly and artificially impacted, which could further skew the results during this period. The inability to account for or risk-adjust the measures for the influence of a worldwide airborne viral pandemic was also given as justification for excluding additional quarters in 2020.
Response: We are uncertain what the commenter means in stating that some measures may have been artificially impacted. We acknowledge the efforts that SNFs have gone to keep their residents and staffs as safe as possible during the COVID-19 PHE. One of the reasons the SNF QRP reporting requirement waivers for reporting measure data was granted for Q4 2019 through Q2 2020 was to enable SNFs to address their residents' care, and to acclimate to care patterns associated with the PHE. However, CMS uses all SNF QRP data submitted to CMS for the purposes of public reporting. As stated previously, we routinely monitor measures to identify any concerning trends, and will continue to do so as part of our routine monitoring activities to regularly assess measure performance, reliability, and reportability for all data submitted for the SNF QRP.
Comment: One commenter requested that CMS include a notation on Care Compare to explain the temporary adjustments made for the PHE and that consumers should consider additional information when selecting facilities such as survey results and in-person facility visits.
Response: We will notify consumers of the use of fewer quarters of data reported on Care Compare when the website is refreshed. However, we do not believe that posting additional messaging alluding to how SNF measure scores may or may not be affected by the ongoing PHE would be helpful to consumers. Such messages would give the impression that the data posted on Care Compare are inaccurate or cannot be used when making informed healthcare decisions, which is not the case given the extensive testing CMS conducts.
After careful consideration of the public comments, we are finalizing the revisions to use the CAR scenario to publicly report SNF measures for the January 2022 through July 2023 refreshes as proposed.
I. Miscellaneous Comments
Comment: One commenter encouraged CMS to provide more infrastructure support for SNFs to adopt certified electronic technology to facilitate meaningful data exchange. They point out the importance of knowing whether the data have been received and acted upon, as well as the opportunity to understand just what parts of the data are most beneficial to the receiving provider.
Response: This comment is out of scope and is not relevant to our proposal to update the TOH Information measure.
VIII. Skilled Nursing Facility Value-Based Purchasing (SNF VBP) Program
A. Statutory Background
Section 215(b) of the Protecting Access to Medicare Act of 2014 (PAMA) (Pub. L. 113-93) authorized the SNF VBP Program (the "Program") by adding section 1888(h) to the Act. As a prerequisite to implementing the SNF VBP Program, in the FY 2016 SNF PPS final rule (80 FR 46409 through 46426), we adopted an all-cause, all-condition hospital readmission measure, as required by section 1888(g)(1) of the Act, and discussed other policies to implement the Program such as performance standards, the performance period and baseline period, and scoring. SNF VBP Program policies have been codified in our regulations at 42 CFR 413.338. For additional background information on the SNF VBP Program, including an overview of the SNF VBP Report to Congress and a summary of the Program's statutory requirements, we refer readers to the following prior final rules:
- In the FY 2017 SNF PPS final rule (81 FR 51986 through 52009), we adopted an all-condition, risk-adjusted potentially preventable hospital readmission measure for SNFs, as required by section 1888(g)(2) of the Act, adopted policies on performance standards, performance scoring, and sought comment on an exchange Start Printed Page 42503 function methodology to translate SNF performance scores into value-based incentive payments, among other topics.
- In the FY 2018 SNF PPS final rule (82 FR 36608 through 36623), we adopted additional policies for the Program, including an exchange function methodology for disbursing value-based incentive payments.
- In the FY 2019 SNF PPS final rule (83 FR 39272 through 39282), we adopted more policies for the Program, including a scoring adjustment for low-volume facilities.
- In the FY 2020 SNF PPS final rule (84 FR 38820 through 38825), we adopted additional policies for the Program, including a change to our public reporting policy and an update to the deadline for the Phase One Review and Correction process. We also adopted a data suppression policy for low-volume SNFs.
- In the FY 2021 SNF PPS final rule (85 FR 47624 through 47627), we amended regulatory text definitions at § 413.338(a)(9) and (11) to reflect the definition of Performance Standards and the updated Skilled Nursing Facility Potentially Preventable Readmissions after Hospital Discharge measure name, respectively. We also updated the Phase One Review and Correction deadline and codified that update at § 413.338(e)(1). Additionally, we codified the data suppression policy for low-volume SNFs at § 413.338(e)(3)(i), (ii), and (iii) and amended § 413.338(e)(3) to reflect that SNF performance information will be publicly reported on the Nursing Home Compare website and/or successor website (84 FR 38823 through 38824) which since December 2020 is the Provider Data Catalogue website (https://data.cms.gov/provider-data/).
The SNF VBP Program applies to freestanding SNFs, SNFs affiliated with acute care facilities, and all non-CAH swing-bed rural hospitals. Section 1888(h)(1)(B) of the Act requires that the SNF VBP Program apply to payments for services furnished on or after October 1, 2018. We believe the implementation of the SNF VBP Program is an important step towards transforming how payment is made for care, moving increasingly towards rewarding better value, outcomes, and innovations instead of merely rewarding volume.
B. SNF VBP Program Measures
For background on the measures we have adopted for the SNF VBP Program, we refer readers to the FY 2016 SNF PPS final rule (80 FR 46419), where we finalized the Skilled Nursing Facility 30-Day All-Cause Readmission Measure (SNFRM) (NQF #2510) that we are currently using for the SNF VBP Program. We also refer readers to the FY 2017 SNF PPS final rule (81 FR 51987 through 51995), where we finalized the Skilled Nursing Facility 30-Day Potentially Preventable Readmission Measure (SNFPPR) that we will use for the SNF VBP Program instead of the SNFRM as soon as practicable, as required by statute. The SNFPPR measure's name is now "Skilled Nursing Facility Potentially Preventable Readmissions after Hospital Discharge measure" (§ 413.338(a)(11)). We intend to submit the SNFPPR measure for NQF endorsement review during the Fall 2021 cycle, and to assess transition timing of the SNFPPR measure to the SNF VBP Program after NQF endorsement review is complete.
1. Flexibilities for the SNF VBP Program in Response to the Public Health Emergency Due to COVID-19
In previous rules, we have identified the need for flexibility in our quality programs to account for the impact of changing conditions that are beyond participating facilities' or practitioners' control. We identified this need because we would like to ensure that participants in our programs are not affected negatively when their quality performance suffers not due to the care provided, but due to external factors.
A significant example of the type of external factor that may affect quality measurement is the COVID-19 public health emergency (PHE), which has had, and continues to have, significant and ongoing effects on the provision of medical care in the country and around the world. The COVID-19 pandemic and associated PHE has impeded effective quality measurement in many ways. Changes to clinical practices to incorporate safety protocols for medical personnel and patients, as well as unpredicted changes in the number of stays and facility-level case mixes, have affected the data that SNFs report under the SNF VBP Program and the resulting measure calculations. CMS is considering whether the SNF readmission measure specifications should be updated to account for changes in SNF admission and/or hospital readmission patterns that we have observed during the PHE. Additionally, because COVID-19 prevalence is not identical across the country, facilities located in different areas have been affected differently at different times throughout the pandemic. Under those circumstances, we remain concerned that the SNF readmission measure scores are distorted, which would result in skewed payment incentives and inequitable payments, particularly for SNFs that have treated more COVID-19 patients than others.
It is not our intention to penalize SNFs based on measure scores that we believe are distorted by the COVID-19 pandemic, and are thus not reflective of the quality of care that the measure in the SNF VBP Program was designed to assess. As discussed above, the COVID-19 pandemic has had, and continues to have, significant and enduring effects on health care systems around the world, and affects care decisions, including readmissions to the hospital as measured by the SNF VBP Program. As a result of the PHE, SNFs could provide care to their patients that meets the underlying clinical standard but results in worse measured performance, and by extension, lower incentive payments in the SNF VBP Program. Additionally, because COVID-19 prevalence has not been identical across the country, SNFs located in different regions have been affected differently during the PHE. As a result, we are concerned that regional differences in COVID-19 prevalence during the revised performance period for the FY 2022 SNF VBP Program, which includes one quarter of data during the pandemic (July 1, 2020 through September 30, 2020), have directly affected SNF readmission measure scores for the FY 2022 SNF VBP Program Year. Although these regional differences in COVID-19 prevalence rates do not reflect differences in the quality of care furnished by SNFs, they directly affect the value-based incentive payments that these SNFs are eligible to receive and could result in an unfair and inequitable distribution of those incentives. These inequities could be especially pronounced for SNFs that have treated a large number of COVID-19 patients.
Therefore, we proposed to adopt a policy for the duration of the PHE for COVID-19 that would enable us to suppress the use of SNF readmission measure data for purposes of scoring and payment adjustments in the SNF VBP Program if we determine that circumstances caused by the PHE for COVID-19 have affected the measure and the resulting performance scores significantly. We proposed that under this policy, if we determine that the suppression of the SNF readmission measure is warranted for a SNF VBP Program Year, we would calculate the SNF readmission measure rates for that program year but then suppress the use of those rates to generate performance scores, rank SNFs, and generate value-based incentive payment percentages based on those performance scores. We Start Printed Page 42504 would instead assign each eligible SNF a performance score of zero for the program year to mitigate the effect that the distorted measure results would otherwise have on the SNF's performance score and incentive payment multiplier. We would also reduce each eligible SNF's adjusted Federal per diem rate by the applicable percent (2 percent) and then further adjust the resulting amounts by a value-based incentive payment amount equal to 60 percent of the total reduction. Those SNFs subject to the Low-Volume Adjustment policy would receive 100 percent of their 2 percent withhold in accordance with the policy previously finalized in the FY 2019 SNF PPS final rule (83 FR 39278 through 39280). We would also provide each SNF with its SNF readmission measure rate in confidential feedback reports so that the SNF is aware of the observed changes to its measure rates. We would also publicly report the FY 2022 SNF readmission measure rates with appropriate caveats noting the limitations of the data due to the PHE for COVID-19.
In developing this proposed policy, we considered what circumstances caused by the PHE for COVID-19 would affect a quality measure significantly enough to warrant its suppression in a value-based purchasing program. We believe that a significant deviation in measured performance that can be reasonably attributed to the PHE for COVID-19 is a significant indicator of changes in clinical conditions that affect quality measurement. Similarly, we believe that a measure may be focused on a clinical topic or subject that is proximal to the disease, pathogen, or other health impacts of the PHE. As has been the case during the COVID-19 PHE, we believe that rapid or unprecedented changes in clinical guidelines and care delivery, potentially including appropriate treatments, drugs, or other protocols, may affect quality measurement significantly and should not be attributed to the participating facility positively or negatively. We also note that scientific understanding of a particular disease or pathogen may evolve quickly during an emergency, especially in cases of new disease or conditions. Finally, we believe that, as evidenced during the COVID-19 PHE, national or regional shortages or changes in health care personnel, medical supplies, equipment, diagnostic tools, and patient case volumes or facility-level case mix may result in significant distortions to quality measurement.
Based on these considerations, we developed a number of Measure Suppression Factors that we believe should guide our determination of whether to propose to suppress the SNF readmission measure for one or more program years that overlap with the PHE for COVID-19. We proposed to adopt these Measure Suppression Factors for use in the SNF VBP Program and, for consistency, the following other value-based purchasing programs: Hospital Value-Based Purchasing Program, Hospital Readmissions Reduction Program, HAC Reduction Program, and End-Stage Renal Disease Quality Incentive Program. We believe that these Measure Suppression Factors will help us evaluate the SNF readmission measure in the SNF VBP Program and that their adoption in the other value-based purchasing programs noted above will help ensure consistency in our measure evaluations across programs. The proposed Measure Suppression Factors are:
(1) Significant deviation in national performance on the measure during the PHE for COVID-19, which could be significantly better or significantly worse compared to historical performance during the immediately preceding program years.
(2) Clinical proximity of the measure's focus to the relevant disease, pathogen, or health impacts of the PHE for COVID-19.
(3) Rapid or unprecedented changes in:
- Clinical guidelines, care delivery or practice, treatments, drugs, or related protocols, or equipment or diagnostic tools or materials; or
- The generally accepted scientific understanding of the nature or biological pathway of the disease or pathogen, particularly for a novel disease or pathogen of unknown origin.
(4) Significant national shortages or rapid or unprecedented changes in:
- Healthcare personnel;
- Medical supplies, equipment, or diagnostic tools or materials; or
- Patient case volumes or facility-level case mix.
We stated in the proposed rule that we had also considered alternatives to this proposed policy that could also fulfill our objective to not hold facilities accountable for measure results that are distorted due to the PHE for COVID-19. As noted above, the country continues to grapple with the effects of the COVID-19 PHE, and in March 2020, we issued a nationwide, blanket ECE for all hospitals and other facilities participating in our quality reporting and value-based purchasing programs in response to the PHE for COVID-19. This blanket ECE excepted all data reporting requirements for Q1 and Q2 2020 data. For claims-based measures, we also stated that we would exclude all qualifying Q1 and Q2 2020 claims from our measure calculations. We considered extending the blanket ECE that we issued for Q1 and Q2 2020 to also include Q3 2020 data. However, this option would result in less than 12 months of data being used to calculate the single readmissions measure in the Program for multiple program years, which we do not believe would provide an accurate assessment of the quality of care provided in SNFs. This option would also leave no comprehensive data available for us to provide confidential performance feedback to providers nor for monitoring and to inform decision-making for potential future programmatic changes, particularly as the PHE is extended.
As we stated in the proposed rule, we view this measure suppression proposal as a necessity to ensure that the SNF VBP Program does not reward or penalize facilities based on factors that the SNF readmission measure was not designed to accommodate. We also stated that we intend for this proposed policy to provide short-term relief to SNFs when we have determined that one or more of the Measure Suppression Factors warrants the suppression of the SNF readmission measure.
We invited public comments on this proposal for the adoption of a measure suppression policy for the SNF VBP Program for the duration of the PHE for COVID-19, and also on the proposed Measure Suppression Factors that we developed for purposes of this proposed policy.
We also invited comment on whether we should consider adopting a measure suppression policy that would apply in a future national PHE, and if so, whether under such a policy, we should have the flexibility to suppress quality measures without specifically proposing to do so in rulemaking. We also requested comment on whether we should in future years consider adopting any form of regional adjustment for the proposed measure suppression policy that could take into account any disparate effects of circumstances affecting hospitals around the country that would prompt us to suppress a measure. For example, COVID-19 affected different regions of the country at different rates depending on factors like time of year, geographic density, state and local policies, and health care system capacity. In future years and for future PHEs, should they arise, we also requested commenters' feedback on whether we should, rather than suppress a measure completely, consider a suppression policy with Start Printed Page 42505 more granular effects based on our assessment of the geographic effects of the circumstances, and if so, how region-based measure suppression could be accounted for within the program's scoring methodology.
The following is a summary of the public comments received on the proposed Flexibilities for the SNF VBP Program in Response to the Public Health Emergency Due to COVID-19 and our responses:
Comment: Several commenters expressed support for our proposal to establish a measure suppression policy for the PHE due to COVID-19 and for future PHEs. Many of the commenters noted that the proposed measure suppression factors are appropriate and comprehensive. One commenter suggested we include a review of state and regional performance in addition to national performance when evaluating the measure suppression factors in order to account for regional and state differences in the response to the PHE due to COVID-19. A few commenters recommended that the measure suppression should occur anytime a PHE is declared and extend through the end of that PHE, and one commenter specifically urged us to continue measure suppression for the PHE due to COVID-19 in FY 2023 to account for late surges that occurred in late CY 2020 and early CY 2021. A few commenters also expressed appreciation for our intent to standardize our suppression policy across settings and payment programs.
Response: We agree that the Measure Suppression Factors are appropriate. In our development of this measure suppression proposal, we considered that COVID-19 prevalence has not been identical across the country and that SNFs located in different regions have been affected differently during the PHE. Our proposal in the FY 2022 SNF PPS proposed rule was to adopt a measure suppression policy only for the duration of the COVID-19 PHE and to suppress the SNF readmission measure for only the FY 2022 SNF VBP Program, but we are continuing to consider options for mitigating any potential negative impacts the PHE due to COVID-19 may have on the FY 2023 Program.
Comment: A few commenters noted that CMS should be required to go through the rulemaking process when suppressing measures to ensure that the approach is fully vetted.
Response: We thank commenters and agree that we should use the rulemaking process if we consider suppressing one or more measures.
After considering the public comments, we are finalizing our measure suppression policy as proposed.
2. Suppression of the SNFRM for the FY 2022 SNF VBP Program Year
In the proposed rule, we proposed to suppress the SNFRM for the FY 2022 SNF VBP Program Year under proposed Measure Suppression Factor: (4) Significant national shortages or rapid or unprecedented changes in: (iii) Patient case volumes or facility-level case mix.
In response to the PHE for COVID-19, we granted an ECE for SNFs participating in the SNF VBP Program. Under the ECE, SNF qualifying claims for the period January 1, 2020 through June 30, 2020 are excepted from the calculation of the SNFRM. Because this ECE excepted data for 6 months of the performance period that we had previously finalized for the FY 2022 SNF VBP program year (84 FR 38822), we updated the performance period for that program year in the "Medicare and Medicaid Programs, Clinical Laboratory Improvement Amendments, and Patient Protection and Affordable Care Act: Additional Policy and Regulatory Revisions in Response to the COVID-19 Public Health Emergency" interim final rule with comment ("the September 2nd IFC") (85 FR 54820). Specifically, we finalized that the new performance period for the FY 2022 SNF VBP program year would be April 1, 2019 through December 31, 2019 and July 1, 2020 through September 30, 2020 because we believed that this period, which combined 9 months of data prior to the start of the PHE for COVID-19 and 3 months of data after the end of the ECE, would provide sufficiently reliable data for evaluating SNFs for the FY 2022 SNF VBP Program. However, analyses conducted by our contractor since the publication of the September 2nd IFC have found that when July-September 2020 SNF data are compared with July-September 2019 SNF data, the July-September 2020 SNF data showed 25 percent fewer SNF admissions and 26 percent fewer readmissions from a SNF to a hospital. These impacts have affected the reliability of the SNFRM. Generally speaking, the SNFRM's reliability decreases as the sample size and measured outcome (that is, readmissions) decrease. A drop of 25 percent in SNF admissions and 26 percent in readmissions to the hospital from July-September 2020 has significantly reduced the sample size needed to calculate both the measure cohort and outcome for the FY 2022 SNF VBP Program, thus jeopardizing the measure's reliability. Our contractor's analysis using FY 2019 data showed that such changes may lead to a 15 percent decrease in the measure reliability, assessed by the intra-class correlation coefficient (ICC). In addition, the current risk-adjustment model does not factor in COVID-19 or the fact that SNFs are treating different types of patients as a result of the COVID-19 PHE. Nearly 10 percent of SNF residents in July-September 2020 had a current or prior diagnosis of COVID-19, with uneven regional impacts. The SNFRM does not adjust for COVID-19 in the risk-adjustment methodology, as the measure was developed before the pandemic. As a result, risk-adjusted rates, which compare SNFs to each other nationally, are likely to reflect variation in COVID-19 prevalence rather than variation in quality of care. We do not believe that assessing SNFs on a quality measure affected significantly by the varied regional response to the COVID-19 PHE presents a clear picture of the quality of care provided by an individual SNF. The data also demonstrated other important changes in SNF patient case-mix during the PHE for COVID-19, including an 18 percent increase in the proportion of dually eligible residents and a 9 percent increase in the proportion of African-American SNF residents at the facility level. Dually eligible and African-American SNF residents have been disproportionately impacted by COVID, both in terms of morbidity and mortality. In the proposed rule, we stated we are conducting analyses to determine whether and how the SNFRM specifications may need to be updated to account for SNF residents with a primary or secondary diagnosis of COVID-19 for future program years. We also stated we plan to conduct analysis for the SNFPPR measure.
We considered whether we could propose to remove the July 1, 2020-September 30, 2020 data from the updated performance period for the FY 2022 SNF VBP Program Year and calculate the SNFRM using a 9-month performance period (April 1, 2019-December 31, 2019). To determine whether the measure would be reliable using data during this period, which would be closer to 8 months once we remove all SNF stays whose 30-day readmission risk-window extended to or after January 1, 2020, we performed reliability analyses using a formula that relates the reliability of a measure to its intraclass correlation coefficient (ICC), and found that an estimate of reliability using all 12 combinations of potential 8-month data periods from FY 2019 (that Start Printed Page 42506 is, October through May, November through June, and so on)[116] produces an average reliability estimate of 0.367, which is lower than our generally accepted minimum reliability threshold of 0.40.
We also considered substituting the July 1, 2020-September 30, 2020 period with an alternate data period; however, we are limited operationally in terms of which data may be used. Using data from further in the future would cause a delay in the calculation and dissemination of results for the FY 2022 Program. Such a delay could require us to make adjustments to the otherwise applicable Federal per diem rate paid to SNFs in FY 2022 on a delayed basis, which would be an extremely burdensome process for the MACs and a potentially confusing process for SNFs. While using older data is feasible, and we recognize that we adopted a performance period in the September 2nd IFC that duplicated the use of data from a previous performance period, our preference is to use as much new data as possible to assess SNF performance each year and to avoid, where feasible, using the same data as a performance period in multiple program years. Further revising the FY 2022 Program performance period to include older data would create a substantial overlap with the FY 2021 Program's performance period. Such a significant overlap would result in SNFs receiving payments in FY 2022 based largely on the same performance used to assess SNFs for the FY 2021 SNF VBP program year. Using over 80 percent of the same data twice as a performance period could result in some SNFs being penalized (or receiving a bonus) twice for nearly the same performance.
Therefore, due to concerns about the validity of the measure when calculated as currently specified on data during the PHE given the significant changes in SNF patient case volume and facility-level case mix described above, and lacking any viable alternatives, we proposed to suppress the use of SNF readmission measure data for purposes of scoring and payment adjustments in the FY 2022 SNF VBP Program Year, under the proposed Measure Suppression Factor (4) Significant national or regional shortages or rapid or unprecedented changes in: (iii) Patient case volumes or facility-level case mix.
As we stated in the proposed rule, under this suppression policy, for all SNFs participating in the FY 2022 SNF VBP Program, we would use the previously finalized performance period and baseline period to calculate each SNF's RSRR for the SNFRM. Then, we would suppress the use of SNF readmission measure data for purposes of scoring and payment adjustments. Specifically, we proposed to change the scoring methodology to assign all SNFs a performance score of zero in the FY 2022 SNF VBP Program Year. This would result in all participating SNFs receiving an identical performance score, as well as an identical incentive payment multiplier. We would then apply the Low-Volume Adjustment policy as previously finalized in the FY 2019 SNF PPS final rule (83 FR 39278 through 39280). That is, if a SNF has fewer than 25 eligible stays during the performance period for a program year we would assign that SNF a performance score resulting in a net-neutral payment incentive multiplier. SNFs will not be ranked for the FY 2022 SNF VBP Program.
As we stated in the proposed rule, under this policy, we would reduce each participating SNF's adjusted Federal per diem rate for FY 2022 by 2 percentage points and award each participating SNF 60 percent of that 2 percent withhold, resulting in a 1.2 percent payback for the FY 2022 SNF VBP Program Year. We believe this continued application of the 2 percent withhold is required under section 1888(h)(5)(C)(ii)(III) of the Act and that a payback percentage that is spread evenly across all qualifying SNFs is the most equitable way to reduce the impact of the withhold in light of our proposal to award a performance score of zero to all SNFs. Those SNFs subject to the Low-Volume Adjustment policy would receive 100 percent of their 2 percent withhold per the previously finalized policy, increasing the overall payback percentage to an estimated 62.9 percent.
Further, we proposed to provide quarterly confidential feedback reports to SNFs and publicly report the SNFRM rates for the FY 2022 SNF VBP Program Year. However, we stated that we would make clear in the public presentation of those data that the measure has been suppressed for purposes of scoring and payment adjustments because of the effects of the PHE for COVID-19 on the data used to calculate the measure. We proposed to codify this policy at § 413.338(g).
We invited public comment on this proposal. The following is a summary of the public comments we received on the proposed Suppression of the SNFRM for the FY 2022 SNF VBP Program Year, and our responses:
Comment: Many commenters expressed support for the proposal to suppress the SNFRM data for the purposes of scoring and payment adjustments for the FY 2022 SNF VBP Program Year under Measure Suppression Factor (4) Significant national or regional shortages or rapid or unprecedented changes in: (iii) Patient case volumes or facility-level case mix. Commenters agreed with our conclusion that the inclusion of data during the PHE due to COVID-19 would significantly affect the SNF readmission measure and not present a clear picture of the quality of care provided by an individual SNF. Additionally, they noted that CMS provided a fair path forward given the FY 2020 average reliability estimate using FY 2019 data was lower than the minimum reliability threshold.
Response: We thank the commenters for their support.
Comment: One commenter stated that the proposed measure suppression policy violates the provisions of section 1888(h)(6) of the Act, which funds value-based incentive payments via a reduction to SNFs' adjusted Federal per diem rates. The commenter also stated that the proposed suppression policy does not differentiate between high-performing and low-performing SNFs, and therefore, does not make value-based incentive payments as required by statute.
Response: As discussed in the proposed rule, we proposed to suppress the SNFRM due to the impacts of the COVID-19 PHE. Specifically, we have concerns about the validity of the measure when calculated as currently specified using data during the PHE given the significant changes in SNF patient case volume and facility-level case mix. We continue to believe that for purposes of scoring and payment adjustments under the SNF VBP Program, the SNFRM as impacted by the COVID-19 PHE should not be attributed to the participating facility positively or negatively, because the performance scores associated with the SNFRM would not accurately reflect facility performance for national comparison and ranking purposes given the variation in COVID-19 across different geographies and time periods and seen in fluctuating case volumes and case mix. However, due to the SNFRM being the only quality measure authorized for use in the FY 2022 SNF VBP, suppression of the SNFRM would mean we would not be able to calculate SNF performance scores for any SNF or to differentially rank SNFs. Therefore, we Start Printed Page 42507 proposed to change the scoring methodology to assign all SNFs a performance score of zero and effectively rank all SNFs equally in the FY 2022 SNF VBP Program Year.
Comment: Several commenters expressed concerns about publicly reporting SNFRM measure results for the FY 2022 SNF VBP Program Year despite the measure being suppressed because they believe that the publicly reported information may cause public confusion and misrepresent quality of care for a particular SNF. Two commenters also noted that the SNFRM does not adjust for COVID-19 diagnoses and should not be publicly reported until it does.
Response: We proposed to suppress the SNFRM due to the impacts of the COVID-19 PHE for purposes of scoring and payment adjustments because of our concern that we would not be able to make fair, national comparisons of SNFs across the country or to fairly and accurately rank SNFs based only on quality performance and not other exogenous factors related to the PHE for COVID-19. We also believe it is important to balance fairness in performance-based payments with the public's interest in and need for transparency of data from during the COVID-19 PHE, including hospital readmissions information for SNF patients. Therefore, we intend to make the data available on the Provider Data Catalogue (https://data.cms.gov/provider-data/) website. We will make clear in the public presentation of the data that the measure has been suppressed for purposes of scoring and payment adjustments because of the effects of the PHE due to COVID-19. We will also appropriately caveat the data in order to mitigate public confusion and avoid misrepresenting quality of care. SNFs that qualify for the low-volume adjustment policy will not have their risk-standardized readmission rate publicly displayed and an explanatory footnote will be available instead.
We also understand the commenters' concern that the SNFRM does not currently adjust for COVID-19 diagnoses in the risk-adjustment methodology, as the measure was developed before the PHE. We have conducted internal analyses that indicated a large number of patients who were admitted to SNFs had a primary or secondary diagnosis of COVID-19 during their prior proximal hospitalization. The SNFRM does not currently account for COVID-19, and we believe it is important to more fully assess the impact of COVID-19 on the SNFRM, including the following: Whether we should add COVID-19 as a risk-adjustment variable, exclude COVID-19 patients from the denominator, or exclude COVID-19 readmissions from the outcome.
After considering the public comments, we are finalizing our proposal to suppress the SNFRM for the FY 2022 SNF VBP Program Year as proposed and codifying it, as well as the scoring and payment policies we are finalizing for FY 2022, at § 413.338(g) of our regulations.
3. Revision to the SNFRM Risk Adjustment Lookback Period for the FY 2023 SNF VBP Program
In the FY 2021 SNF PPS final rule (85 FR 47624), we finalized the FY 2023 Program performance period as FY 2021 (October 1, 2020-September 30, 2021). In the FY 2016 SNF PPS final rule (80 FR 46418), we finalized that the risk-adjustment model would account for certain risk-factors within 365 days prior to the discharge from the hospital to the SNF (a 365-day lookback period). Under the COVID-19 ECE, SNF qualifying claims for the period January 1, 2020-June 30, 2020 are excepted from the calculation of the SNFRM; using FY 2021 data, this results in at least 3 months of lookback data being available for all SNF stays included in the measure without extending into or beyond June 30, 2020. We proposed instead a 90-day lookback period for risk-adjustment in the FY 2023 performance period (FY 2021 data) only. We stated in the proposed rule that using a 90-day risk-adjustment period would allow us to use the most recent claims available for risk-adjustment, and an identical risk-adjustment lookback period for all stays included in the measure. It also allows us to avoid combining data from both prior to and during the COVID-19 PHE in the risk-adjustment lookback period, which would be necessary if we attempted to maintain a 12-month lookback period due to the COVID-19 ECE. Using a 90-day lookback period for risk-adjustment would allow us to look back 90 days prior to the discharge from the hospital to the SNF for each SNF stay. Analyses conducted on FY 2019 performance data found that when compared to the 365-day lookback period traditionally used, a 90-day lookback period resulted in similar model performance (that is, the C-statistic was nearly identical). We also considered similarly reducing the risk-adjustment lookback period for the applicable FY 2023 Program baseline year which would align the risk-adjustment lookback period for the baseline and performance years in the FY 2023 Program; we invited comments on this consideration.
We invited public comment on the proposed updates to the risk-adjustment lookback period for the FY 2023 performance period.
The following is a summary of the public comments received on the proposed 90-day SNFRM risk-adjustment lookback period for the FY 2023 SNF VBP Program performance period and our responses:
Comment: One commenter recommended continued testing of the 90-day risk-adjustment lookback period for FY 2023, stating that this approach worked well using FY 2019 performance data. The commenter stated that testing with FY 2020 data and analyses of regional effects based on COVID-19 impacts would be informative before finalizing this approach.
Response: We acknowledge the commenter's suggestion to continue testing the 90-day risk-adjustment lookback period for FY 2023 and agree with the importance of continued testing. We note that the analyses we conducted on FY 2019 performance data resulted in nearly identical C-statistics, indicating that the model using a 90-day lookback period performed similarly to the model using a traditional 365-day lookback period. We will continue to test FY 2020 data in a similar fashion, but we believe the results from the FY 2019 data illustrate the model performance for a 90-day lookback period for the FY 2023 performance period.
After considering the public comments, we are finalizing our proposal to use a 90-day lookback period for risk-adjustment in the FY 2023 performance period (FY 2021).
4. Summary of Comments Received on Potential Future Measures for the SNF VBP Program
On December 27, 2020, Congress enacted the Consolidated Appropriations Act, 2021 (CAA) (Pub. L. 116-260). Section 111(a)(1) of Division CC of the CAA amends section 1888(h)(1) of the Act to, with respect to payments for services furnished on or after October 1, 2022, preclude the SNF VBP from applying to a SNF for which there are not a minimum number (as determined by the Secretary) of cases for the measures that apply to the facility for the performance period for the applicable fiscal year, or measures that apply to the facility for the performance period for the applicable fiscal year. Section 111(a)(2) of the CAA amended section 1888(h)(2)(A) of the Act to, with respect to payments for services furnished on or after October 1, 2023, require the Secretary to apply the readmission measure specified under Start Printed Page 42508 section 1888(g)(1) of the Act, and allow the Secretary to apply up to 9 additional measures determined appropriate, which may include measures of functional status, patient safety, care coordination, or patient experience. To the extent that the Secretary decides to apply additional measures, section 1888(h)(2)(A)(ii) of the Act, as amended by section 111(a)(2)(C) of the CAA, requires the Secretary to consider and apply, as appropriate, quality measures specified under section 1899B(c)(1) of the Act. Finally, section 111(a)(3) of the CAA amended section 1888(h) of the Act by adding a new paragraph (12), which requires that the Secretary apply a process to validate the measures and data submitted under the SNF VBP and the SNF QRP, as appropriate, which may be similar to the process specified under the Hospital Inpatient Quality Reporting (IQR) Program for validating inpatient hospital measures. In the proposed rule, we solicited input from stakeholders regarding which measures we should consider adding to the SNF VBP Program. We intend to use future rulemaking to address these new statutory requirements.
Currently, the SNF VBP Program includes only a single quality measure, the SNFRM, which we intend to transition to the SNFPPR measure as soon as practicable. Both the SNFRM and SNFPPR assess the risk-adjusted rate of readmissions to hospitals, for SNF residents within 30 days of discharge from a prior hospital stay. Consistent with amended section 1888(h)(2)(A)(ii) of the Act, in considering which measures might be appropriate to add to the SNF VBP Program, we are considering additional clinical topics such as measures of functional status, patient safety, care coordination, and patient experience, as well as measures on those topics that are utilized in the SNF Quality Reporting Program (QRP). For more information about the SNF QRP measures, please visit https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Skilled-Nursing-Facility-Quality-Reporting-Program/SNF-Quality-Reporting-Program-Measures-and-Technical-Information.
We are also considering measures on clinical topics that are not included in the SNF QRP's measure set because we believe that other clinical topics would be helpful to our efforts to robustly assess the quality of care furnished by SNFs.
In expanding the SNF VBP measure set, we are also considering measures that we already require for Long-Term Care Facilities (LTCFs), which include both SNFs and nursing facilities (NFs), to collect and report under other initiatives. Approximately 94 percent of LTCFs are dually certified as both a SNF and NF (Provider Data Catalog Nursing Homes and Rehab Services Provider Information File January 2021) (https://data.cms.gov/provider-data/dataset/4pq5-n9py). The vast majority of LTCF residents are also Medicare beneficiaries, regardless of whether they are in a Medicare Part A SNF stay, because they are enrolled in Medicare Part B and receive Medicare coverage of certain services provided by the LTCF even if they are a long-term care resident. Therefore, we believe that expanding the SNF VBP measure set to assess the quality of care that SNFs provide to all residents of the facility, regardless of payer, would best represent the quality of care provided to all Medicare beneficiaries in the facility. We requested public comment on whether the measures in an expanded SNF VBP measure set should require SNFs to collect data on all residents in the facility, regardless of payer.
We identified the measures listed in Table 30 as measures we could add to the SNF VBP Program measure set, and we sought comment on those measures, including which of those measures would be best suited for the program. We also solicited public comment on any measures or measure concepts that are not listed in Table 30 that stakeholders believe we should consider for the SNF VBP Program. In considering an initial set of measures with which SNFs should largely be familiar (through the SNF QRP, 5-Star Rating Program and/or the Nursing Home Quality Initiative (NHQI)), we believe we can implement a measure set that would impose minimal additional burden on SNFs.
Start Printed Page 42509
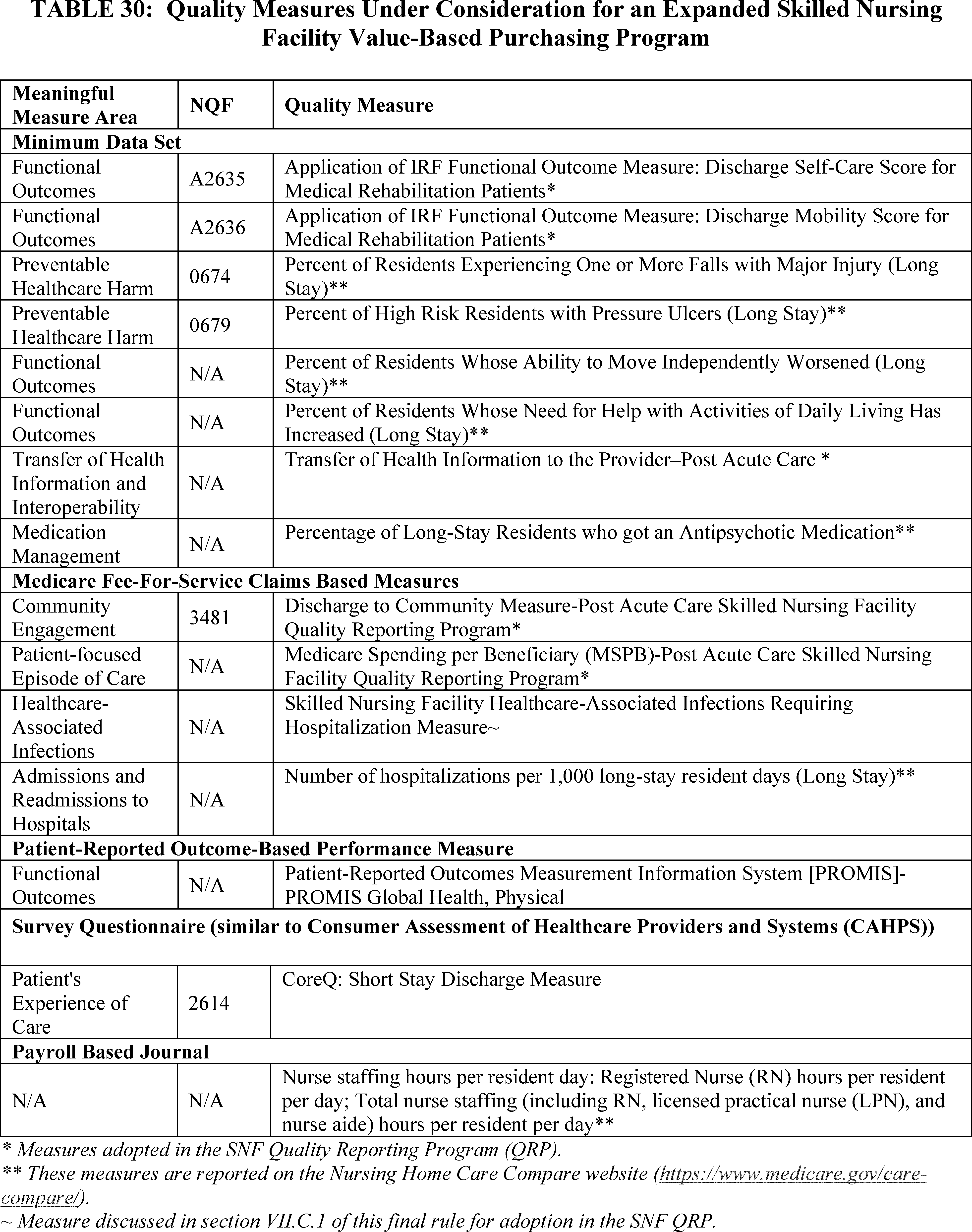
In addition to the staffing measures listed in Table 30 that focus on nurse staffing hours per resident day and that are currently reported on the Nursing Home Care Compare website, we indicated in the proposed rule that we are also interested in measures that focus on staff turnover. We have been developing measures of staff turnover for data that are required to be submitted under section 1128I(g)(4) of the Act, with the goal of making the information publicly available. Through our implementation of the Payroll-Based Journal (PBJ) staffing data collection program, we have indicated that we will be reporting rates of employee turnover in the future (for more information on Start Printed Page 42510 this program, see CMS memorandum QSO-18-17-NH[117] ). As we plan to report employee turnover information in the near future, we also sought comment on inclusion of these measures in the SNF VBP Program.
We are also considering two patient-reported measures (the PROMIS measure and the CoreQ patient experience of care measure), as listed in Table 30, to assess residents' views of their healthcare.
The CoreQ: Short Stay Discharge Measure calculates the percentage of individuals discharged in a 6-month time period from a SNF, within 100 days of admission, who are satisfied with their SNF stay. This patient reported outcome measure is based on the CoreQ: Short Stay Discharge questionnaire that utilizes four items: (1) In recommending this facility to your friends and family, how would you rate it overall; (2) Overall, how would you rate the staff; (3) How would you rate the care you receive; (4) How would you rate how well your discharge needs were met. For additional information about the CoreQ: Short Stay Discharge Measure, please visit https://cmit.cms.gov/CMIT_public/ViewMeasure?MeasureId=3436.
We welcomed public comment on future measures for the SNF VBP Program, and on whether the measures in an expanded SNF VBP measure set should require SNFs to collect data on all residents in the facility, regardless of payer.
The following is a summary of the public comments received on the Request for Comments on Potential Future Measures for the SNF VBP Program:
Comment: Many commenters generally supported the adoption of new measures in the SNF VBP Program. However, many commenters did not support the Percentage of Long-Stay Residents who got an Antipsychotic Medication measure noting concerns with disincentivizing clinically appropriate access to FDA-approved medications, impact on patient care and outcomes, and that the measure is not NQF-endorsed.
A few commenters supported CoreQ: Short Stay Discharge Measure (CoreQ) stating it measures outcomes important to residents. A few commenters expressed concerns that CoreQ may not fully reflect the patient experience and that the measure's questions are vague. A few commenters recommended the use of CAHPS Nursing Home Resident and Family member surveys instead of the CoreQ questionnaire because commenters believe it provides more complete and comprehensive information about a resident's experience and is developed through a more rigorous and independent process. A few commenters supported inclusion of the Skilled Nursing Facility Healthcare-Associated Infections Requiring Hospitalization Measure (HAI) in the SNF VBP Program to support and prioritize improved patient outcomes. A few commenters supported the inclusion of the Medicare Spending per Beneficiary (MSPB) measure because the measure captures elements of care coordination that are important to beneficiaries and the Medicare program. A few commenters did not support the MSPB measure, citing their belief that costs can vary depending upon beneficiary needs and that the measure does not reflect the immediate need or interests of residents or families.
With respect to measures related to staffing turnover, several commenters supported staffing measures that assess the appropriate level of licensed clinical staff such as those that can be derived from the Payroll-Based Journal (PBJ) data collection program, including Registered Nurse (RN) hours per resident per day and total nurse staffing (including RN, licensed practical nurse (LPN), and nurse aide) hours per resident per day. While they supported these PBJ-based staffing measures, commenters strongly recommended that CMS consider staffing turnover to assess patterns and consistency in staffing levels as they are associated with and indicative of quality and safety issues, and high turnover could lead to low quality of care and could disrupt the health, safety, and well-being of patients.
Several commenters expressed some concerns with the inclusion of a staffing measure. One commenter recommended that staffing measures should focus on consistent staffing rather than just collecting data on the number of nursing staff by type. One commenter noted that staffing measures are important to report but expressed concern that staffing measures have not been evaluated for use in value-based purchasing programs, and another commenter suggested that staffing requirements vary across states. A few commenters expressed concerns with the burden of reporting a staffing measure. A few commenters recommended delaying the addition of a staffing measure due to the COVID-19 pandemic.
One commenter supported the inclusion of Patient Reported Outcome Measures (PROMs) as soon as possible and appreciated the consideration of the two PROMs (PROMIS and the CoreQ patient experience of care) for future years. One commenter supported the use of the PROMIS questionnaire, but noted additional resources would be needed for implementation. One commenter recommended that the patient experience measure use minimal questions and take into account the role of caregivers in helping complete the surveys. One commenter recommended that any PROMIS measure considered be reviewed by NQF; this commenter also noted that PROMIS measures were not developed for institutional populations and that CMS should consider the burden to collect, store, and transmit these data.
Many commenters supported the use of patient experience measures in the SNF VBP Program. One commenter recommended that patient experience measures be adjusted for respondent characteristics. One commenter recommended excluding beneficiaries in managed care plans from a patient experience measure, expressing concern that beneficiaries may be unsatisfied with how their stay was managed by their Managed Care/Medicare Advantage Plan and that this would reflect negatively towards the SNF on a patient-reported outcome survey. A few commenters recommended delaying the implementation of patient experience surveys due to the COVID-19 pandemic. One commenter did not support the two patient-reported measures, noting the survey process already includes residents, and suggested that we focus on expanding the survey protocol instead of adding a new measure. This commenter also stated that the questions on the CoreQ measure may not sufficiently capture customer dissatisfaction. Instead, this commenter recommended strengthening and expanding the current CMS survey protocol. One commenter recommended the development and adoption of a standardized patient experience survey for the SNF QRP before potentially being adopted for the SNF VBP Program.
A few commenters recommended inclusion of the NQF 3481, Discharge to Community Measure-Post Acute Care Skilled Nursing Facility Quality Reporting Program measure. A few commenters recommended inclusion of the NQF A2636, Application of IRF Functional Outcome Measure: Discharge Mobility Score for Medical Rehabilitation Patients measure. One commenter recommended inclusion of the Preventable Healthcare Harm—0674 Percent of Residents Experiencing One or More Falls with Major Injury Start Printed Page 42511 measure. One commenter recommended inclusion of the Transfer of Health Information (HI) and Interoperability—Transfer of Health Information to the Provider-Post Acute Care measure to advance CMS' goals of improving patient safety through adoption of EHR and FHIR standards.
Several commenters recommended aligning SNF VBP readmissions measures with the readmission measures used by other CMS programs, including the SNF QRP. One commenter recommended criteria for evaluating which measures should be adopted in the SNF VBP Program, including measures with NQF endorsement, high impact on outcomes/performance, resident quality of life focus, low administrative burden, statistically significant variation among providers, risk-adjustment for social risk factors, and appropriate application to the SNF population and their health status. Many commenters recommended that any new measures added to SNF VBP be NQF-endorsed. One commenter recommended that any new measures should include descriptions of the measure's weight and scoring requirements. Another commenter recommended that CMS balance the need for new quality measures with reducing administrative burden and duplicative reporting in other quality programs. A few commenters recommended a phased approach to adding new measures to the SNF VBP Program. One commenter recommended limiting the number of measures added in the first year in order to avoid diluting the Program's clear focus on readmissions. One commenter noted that adding nine additional measures to the SNF VBP Program would be too aggressive in expanding the measures and recommended adding two or three measures suggesting this would be easier to integrate and allow providers time to prepare. One commenter recommended delaying the addition of measures until after the PHE has ended.
Several commenters expressed support for collecting performance data across payers. One commenter supported that any and all new measures require data on all SNF residents regardless of payer. One commenter did not support moving to all-payer for most measures but did support the inclusion of all residents across payers in the patient experience measure to increase the sample size for an important measure of quality care. A few commenters did not support the inclusion of nursing home residents in the calculation of measure results for the SNF VBP Program noting differences in policies such as limitations on days of care under Medicare Advantage. A few commenters recommended that not all measures should apply to all residents within a nursing home and that there should be a distinction between measures for short-term and long-term stay residents to accommodate the different goals between these two types of residents.
One commenter recommended that CMS focus on adding outcomes-based measures to the SNF VBP Program. A few commenters did not support any new measures based on self-reported MDS data, believing these data are inaccurate. One commenter recommended that measures should incorporate social determinants of health when feasible and applicable. One commenter did not support the inclusion of utilization-based measures.
A few commenters recommended future consideration of new measures for frailty, patient reported outcomes, health equity, and pain, including the following measures: Satisfaction with Participation in Social Roles; Ability to Participate in Social Roles and Activities; Cognitive Function—Abilities; General Life Satisfaction; General Self-Efficacy: Self-Efficacy for Managing Chronic Conditions—Managing Daily Activities, Self-Efficacy for Managing Chronic Conditions—Managing Symptoms, and Self-Efficacy for Managing Chronic Conditions—Managing Medications and Treatment. Another commenter recommended measures of patient and workforce safety and reliability, clinical quality, and caregiver engagement that are evidence-based, targeted, and meaningful to patients and caregivers; this commenter also encouraged the collection of data based on key variables of inequities in patient care for all types of measures. One commenter recommended a small set of population-based measures tied to outcomes, patient-experience and resource use that are not burdensome to report. One commenter recommended that CMS add a risk-adjustment variable for socioeconomic status to the hospital readmission measure for the SNF VBP. One commenter recommended a measure focused on resident "dumping." One commenter recommended a measure comparing the Minimum Data Set section GG: Functional Abilities and Goals with length of stay to develop an outcome ratio to account for patient complexity for facilities with short-term transitional care patients.
One commenter recommended that CMS take steps to ensure the accuracy of reported data. One commenter recommended further clarification of how measure collection may impact providers with low-volume Medicare beneficiaries and whether this program will be extended to nursing facilities. One commenter recommended prioritizing value for residents by returning a higher percentage of withheld funds and utilizing measures that more directly measure outcomes that are important to SNF residents.
Response: We thank the commenters for their responses to this request for comments on potential future measures for the SNF VBP Program. We will take all of this feedback into consideration as we develop our policies for future rulemaking. In addition, as previously indicated, we plan to report SNF employee turnover information in the near future.
C. SNF VBP Performance Period and Baseline Period
1. Background
We refer readers to the FY 2016 SNF PPS final rule (80 FR 46422) for a discussion of our considerations for determining performance periods under the SNF VBP Program. In the FY 2019 SNF PPS final rule (83 FR 39277 through 39278), we adopted a policy whereby we will automatically adopt the performance period and baseline period for a SNF VBP Program Year by advancing the performance period and baseline period by 1 year from the previous program year.
2. Updated Performance Period for the FY 2022 SNF VBP
In response to the PHE for COVID-19, we granted an ECE for SNFs participating in the SNF VBP Program. Under the ECE, SNF qualifying claims for the period January 1, 2020-June 30, 2020 are excepted from the calculation of the SNFRM. Because this ECE excepted data for 6 months of the performance period that we had previously finalized for the FY 2022 SNF VBP Program Year (84 FR 38822), we updated the performance period for that program year in the "Medicare and Medicaid Programs, Clinical Laboratory Improvement Amendments, and Patient Protection and Affordable Care Act: Additional Policy and Regulatory Revisions in Response to the COVID-19 Public Health Emergency" interim final rule with comment ("the September 2nd IFC") (85 FR 54820). Specifically, we finalized that the new performance period for the FY 2022 SNF VBP Program Year would be April 1, 2019-December 31, 2019 and July 1, 2020-September 30, 2020 because we believed that this period, which combined 9 months of data prior to the Start Printed Page 42512 start of the PHE for COVID-19 and 3 months of data after the end of the ECE, would provide sufficiently reliable data for evaluating SNFs for the FY 2022 SNF VBP Program. The following is a summary of the public comments received from the September 2nd IFC regarding the updated FY 2022 performance period.
Comment: One commenter expressed support for the updated performance period, agreeing that using only 6 months of data would not provide reliable results. This commenter encouraged CMS to extend the ECE to include all of 2020 and suspend the SNFRM measure for FY 2022.
Response: We thank this commenter for their support. Additionally, we refer readers to section VIII.B.1. and VIII.B.2. of this final rule, where we have finalized several flexibilities that result in suppressing the SNFRM for FY 2022. Regarding the commenter's suggestion to extend the ECE in section VIII.B.1. of the FY 2022 SNF PPS proposed rule (86 FR 20007), we noted that while we considered extending the ECE, this option would result in less than 12 months of data being used to calculate the single readmissions measure in the Program for multiple program years, which we do not believe would provide an accurate assessment of the quality of care provided in SNFs. This option would also leave no comprehensive data available for us to provide confidential performance feedback to providers nor for monitoring and to inform decision-making for potential future programmatic changes.
Comment: One commenter opposed this updated performance period, noting that CMS would not receive reliable data from CY 2020, and recommended that CMS not score facilities for FY 2020 performance or make associated payment adjustments for the FY 2022 SNF VBP Program and resume the program in subsequent years once reliable performance data consistent with measure specifications are available. Another commenter also expressed concern that any CY 2020 data would be unreliable and urged CMS to extend the ECE and suspend the SNFRM for FY 2022.
Response: At the time of the publication of the September 2nd IFC, we adopted a performance period that we believed would provide sufficiently reliable data for evaluating SNF performance (85 FR 54837) and would be the most operationally feasible option that included 12 months of data. Since the publication of the September 2nd IFC, additional data have become available, and we have conducted analyses on the impact of the COVID-19 PHE. As described more fully in section VIII.B.2. of this final rule, we continue to have concerns about the validity of the measure when calculated as currently specified on data during the PHE (specifically, July 1, 2020 through September 30, 2020) as well as the reliability of the measure when calculated using data from a shorter timeframe. Further, we considered many alternatives to the performance period we adopted in the September 2nd IFC and believed that none were sufficient for scoring and payment. Therefore, we are finalizing our proposal to suppress the SNFRM for the FY 2022 SNF VBP Program Year for scoring and payment purposes. However, for the purposes of measure rate calculation and public reporting, to ensure we are providing providers and the public with as much information as possible, we believe the performance period adopted in the September 2nd IFC is the most appropriate given the alternatives.
Upon consideration of public comments, we are finalizing the revised Performance Period for the FY 2022 SNF VBP Program (April 1, 2019 through December 31, 2019 and July 1, 2020 through September 30, 2020) as established in the September 2nd IFC. This performance period will be used to calculate each SNF's RSRR for the SNFRM and we will publicly report these results on the Provider Data Catalogue website (https://data.cms.gov/provider-data/), while making it clear in the public presentation of those data that we are suppressing the use of those data for purposes of scoring and payment adjustments in the FY 2022 SNF VBP Program.
3. Performance Period for the FY 2023 SNF VBP Program
In the FY 2021 SNF PPS final rule (85 FR 47624), we finalized that the performance period for the FY 2023 SNF VBP Program Year would be October 1, 2020-September 30, 2021 (FY 2021) and the baseline period would be FY 2019 (October 1, 2018-September 30, 2019). We did not propose any updates to the performance period and baseline period previously finalized for FY 2023.
Comment: One commenter did not support the previously finalized performance period for FY 2023 noting that it includes CY 2020 data that is not adjusted to account for the impact of COVID-19 and is unreliable.
Response: We are considering whether we should make changes to the SNFRM specifications to account for changes in SNF admission and/or hospital readmission patterns that we have observed during the COVID-19 PHE. Any substantive changes to the measure specifications would be proposed in future rulemaking.
We noted in the proposed rule (86 FR 20011 through 20012) that we had considered alternatives to the previously finalized performance period for FY 2023. We specifically considered modifying the performance period for the FY 2023 program year to Calendar Year 2021 (January 1, 2021 through December 31, 2021). However, CY 2021 data are available later than FY 2021 data and would likely result in a delay calculating SNFRM scores for SNFs and a subsequent delay in the application of payment incentives for the FY 2023 program year.
We acknowledge that the COVID-19 PHE extends into both performance period options. As noted in section VIII.B.2., we intend to conduct analyses to determine whether and how the SNFRM specifications may need to be updated to account for SNF residents with a diagnosis of COVID-19 for future program years. Following the completion of these analyses, SNF readmission measure specifications may account for changes in SNF admission and/or hospital readmission patterns that we have observed during the PHE, if needed.
We invited public comment on this alternative to the previously finalized performance period for the FY 2023 SNF VBP program but did not receive any comments on this alternative.
4. Performance Period and Baseline Period for the FY 2024 SNF VBP Program
Under the policy finalized in the FY 2019 SNF PPS final rule (83 FR 39277 through 39278), for the FY 2024 program year, the performance period would be FY 2022 and the baseline period would be FY 2020. However, under the ECE, SNF qualifying claims for a 6-month period in FY 2020 (January 1, 2020 through June 30, 2020) are excepted from the calculation of the SNFRM, which means that we will not have a full year of data to calculate the SNFRM for the FY 2020 baseline period. Moreover, as described in more detail in section VIII.B.2. of this final rule, we are finalizing the suppression of the SNFRM for the FY 2022 program year, in part because there are concerns about the validity of the measure when calculated as currently specified on data during the PHE (specifically, July 1, 2020 through September 30, 2020) given the significant changes in SNF patient case volume and facility-level case mix described above. As the SNF VBP Start Printed Page 42513 Program uses only a single measure calculated on 1 year of data and uses each year of data first as a performance period and then later on as a baseline period in the Program, the removal of 9 months of data in light of the COVID-19 PHE as described above will necessarily result in data being used more than once in the Program. Therefore, to ensure enough data are available to reliably calculate the SNFRM, we proposed that FY 2019 data be used for the baseline period for the FY 2024 program year. We also considered using FY 2021, which will be the baseline period for the FY 2025 program year under our current policy. However, it is operationally infeasible for us to calculate the baseline for the FY 2024 program year using FY 2021 data in time to establish the performance standards for that program year at least 60 days prior to the start of the performance period, as required under section 1888(h)(3)(C) of the Act.
We invited public comment on this proposal. The following is a summary of the public comments received on the proposed baseline period for the FY 2024 SNF VBP program and our responses:
Comment: One commenter noted concern that using FY 2019 data as the baseline period for the FY 2024 program year may not provide relevant or comparable data for the performance period in FY 2024. Therefore, the commenter did not support the proposed FY 2024 baseline period.
Response: Due to measure reliability and operational feasibility considerations noted in section VIII.C.5. of this final rule, as well as FY 2019 data were not impacted by the COVID-19 PHE, we continue to believe that using FY 2019 data as the baseline period for the FY 2024 performance period is appropriate. We are also conducting testing to assess whether any updates should be made to the specifications of the SNF readmission measure to account for changes in SNF admission and/or hospital readmission patterns that we have observed during the PHE which may impact the FY 2024 performance period's comparability to the FY 2024 baseline period. Additionally, we believe that using FY 2019 data will be both relevant and comparable as the FY 2019 SNFRM data would reflect care delivered prior to the start of the Secretary's declaration of a PHE for COVID-19. With regard to the FY 2024 performance period, we believe facilities will have had time to adapt to the changes in care delivery needed to respond to the COVID-19 pandemic.
After considering the public comments, we are finalizing our proposal to use FY 2019 data for the FY 2024 baseline period as proposed.
D. Performance Standards
1. Background
We refer readers to the FY 2017 SNF PPS final rule (81 FR 51995 through 51998) for a summary of the statutory provisions governing performance standards under the SNF VBP Program and our finalized performance standards policy. We adopted the final numerical values for the FY 2022 performance standards in the FY 2020 SNF PPS final rule (84 FR 38822) and adopted the final numerical values for the FY 2023 performance standards in the FY 2021 SNF PPS final rule (85 FR 47625). We also adopted a policy allowing us to correct the numerical values of the performance standards in the FY 2019 SNF PPS final rule (83 FR 39276 through 39277).
We did not propose any changes to these performance standard policies in the proposed rule.
2. SNF VBP Performance Standards Correction Policy
In the FY 2019 SNF PPS final rule (83 FR 39276 through 39277), we finalized a policy to correct numerical values of performance standards for a program year in cases of errors. We also finalized that we will only update the numerical values for a program year one time, even if we identify a second error, because we believe that a one-time correction will allow us to incorporate new information into the calculations without subjecting SNFs to multiple updates. We stated that any update we make to the numerical values based on a calculation error will be announced via the CMS website, listservs, and other available channels to ensure that SNFs are made fully aware of the update. In the FY 2021 SNF PPS final rule (85 FR 47625), we amended the definition of "Performance standards" at § 413.338(a)(9), consistent with these policies finalized in the FY 2019 SNF PPS final rule, to reflect our ability to update the numerical values of performance standards if we determine there is an error that affects the achievement threshold or benchmark. We did not propose any changes to the performance standards correction policy in the proposed rule.
3. Performance Standards for the FY 2024 Program Year
As discussed in section VIII.C.5. of this final rule, we are finalizing our proposal to use FY 2019 data for the baseline period for the FY 2024 program year. Based on this updated baseline period and our previously finalized methodology for calculating performance standards (81 FR 51996 through 51998), the final numerical values for the FY 2024 program year performance standards are as follows:
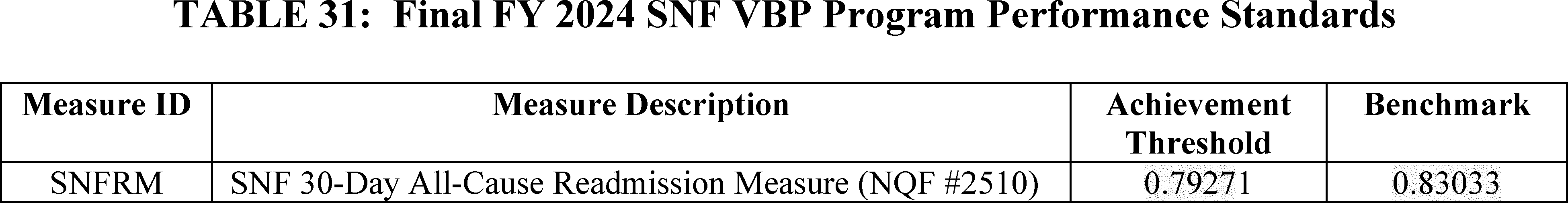
E. SNF VBP Performance Scoring
We refer readers to the FY 2017 SNF PPS final rule (81 FR 52000 through 52005) for a detailed discussion of the scoring methodology that we have finalized for the Program. We also refer readers to the FY 2018 SNF PPS final rule (82 FR 36614 through 36616) for discussion of the rounding policy we adopted. We also refer readers to the FY 2019 SNF PPS final rule (83 FR 39278 through 39281), where we adopted: (1) A scoring policy for SNFs without sufficient baseline period data, (2) a scoring adjustment for low-volume SNFs, and (3) an extraordinary circumstances exception policy.
In the FY 2022 SNF PPS proposed rule, we proposed to suppress the SNFRM for the FY 2022 program year due to the impacts of the PHE for COVID-19. Specifically, for FY 2022 scoring, we proposed that for all SNFs participating in the FY 2022 SNF VBP Program, we would use performance period data from April 1, 2019 through December 31, 2019 and July 1, 2020 through September 30, 2020 and baseline period data from October 1, 2017 through September 30, 2018, Start Printed Page 42514 which we previously finalized to calculate each SNF's RSRR for the SNFRM. Then, we would assign all SNFs a performance score of zero. This would result in all participating SNFs receiving an identical performance score, as well as an identical incentive payment multiplier. We stated in the proposed rule that we would then apply the Low-Volume Adjustment policy as previously finalized in the FY 2019 SNF PPS final rule (83 FR 39278 through 39280). That is, if a SNF has fewer than 25 eligible stays during the performance period for a program year we would assign that SNF a performance score resulting in a net-neutral payment incentive multiplier. SNFs would not be ranked for the FY 2022 SNF VBP Program.
The following is a summary of the public comments received on the proposal to use a special scoring policy for FY 2022 and our responses:
Comment: One commenter expressed support for our proposed adjustments to FY 2022 scoring and payments if the SNFRM is suppressed given the unprecedented circumstances caused by the PHE due to COVID-19.
Response: We thank this commenter for its support.
Comment: One commenter suggested an alternative of basing payment adjustments on performance scores from the FY 2021 SNF VBP Program Year.
Response: We did consider using alternative performance periods for the FY 2022 SNF VBP Program Year, as noted in section VIII.B.2. of the proposed rule. However, we believe using entirely the same data (both the exact same performance and baseline period data) for both the FY 2021 and FY 2022 program years would provide no new information for SNFs or the public, particularly information during the COVID-19 PHE, and may have the unintended effect of mitigating incentives for providers to improve between the overlapping program years or unfairly rewarding or penalizing SNFs by repeating the FY 2021 program.
Comment: Several commenters expressed concern that our proposed measure suppression and scoring policy for FY 2022 might violate sections 1888(h)(4)(B) and 1888(h)(5)(C)(ii)(II)(cc) of the Act, which state that the Secretary shall rank SNF performance scores from low to high, and for SNFs in the lowest 40 percent ranking, to apply a payment rate for services less than the payment rate that would otherwise apply without the SNF VBP Program.
Response: As discussed in section VIII.D.2. of the proposed rule and this final rule, we proposed and are finalizing suppression of the SNFRM due to the impacts of the COVID-19 PHE. Specifically, we have concerns about the validity of the measure when calculated as currently specified on data during the PHE given the significant changes in SNF patient case volume and facility-level case mix and lacking any viable alternatives. We stated in the proposed rule our belief that for purposes of scoring and payment adjustments under the SNF VBP Program, the SNFRM as impacted by the COVID-19 PHE should not be attributed to the participating facility positively or negatively. We believe that using SNFRM data that has been impacted by the PHE due to COVID-19 could result in performance scores that do not accurately reflect SNF performance for making national comparisons and ranking purposes given the variation in COVID-19 across different geographies and time periods and seen in fluctuating case volumes and case mix. Due to the SNFRM being the only quality measure authorized for use in the FY 2022 SNF VBP, suppression of the SNFRM would mean we would not be able to calculate SNF performance scores for any SNF nor to differentially rank SNFs. Therefore, we proposed to change the scoring methodology to assign all SNFs a performance score of zero and effectively rank all SNFs equally in the FY 2022 SNF VBP Program Year.
After considering the public comments, we are finalizing our proposed special scoring policy for the FY 2022 program year as proposed and codifying it at § 413.338(g) of our regulations.
F. SNF Value-Based Incentive Payments
We refer readers to the FY 2018 SNF PPS final rule (82 FR 36616 through 36621) for discussion of the exchange function methodology that we have adopted for the Program, as well as the specific form of the exchange function (logistic, or S-shaped curve) that we finalized, and the payback percentage of 60 percent. We adopted these policies for FY 2019 and subsequent fiscal years.
We also discussed the process that we undertake for reducing SNFs' adjusted Federal per diem rates under the Medicare SNF PPS and awarding value-based incentive payments in the FY 2019 SNF PPS final rule (83 FR 39281 through 39282).
As discussed in sections VIII.B.2. and VIII.E of this final rule, we are finalizing the suppression of the SNFRM for the FY 2022 program year and assigning all SNFs a performance score of zero, which would result in all participating SNFs receiving an identical performance score, as well as an identical incentive payment multiplier.
In the proposed rule, we proposed to reduce each participating SNF's adjusted Federal per diem rate for FY 2022 by 2 percentage points and to award each participating SNF 60 percent of that 2 percent withhold, resulting in a 1.2 percent payback for the FY 2022 program year. We believe this continued application of the 2 percent withhold is required under section 1888(h)(5)(C)(ii)(III) of the Act and that a payback percentage that is spread evenly across all SNFs is the most equitable way to reduce the impact of the withhold in light of our proposal to award a performance score of zero to all SNFs. We proposed that those SNFs subject to the Low-Volume Adjustment policy would receive 100 percent of their 2 percent withhold per the previously finalized policy, increasing the overall payback percentage to an estimated 62.9 percent. We proposed to codify this policy at § 413.338(g).
We invited public comment on this proposed change to the SNF VBP payment policy for the FY 2022 program year.
The following is a summary of the public comments received on the proposed SNF Value-Based Incentive Payments and our responses:
Comment: The majority of commenters supported suppressing the SNFRM due to the COVID-19 pandemic. However, many commenters expressed concern regarding the payment amount in the proposed payment policy for the FY 2022 SNF VBP Program Year. Several commenters recommended that we not reduce each eligible SNF's adjusted Federal per diem rate by 2 percent, or that we return all of the 2 percent withhold to eligible SNFs. Several commenters also noted that if we must proceed with returning only a portion of the 2 percent withhold, we should return 70 percent of the 2 percent withhold rather than 60 percent and that this approach would be reasonable and the most fair given that all providers will be awarded the same incentive payment multiplier and because we are not basing distribution on performance. One commenter recommended that CMS pause the application of SNF incentive payment adjustments for performance years impacted by the PHE.
Response: Though we acknowledge that the COVID-19 PHE has had unprecedented impacts on SNFs, we believe maintaining the 60 percent payback percentage will best provide for the stability and sustainability of the Medicare Program, as well as the stability and sustainability of other Start Printed Page 42515 programs funded by the Medicare Trust Fund. Increasing the payback percentage to 70 percent would lead to higher SNF PPS baseline spending that would lower the estimated savings realized by the Medicare Trust Fund in FY 2022 by 19 percent. Specifically, we estimate that increasing the payback percentage to 70 percent would reduce estimated savings from $191.64 million to $154.85 million for that fiscal year. We note that the SNF VBP Program was designed to be a cost-saving program for Medicare. We refer readers to the FY 2018 SNF PPS final rule (82 FR 36619 through 36621) for a discussion of the factors we considered when we specified the 60 percent payback percentage, including a balance between the number of SNFs that receive a positive payment adjustment, the marginal incentives for all SNFs to reduce hospital readmissions and make broad-based care quality improvements, and the Medicare Program's long-term sustainability.
Regarding the recommendation to pause the application of SNF incentive payment adjustments for all performance years impacted by the PHE, we believe that the updated FY 2022 performance period that we adopted in the September 2nd IFC and are finalizing in this final rule, as well as the measure suppression and special scoring and payment policies we are finalizing in this final rule, serve to mitigate the impact of the PHE on SNF VBP performance scores for the FY 2022. Therefore, we do not believe further actions to the SNF VBP Program's incentive payment adjustments would be beneficial to the program at this time. We are continuing to analyze data that may impact the FY 2023 Program.
Comment: One commenter specifically noted that this proposal to reduce each eligible SNF's adjusted Federal per diem rate by the applicable 2 percent and then adjust the resulting amounts by a value-based incentive payment amount equal to 60 percent of the total reduction "disconnects payment from quality," and risks "rewarding bad actors and penalizing good performers."
Response: We do not believe that assessing SNFs on a quality measure affected significantly by the varied regional response to the COVID-19 PHE presents a clear picture of the quality of care provided by an individual SNF. Facility-level morbidity and mortality data have been shown to be significantly and disproportionately affected by COVID-19 due to changes in SNF patient case-mix. We are concerned that making payment incentive adjustments using the scoring and payment methodologies specified at § 413.338(c) and (d) could unintentionally award payment incentives to SNFs whose high performance was driven by one or more COVID-19 related factors, such as low COVID-19 prevalence in their locale, lower SNF admissions because of changes in health care patterns, or higher rates of mortality because of conditions related to COVID-19, rather than due to better performance.
Comment: One commenter encouraged CMS to consider modifications to statutory language for situations such as the PHE due to COVID-19 where the Administration could hold participating SNFs harmless.
Response: We thank the commenter for its suggestion and we will take it under consideration.
Comment: One commenter suggested that in addition to the policy we proposed, we should also exclude COVID-19 diagnosed patients from the eligible case count, which would lead to additional SNFs having insufficient numbers of cases and thus receiving a low-volume adjustment rather than a penalty. One commenter questioned whether the 25 or more eligible stay requirement for applying the low-volume adjustment policy is appropriate given the impacts of COVID-19 on SNF residents and facilities and suggested that CMS eliminate all payment cuts for FY 2022.
Response: We do not agree with the commenter's suggestion to exclude COVID-19 diagnosed patients from the SNFRM eligible case count for the FY 2022 program year. As explained above, we believe that our proposal to suppress the SNFRM for FY 2022 scoring and payment adjustment purposes appropriately mitigates the effects of the PHE due to COVID-19. Additionally, excluding COVID-19 diagnosed patients from the eligible case count would negatively affect the Program's impact on the Medicare Trust Fund because it would increase the number of SNFs eligible for the Low-Volume Adjustment policy who receive a net-neutral incentive payment multiplier.
As further detailed below, we believe that the minimum of 25 eligible stays for the performance period as a threshold for applying the Low-Volume Adjustment policy is appropriate and important to maintain for FY 2022, even though we are suppressing the SNFRM measure for scoring and payment adjustment purposes. As noted previously, eliminating all payment cuts for the FY 2022 program year would threaten the stability and maintenance of the SNF VBP Program. We note that while this program is designed to be a cost-savings program, during the COVID-19 PHE, smaller SNFs (those with 45 or fewer eligible stays) and a disproportionate number of rural SNFs have been more vulnerable to unexpected changes in payment or policy as compared to larger SNFs. For the FY 2022 program, we are seeking in particular to protect small and rural SNFs from unexpected or adverse impacts of policies and not applying the LVA would result in those SNFs receiving a deduction when they otherwise would not have. Specifically, when we estimated the impact of the LVA in the upcoming FY 2022 program year, we found that, overall 28 percent of SNFs qualified for the LVA (including 43 percent of all rural SNFs and only 22 percent of all urban SNFs). In comparison to a standard program year, 17 percent of all SNFs would receive the LVA (28.2 percent rural and 12.8 percent urban).
After considering the public comments, we are finalizing our proposed special payment policy for the FY 2022 program year as proposed and codifying it at § 413.338(g) of our regulations.
G. Public Reporting on the Nursing Home Compare Website or a Successor Website
1. Background
Section 1888(g)(6) of the Act requires the Secretary to establish procedures to make SNFs' performance information on SNF VBP Program measures available to the public on the Nursing Home Compare website or a successor website, and to provide SNFs an opportunity to review and submit corrections to that information prior to its publication. We began publishing SNFs' performance information on the SNFRM in accordance with this directive and the statutory deadline of October 1, 2017. In December 2020, we retired the Nursing Home Compare website and are now using the Provider Data Catalogue website (https://data.cms.gov/provider-data/) to make quality data available to the public, including SNF VBP performance information.
Additionally, section 1888(h)(9)(A) of the Act requires the Secretary to make available to the public certain information on SNFs' performance under the SNF VBP Program, including SNF performance scores and their ranking. Section 1888(h)(9)(B) of the Act requires the Secretary to post aggregate information on the Program, including the range of SNF performance scores and the number of SNFs receiving value-based incentive payments, and Start Printed Page 42516 the range and total amount of those payments.
In the FY 2017 SNF PPS final rule (81 FR 52009), we discussed the statutory requirements governing public reporting of SNFs' performance information under the SNF VBP Program. In the FY 2018 SNF PPS final rule (82 FR 36622 through 36623), we finalized our policy to publish SNF VBP Program performance information on the Nursing Home Compare or successor website after SNFs have had an opportunity to review and submit corrections to that information under the two-phase Review and Correction process that we adopted in the FY 2017 SNF PPS final rule (81 FR 52007 through 52009) and for which we adopted additional requirements in the FY 2018 SNF PPS final rule. In the FY 2018 SNF PPS final rule, we also adopted requirements to rank SNFs and adopted data elements that we will include in the ranking to provide consumers and stakeholders with the necessary information to evaluate SNFs' performance under the Program (82 FR 36623).
As discussed in section VIII.B.2. of this final rule, we are finalizing the suppression of the SNFRM for the FY 2022 program year due to the impacts of the PHE for COVID-19. Under this finalized proposal, for all SNFs participating in the FY 2022 SNF VBP Program, we will use the performance period we adopted in the September 2nd IFC and are finalizing in this final rule, as well as the previously finalized baseline period to calculate each SNF's RSRR for the SNFRM. We are also finalizing our proposal to assign all SNFs a performance score of zero. This will result in all participating SNFs receiving an identical performance score, as well as an identical incentive payment multiplier. Further, we are finalizing our proposal to apply the Low-Volume Adjustment policy as previously finalized in the FY 2019 SNF PPS final rule (83 FR 39278 through 39280). That is, if a SNF has fewer than 25 eligible stays during the performance period for a program year, we will assign that SNF a performance score resulting in a net-neutral payment incentive multiplier.
While we will publicly report the SNFRM rates for the FY 2022 program year, we will make clear in the public presentation of those data that we are suppressing the use of those data for purposes of scoring and payment adjustments in the FY 2022 SNF VBP Program given the significant changes in SNF patient case volume and facility-level case mix described above. Under our finalized policy, SNFs will not be ranked for the FY 2022 SNF VBP Program.
2. Data Suppression Policy for Low-Volume SNFs
In the FY 2020 SNF PPS final rule (84 FR 38823 through 38824), we adopted a data suppression policy for low-volume SNF performance information. Specifically, we finalized that we will suppress the SNF performance information available to display as follows: (1) If a SNF has fewer than 25 eligible stays during the baseline period for a program year, we will not display the baseline risk-standardized readmission rate (RSRR) or improvement score, although we will still display the performance period RSRR, achievement score, and total performance score if the SNF had sufficient data during the performance period; (2) if a SNF has fewer than 25 eligible stays during the performance period for a program year and receives an assigned SNF performance score as a result, we will report the assigned SNF performance score and we will not display the performance period RSRR, the achievement score, or improvement score; and (3) if a SNF has zero eligible cases during the performance period for a program year, we will not display any information for that SNF. We codified this policy in the FY 2021 SNF PPS final rule (85 FR 47626) at § 413.338(e)(3)(i), (ii), and (iii).
As discussed in section VIII.B.2. of this final rule, we are finalizing the suppression of the SNFRM for the FY 2022 program year and our proposals for scoring and payment in FY 2022, including applying the Low-Volume Adjustment policy as previously finalized. That is, if a SNF has fewer than 25 eligible stays during the performance period for FY 2022 (April 1, 2019 through December 31, 2019 and July 1, 2020 through September 30, 2020), we will assign that SNF a performance score resulting in a net-neutral payment incentive multiplier.
3. Public Reporting of SNF VBP Performance Information on Nursing Home Compare or a Successor Website
Section 1888(h)(9)(A) of the Act requires that the Secretary make available to the public on the Nursing Home Compare website or a successor website information regarding the performance of individual SNFs for a fiscal year, including the performance score for each SNF for the fiscal year and each SNF's ranking, as determined under section 1888(h)(4)(B) of the Act. Additionally, section 1888(h)(9)(B) of the Act requires that the Secretary periodically post aggregate information on the SNF VBP Program on the Nursing Home Compare website or a successor website, including the range of SNF performance scores, and the number of SNFs receiving value-based incentive payments and the range and total amount of those payments. In the FY 2018 SNF PPS final rule (82 FR 36622 through 36623), we finalized our policy to publish SNF measure performance information under the SNF VBP Program on Nursing Home Compare.
In the FY 2021 SNF PPS final rule (85 FR 47626), we finalized an amendment to § 413.338(e)(3) to reflect that we will publicly report SNF performance information on the Nursing Home Compare website or a successor website located at https://data.cms.gov/provider-data//. We did not propose any changes to the public reporting policies in the proposed rule.
H. Update and Codification of the Phase One Review and Correction Claims "Snapshot" Policy
In the FY 2017 SNF PPS final rule (81 FR 52007 through 52009), we adopted a two-phase review and corrections process for SNFs' quality measure data that will be made public under section 1888(g)(6) of the Act and SNF performance information that will be made public under section 1888(h)(9) of the Act. We detailed the process for requesting Phase One corrections and finalized a policy whereby we would accept Phase One corrections to a quarterly report provided during a calendar year until the following March 31.
In the FY 2020 SNF PPS final rule (84 FR 38824 through 38835), we updated this policy to reflect a 30-day Phase One Review and Correction deadline rather than through March 31st following receipt of the performance period quality measure quarterly report.
In the FY 2021 SNF PPS final rule (85 FR 47626 through 47627), we updated the 30-day deadline for Phase One Review and Correction and codified the policy at § 413.338(e)(1). Under the updated policy, beginning with the baseline period quality report issued on or after October 1, 2020 that contains the baseline period measure rate and underlying claim information used to calculate the measure rate for the applicable program year, SNFs have 30 days following the date that CMS provides those reports to review and submit corrections to the data contained in those reports. We also stated that if the issuance dates of these reports are significantly delayed or need to be shifted for any reason, we would notify SNFs through routine communication channels including, but not limited to Start Printed Page 42517 memos, emails, and notices on the CMS SNF VBP website at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/SNF-VBP/SNF-VBP-Page.
We proposed to include a Phase One Review and Correction claims "snapshot" policy beginning with the baseline period and performance period quality measure quarterly reports issued on or after October 1, 2021. This proposed policy would limit the Phase One Review and Correction to errors made by CMS or its contractors when calculating a SNF's readmission measure rate and would not allow corrections to the underlying administrative claims data used to calculate those rates. Under this proposed policy, the administrative claims data we use to calculate a SNF's readmission measure rate for purposes of a baseline period or performance period for a given SNF VBP Program Year would be held constant (that is, frozen in a "snapshot") from the time we extract it for that purpose. This proposal would align the review and correction policy for the SNF VBP Program with the review and correction policy we have adopted for other value-based purchasing programs, including the Hospital Readmissions Reduction Program (HRRP), Hospital-Acquired Condition (HAC) Reduction Program, and Hospital VBP Program.
For purposes of this program, we proposed to calculate the SNF readmission measure rates using a static "snapshot" of claims updated as of 3 months following the last index SNF admission in the applicable baseline period or performance period. The source of the administrative claims data we use to calculate the SNF readmission measure is the Medicare Provider Analysis and Review (MedPAR). For example, if the last index SNF admission date for the applicable baseline period or performance period is September 30, 2019, we would extract the administrative claims data from the MedPAR file as that data exists on December 31, 2019. SNFs would then receive their SNF readmission measure rate and accompanying stay-level information in their confidential quality measure quarterly reports, and they would have an opportunity to review and submit corrections to our calculations as part of the Phase One corrections process. However, SNFs would not be able to correct any of the underlying administrative claims data (for example, a SNF discharge destination code) we use to generate the measure rate.
The use of a data "snapshot" enables us to provide as timely quality data as possible, both to SNFs for the purpose of quality improvement and to the public for the purpose of transparency. After the claims "snapshot" is taken through our extraction of the data from MedPAR, it takes several months to incorporate other data needed for the SNF readmission measure calculations, generate and check the calculations, as well as program, populate, and deliver the confidential quarterly reports and accompanying data to SNFs. Because several months lead-time is necessary after acquiring the input data to generate these calculations, if we were to delay our data extraction point beyond the date that is 3 months after the last SNF index admission attributable to a baseline period or performance period, we believe this would create an unacceptably long delay both for SNFs to receive timely data for quality improvement and transparency, and, incentive payments for purposes of this program. Therefore, we believe that a 3-month claims "run-out" period between the date of the last SNF index admission and the date of the data extraction is a reasonable period that allows SNFs time to correct their administrative claims or add any missing claims before those claims are used for measure calculation purposes while enabling us to timely calculate the measure. If unforeseen circumstances require the use of additional months of claims "run-out", that is, more than 3 months, we would notify SNFs through routine communication channels including, but not limited to, memos, emails, quarterly reports and notices on the CMS SNF VBP website at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/SNF-VBP/SNF-VBP-Page.
We believe this proposed policy would address both fairness and operational concerns associated with calculating measure rates and would provide consistency across value-based purchasing programs.
We also proposed to codify this policy in our regulations by revising § 413.338(e)(1) to remove the policies that would no longer be applicable beginning October 1, 2021 and state the newly proposed policy that would be effective, if finalized, on October 1, 2021.
We invited public comment on this proposal to update the Phase One Review and Correction policy.
The following is a summary of the public comments received on our proposal to Update and Codify the Phase One Review and Correction Claims "Snapshot" Policy and our responses:
Comment: A few commenters supported updating the Phase One Review and Corrections policy to align with the review and corrections policy in other value-based purchasing programs.
Response: We thank the commenters for their support.
After considering the comments, we are finalizing the updated Phase One Review and Corrections claims "snapshot" policy as proposed and codifying it at § 413.338(e)(1) of our regulations.
I. Update to the Instructions for Requesting an ECE in § 413.338(d)(4)(ii) of the SNF VBP Regulations
We proposed to update the instructions for a SNF to request an extraordinary circumstances exception (ECE). Specifically, we proposed to update the URL for our QualityNet website from QualityNet.org to QualityNet.cms.gov. We also proposed to update the email address that a SNF must use to send an ECE request. We also proposed to remove the separate reference to newspapers because newspapers are already included in the broader term "media articles." We proposed to update § 413.338(d)(4)(ii) of our regulations to reflect these changes.
We invited public comment on this proposal.
The following is a summary of the public comments received on our proposal to Update the Instructions for Requesting an ECE in § 413.338(d)(4)(ii) of the SNF VBP Regulations and our responses:
Comment: A few commenters supported our proposal to update the instructions to request an ECE in the SNF VBP regulations.
Response: We thank these commenters for their support.
After considering the public comments, we are finalizing our proposal to update the instructions for requesting an ECE in the SNF VBP regulations and codifying it at § 413.338(d)(4)(ii) of our regulations. However, due to operational concerns, we are updating the regulation text to specify that a SNF may request an exception in the form and manner specified by CMS on the SNF VBP website, which will include the appropriate email address to which a SNF can send its ECE request.
IX. Technical Correction for § 483.90(d)
In the July 18, 2019 "Medicare and Medicaid Programs; Requirements for Long-Term Care Facilities: Regulatory Provisions To Promote Efficiency, and Start Printed Page 42518 Transparency" proposed rule, we proposed a technical correction to revise § 483.90(d)(1) and add paragraph (d)(3) to correct an error in the Code of Federal Regulations (CFR) (84 FR 34737).
Previously, on July 13, 2017, we issued a correcting amendment entitled, "Medicare and Medicaid Programs; Reform of Requirements for Long-Term Care Facilities" correcting amendment (82 FR 32256) to correct technical and typographical errors identified in the October 2016 "Medicare and Medicaid Programs; Reform of Requirements for Long-Term Care Facilities" final rule (81 FR 68688). This document inadvertently removed revisions made to § 483.90(d), which were finalized in the October 2016 final rule. Specifically, the rule finalized requirements at § 483.90(d) (incorrectly labeled paragraph (c) in the October 2016 final rule) for facilities to—(1) provide sufficient space and equipment in dining, health services, recreation, living, and program areas to enable staff to provide residents with needed services as required by these standards and as identified in each resident's assessment and plan of care at § 483.90(d)(1)); (2) maintain all mechanical, electrical, and patient care equipment in safe operating condition at § 483.90(d)(2); and (3) conduct regular inspection of all bed frames, mattresses, and bed rails, if any, as part of a regular maintenance program to identify areas of possible entrapment. When bed rails and mattresses are used and purchased separately from the bed frame, the facility must ensure that the bed rails, mattress, and bed frame are compatible at § 483.90(d)(3).
We did not receive comments in response to this proposal. Therefore, we are finalizing this technical correction, as proposed, to revise § 483.90(d)(1) and add paragraph (d)(3).
X. Collection of Information Requirements
Consistent with our April 15, 2021 (86 FR 19954) proposed rule, this final rule will not impose any new or revised "collection of information" requirements or burden as it pertains to CMS. For the purpose of this section of the preamble, collection of information is defined under 5 CFR 1320.3(c) of the Paperwork Reduction Act of 1995's (PRA) (44 U.S.C. 3501 et seq.) implementing regulations. Consequently, this rule is not subject to the requirements of the PRA.
In section VII.C.1. of this final rule, we are finalizing the adoption of the SNF HAIs Requiring Hospitalization measure beginning with the FY 2023 SNF QRP. The measure is claims-based. All claims-based measures are calculated using data that are already reported to the Medicare program for payment purposes. Since the data source for this measure is Medicare fee-for-service claims, there is no additional burden for SNFs.
In section VII.C.2. of this final rule, we are finalizing the adoption of the COVID-19 Vaccination Coverage among Healthcare Personnel (HCP) measure beginning with the FY 2023 SNF QRP. SNFs must submit data on the measure through the CDC/National Healthcare Safety Network (NHSN). We note that the CDC will account for the burden associated with the COVID-19 Vaccination Coverage among HCP measure collection under OMB control number 0920-1317 (current expiration January 31, 2024). However, the CDC currently has a PRA waiver for the collection and reporting of vaccination data under section 321 of the National Childhood Vaccine Injury Act of 1986 (Pub. L. 99-660, enacted on November 14, 1986) (NCVIA).[118] We refer readers to section XI.A.5. of this final rule for an estimate of the burden to SNFs, and note that the CDC will include it in a revised information collection request under said control number.
In section VII.C.3. of this final rule, we are finalizing our proposal to update the Transfer of Health (TOH) Information to the Patient—Post Acute Care (PAC) measure to exclude residents discharged home under the care of an organized home health service or hospice. This measure was adopted in the FY 2020 SNF PPS final rule (84 FR 38728) and the associated burden was accounted for under OMB control number 0938-1140 (CMS-10387) (current expiration November 30, 2022). The update will not affect the requirements and burden that are currently approved under that control number.
In section VII.G.3. of this final rule, we are finalizing our proposal that SNFs submit data on the COVID-19 Vaccination among HCP measure through the CDC/National Healthcare Safety Network (NHSN). The NHSN is a secure, internet-based surveillance system that is maintained by the CDC and provided free of charge to healthcare facilities including SNFs.
While the NHSN is currently not utilized by SNFs for purposes of meeting the SNF QRP requirements, nursing homes were enrolled in the NHSN in 2020 and are currently submitting mandatory COVID-19 data through the Long-term Care Facility COVID-19 module (https://www.cdc.gov/nhsn/ltc/covid19/index.html). As such, there is no additional information collection burden related to the onboarding and training of SNF providers to utilize this system.
In section VIII.B.2. of this final rule, we are finalizing our proposal to suppress the Skilled Nursing Facility 30-Day All-Cause Readmission Measure (SNFRM) for scoring and payment purposes for the FY 2022 SNF VBP Program Year. Because the data source for this quality measure is Medicare fee-for-service claims, there is no additional burden for SNFs. All claims-based measures can be calculated based on data that are already reported to the Medicare program for payment purposes.
XI. Economic Analyses
A. Regulatory Impact Analysis
1. Statement of Need
This final rule updates the FY 2022 SNF prospective payment rates as required under section 1888(e)(4)(E) of the Act. It also responds to section 1888(e)(4)(H) of the Act, which requires the Secretary to provide for publication in the Federal Register before the August 1 that precedes the start of each FY, the unadjusted Federal per diem rates, the case-mix classification system, and the factors to be applied in making the area wage adjustment. As these statutory provisions prescribe a detailed methodology for calculating and disseminating payment rates under the SNF PPS, we do not have the discretion to adopt an alternative approach on these issues.
2. Introduction
We have examined the impacts of this final rule as required by Executive Order 12866 on Regulatory Planning and Review (September 30, 1993), Executive Order 13563 on Improving Regulation and Regulatory Review (January 18, 2011), the Regulatory Flexibility Act (RFA, September 19, 1980, Pub. L. 96-354), section 1102(b) of the Act, section 202 of the Unfunded Mandates Reform Act of 1995 (UMRA, March 22, 1995; Pub. L. 104-4), Executive Order 13132 on Federalism (August 4, 1999), and the Congressional Review Act (5 U.S.C. 804(2)).
Executive Orders 12866 and 13563 direct agencies to assess all costs and benefits of available regulatory alternatives and, if regulation is necessary, to select regulatory approaches that maximize net benefits Start Printed Page 42519 (including potential economic, environmental, public health and safety effects, distributive impacts, and equity). Executive Order 13563 emphasizes the importance of quantifying both costs and benefits, of reducing costs, of harmonizing rules, and of promoting flexibility. This rule has been designated an economically significant rule, under section 3(f)(1) of Executive Order 12866. Accordingly, we have prepared a regulatory impact analysis (RIA) as further discussed below. Also, the rule has been reviewed by OMB.
3. Overall Impacts
This rule updates the SNF PPS rates contained in the SNF PPS final rule for FY 2021 (85 FR 47594). We estimate that the aggregate impact would be an increase of approximately $410 million in Part A payments to SNFs in FY 2022. This reflects a $411 million increase from the update to the payment rates and a $1.2 million decrease due to the proposed reduction to the SNF PPS rates to account for the recently excluded blood-clotting factors (and items and services related to the furnishing of such factors) in section 1888(e)(2)(A)(iii)(VI) of the Act. We note that these impact numbers do not incorporate the SNF VBP Program reductions that we estimate would total $191.64 million in FY 2022. We would note that events may occur to limit the scope or accuracy of our impact analysis, as this analysis is future-oriented, and thus, very susceptible to forecasting errors due to events that may occur within the assessed impact time period.
In accordance with sections 1888(e)(4)(E) and (e)(5) of the Act and implementing regulations at § 413.337(d), we are updating the FY 2021 payment rates by a factor equal to the market basket index percentage change reduced by the forecast error adjustment and the productivity adjustment to determine the payment rates for FY 2022. The impact to Medicare is included in the total column of Table 32. When proposing the SNF PPS rates for FY 2022, we proposed a number of standard annual revisions and clarifications mentioned elsewhere in this final rule (for example, the proposed update to the wage and market basket indexes used for adjusting the Federal rates).
The annual update in this rule applies to SNF PPS payments in FY 2022. Accordingly, the analysis of the impact of the annual update that follows only describes the impact of this single year. Furthermore, in accordance with the requirements of the Act, we will publish a rule or notice for each subsequent FY that will provide for an update to the payment rates and include an associated impact analysis.
4. Detailed Economic Analysis
The FY 2022 SNF PPS payment impacts appear in Table 32. Using the most recently available data, in this case FY 2020, we apply the current FY 2021 CMIs, wage index and labor-related share value to the number of payment days to simulate FY 2021 payments. Then, using the same FY 2020 data, we apply the FY 2022 CMIs, wage index and labor-related share value to simulate FY 2022 payments. We would note that, given that this same data is being used for both parts of this calculation, as compared to other analyses discussed in this final rule which compare data from FY 2020 to data from other fiscal years, any issues discussed throughout this final rule with regard to data collected in FY 2020 will not cause any difference in this economic analysis. We tabulate the resulting payments according to the classifications in Table 32 (for example, facility type, geographic region, facility ownership), and compare the simulated FY 2021 payments to the simulated FY 2022 payments to determine the overall impact. The breakdown of the various categories of data in Table 32 follows:
- The first column shows the breakdown of all SNFs by urban or rural status, hospital-based or freestanding status, census region, and ownership.
- The first row of figures describes the estimated effects of the various proposed changes on all facilities. The next six rows show the effects on facilities split by hospital-based, freestanding, urban, and rural categories. The next nineteen rows show the effects on facilities by urban versus rural status by census region. The last three rows show the effects on facilities by ownership (that is, government, profit, and non-profit status).
- The second column shows the number of facilities in the impact database.
- The third column shows the effect of the proposed annual update to the wage index. This represents the effect of using the most recent wage data available. The total impact of this change is 0.0 percent; however, there are distributional effects of the proposed change.
- The fourth column shows the effect of all of the changes on the FY 2022 payments. The update of 1.2 percent is constant for all providers and, though not shown individually, is included in the total column. It is projected that aggregate payments would increase by 1.2 percent, assuming facilities do not change their care delivery and billing practices in response.
As illustrated in Table 32, the combined effects of all of the changes vary by specific types of providers and by location. For example, due to changes in this final rule, rural providers would experience a 1.6 percent increase in FY 2022 total payments. Finally, we note that we did not include in Table 32 the distributional impacts associated with the blood-clotting factor exclusion because the reduction is so minor that it does not have any visible effect on the distributional impacts included in the Table 32.
Start Printed Page 42520

5. Impacts for the SNF QRP for FY 2022
Estimated impacts for the SNF QRP are based on analysis discussed in section IX.B. of this final rule. The SNF QRP requirements add no additional burden to the active collection under OMB control number #0938-1140 (CMS-10387; expiration November 30, 2022).
In accordance with section 1888(e)(6)(A)(i) of the Act, the Secretary must reduce by 2 percentage points the annual payment update applicable to a SNF for a fiscal year if the SNF does not comply with the requirements of the SNF QRP for that fiscal year. In section VII.A. of this final rule, we discuss the method for applying the 2 percentage point reduction to SNFs that fail to meet the SNF QRP requirements. As discussed in section VII.C. of this final rule, we are finalizing the adoption of two new measures to the SNF QRP beginning with the FY 2023 SNF QRP: SNF Healthcare-Associated Infections Requiring Hospitalization Measure (SNF-HAI) and the COVID-19 Vaccination Coverage among Healthcare Personnel (HCP) measure. The SNF-HAI measure is a claims-based measure, and therefore, would impose no additional burden to the SNFs.
We believe that the burden associated with the SNF QRP is the time and effort associated with complying with the non-claims-based measures requirements of the SNF QRP. Although the burden associated with the COVID-19 Vaccination Coverage among HCP measure is not accounted for under the CDC PRA package currently approved under OMB control number 0920-1317 due to the NCVIA waiver the cost and burden is discussed here and will be included in a revised information collection request for 0920-1317.
Consistent with the CDC's experience of collecting data using the NHSN, we estimate that it would take each SNF an average of 1 hour per month to collect data for the COVID-19 Vaccination Start Printed Page 42521 Coverage among HCP measure and enter it into NHSN. We have estimated the time to complete this entire activity, since it could vary based on provider systems and staff availability. We believe it would take an administrative assistant from 45 minutes up to 1 hour and 15 minutes to enter this data into NHSN. For the purposes of calculating the costs associated with the collection of information requirements, we obtained mean hourly wages from the U.S. Bureau of Labor Statistics' May 2019 National Occupational Employment and Wage Estimates.[119] To account for overhead and fringe benefits, we have doubled the hourly wage. These amounts are detailed in Table 33.

Based on this time range, it would cost each SNF between $27.47 and $45.78 each month or an average cost of $36.62 each month, and between $329.64 and $549.36 each year, or an average cost of $439.44 each year. We believe the data submission for the COVID-19 Vaccination Coverage among HCP measure would cause SNFs to incur additional average burden of 12 hours per year for each SNF and a total annual burden of 180,936 hours for all SNFs. The estimated annual cost across all 15,078 SNFs in the U.S. for the submission of the COVID-19 Vaccination Coverage among HCP measure would be between $4,970,312 and $8,283,250.08, and an average of $6,625,872.
We recognize that many SNFs may also be reporting other COVID-19 data to HHS. However, we believe the benefits of reporting data on the COVID-19 Vaccination Coverage among HCP measure to assess whether SNFs are taking steps to limit the spread of COVID-19 among their HCP, reduce the risk of transmission of COVID-19 within their facilities, and to help sustain the ability of SNFs to continue serving their communities throughout the PHE and beyond outweigh the costs of reporting. We welcomed comments on the estimated time to collect data and enter it into NHSN.
We did not receive any comments on the estimated time to collect data and enter it into NHSN, and are finalizing the revisions as proposed.
6. Impacts for the SNF VBP Program
The estimated impacts of the FY 2022 SNF VBP Program are based on historical data from February 1, 2019 to September 30, 2019. In section VIII.B.2. of this final rule, we discuss the suppression of the SNFRM for the FY 2022 program year. As finalized, we will award each participating SNF 60 percent of their 2 percent withhold, except those SNFs subject to the low-volume scoring adjustment, which would each receive 100 percent of their 2 percent withhold. We estimated that the low-volume scoring adjustment would increase the 60 percent payback percentage for FY 2022 by approximately 2.9 percentage points (or $14.8 million), resulting in a payback percentage for FY 2022 that is 62.9 percent of the estimated $516.2 million in withheld funds for that fiscal year. Based on the 60 percent payback percentage (as modified by the low-volume scoring adjustment), we estimated that we will redistribute approximately $324.5 million in value-based incentive payments to SNFs in FY 2022, which means that the SNF VBP Program is estimated to result in approximately $191.6 million in savings to the Medicare Program in FY 2022.
7. Impacts for Long Term Care Facilities: Physical Environment Requirements Technical Correction
There are no impacts associated with this technical correction.
8. Alternatives Considered
As described in this section, we estimated that the aggregate impact for FY 2022 under the SNF PPS would be an increase of approximately $410 million in Part A payments to SNFs. This reflects a $411 million increase from the update to the payment rates, and a $1.2 million decrease due to the proposed reduction to the SNF PPS rates to account for the recently excluded blood-clotting factors (and items and services related to the furnishing of such factors) in section 1888(e)(2)(A)(iii)(VI) of the Act.
Section 1888(e) of the Act establishes the SNF PPS for the payment of Medicare SNF services for cost reporting periods beginning on or after July 1, 1998. This section of the statute prescribes a detailed formula for calculating base payment rates under the SNF PPS, and does not provide for the use of any alternative methodology. It specifies that the base year cost data to be used for computing the SNF PPS payment rates must be from FY 1995 (October 1, 1994, through September 30, 1995). In accordance with the statute, we also incorporated a number of elements into the SNF PPS (for example, case-mix classification methodology, a market basket index, a wage index, and the urban and rural distinction used in the development or adjustment of the Federal rates). Further, section 1888(e)(4)(H) of the Act specifically requires us to disseminate the payment rates for each new FY through the Federal Register, and to do so before the August 1 that precedes the start of the new FY; accordingly, we are not pursuing alternatives for this process.
With regard to the alternatives considered related to the other provisions contained in this final rule, such as the methodology for calculating the proportional reduction to the rates to account for the exclusion of blood clotting factors from SNF consolidated billing, we discuss any alternatives considered within those sections.
With regard to the SNF VBP Program measure suppression policy, we discuss alternatives considered within those sections.
9. Accounting Statement
As required by OMB Circular A-4 (available online at https://obamawhitehouse.archives.gov/omb/circulars_a004_a-4/), in Tables 34, 35, and 36, we have prepared an accounting Start Printed Page 42522 statement showing the classification of the expenditures associated with the provisions of this final rule for FY 2022. Tables 32 and 34 provide our best estimate of the possible changes in Medicare payments under the SNF PPS as a result of the policies in this final rule, based on the data for 15,560 SNFs in our database. Table 35 provides our best estimate of the possible changes in Medicare payments under the SNF VBP as a result of the policies we have proposed for this program. Tables 33 and 36 provide our best estimate of the additional cost to SNFs to submit the data for the SNF QRP as a result of the policies in this final rule.


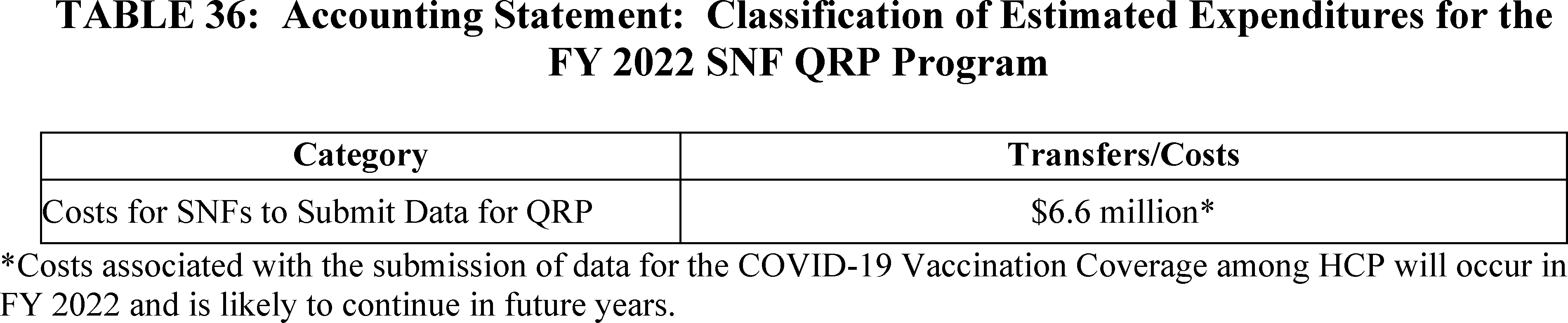
10. Conclusion
This rule updates the SNF PPS rates contained in the SNF PPS final rule for FY 2021 (85 FR 47594). Based on the above, we estimate that the overall payments for SNFs under the SNF PPS in FY 2022 are projected to increase by approximately $410 million, or 1.2 percent, compared with those in FY 2021. We estimate that in FY 2022, SNFs in urban and rural areas would experience, on average, a 1.1 percent increase and 1.0036 percent increase, respectively, in estimated payments compared with FY 2021. Providers in the rural South Atlantic region would experience the largest estimated increase in payments of approximately 2.6 percent. Providers in the rural New England region would experience the smallest estimated increase in payments of 0.2 percent.
B. Regulatory Flexibility Act Analysis
The RFA requires agencies to analyze options for regulatory relief of small entities, if a rule has a significant impact on a substantial number of small entities. For purposes of the RFA, small entities include small businesses, non-profit organizations, and small governmental jurisdictions. Most SNFs and most other providers and suppliers are small entities, either by reason of their non-profit status or by having revenues of $30 million or less in any 1 year. We utilized the revenues of individual SNF providers (from recent Medicare Cost Reports) to classify a small business, and not the revenue of a larger firm with which they may be affiliated. As a result, for the purposes of the RFA, we estimate that almost all SNFs are small entities as that term is used in the RFA, according to the Small Business Administration's latest size standards (NAICS 623110), with total revenues of $30 million or less in any 1 year. (For details, see the Small Business Administration's website at http://www.sba.gov/category/navigation-structure/contracting/contracting-officials/eligibility-size-standards). In addition, approximately 20 percent of SNFs classified as small entities are non-profit organizations. Finally, individuals and states are not included in the definition of a small entity.
This rule would update the SNF PPS rates contained in the SNF PPS final Start Printed Page 42523 rule for FY 2021 (85 FR 47594). Based on the above, we estimate that the aggregate impact for FY 2022 would be an increase of $410 million in payments to SNFs, resulting from the SNF market basket update to the payment rates, reduced by the impact of excluding blood clotting factors (and items and services related to the furnishing of such factors) from SNF consolidated billing under section 1888(e)(2)(A)(iii)(VI) and (e)(4)(G)(iii) of the Act. While it is projected in Table 32 that all providers would experience a net increase in payments, we note that some individual providers within the same region or group may experience different impacts on payments than others due to the distributional impact of the FY 2022 wage indexes and the degree of Medicare utilization.
Guidance issued by the Department of Health and Human Services on the proper assessment of the impact on small entities in rulemakings, utilizes a cost or revenue impact of 3 to 5 percent as a significance threshold under the RFA. In their March 2021 Report to Congress (available at http://www.medpac.gov/docs/default-source/reports/mar21_medpac_ch7_sec.pdf), MedPAC states that Medicare covers approximately 9 percent of total patient days in freestanding facilities and 16 percent of facility revenue (March 2020 MedPAC Report to Congress, 224). As indicated in Table 32, the effect on facilities is projected to be an aggregate positive impact of 1.2 percent for FY 2022. As the overall impact on the industry as a whole, and thus on small entities specifically, is less than the 3 to 5 percent threshold discussed previously, the Secretary has determined that this final rule will not have a significant impact on a substantial number of small entities for FY 2022.
In addition, section 1102(b) of the Act requires us to prepare a regulatory impact analysis if a rule may have a significant impact on the operations of a substantial number of small rural hospitals. This analysis must conform to the provisions of section 604 of the RFA. For purposes of section 1102(b) of the Act, we define a small rural hospital as a hospital that is located outside of an MSA and has fewer than 100 beds. This final rule will affect small rural hospitals that: (1) Furnish SNF services under a swing-bed agreement or (2) have a hospital-based SNF. We anticipate that the impact on small rural hospitals will be a positive impact. Moreover, as noted in previous SNF PPS final rules (most recently, the one for FY 2021 (85 FR 47594)), the category of small rural hospitals is included within the analysis of the impact of this final rule on small entities in general. As indicated in Table 32, the effect on facilities for FY 2022 is projected to be an aggregate positive impact of 1.2 percent. As the overall impact on the industry as a whole is less than the 3 to 5 percent threshold discussed above, the Secretary has determined that this final rule will not have a significant impact on a substantial number of small rural hospitals for FY 2022.
C. Unfunded Mandates Reform Act Analysis
Section 202 of the Unfunded Mandates Reform Act of 1995 also requires that agencies assess anticipated costs and benefits before issuing any rule whose mandates require spending in any 1 year of $100 million in 1995 dollars, updated annually for inflation. In 2021, that threshold is approximately $158 million. This final rule will impose no mandates on state, local, or tribal governments or on the private sector.
D. Federalism Analysis
Executive Order 13132 establishes certain requirements that an agency must meet when it issues a proposed rule (and subsequent final rule) that imposes substantial direct requirement costs on state and local governments, preempts state law, or otherwise has federalism implications. This final rule will have no substantial direct effect on state and local governments, preempt state law, or otherwise have federalism implications.
E. Congressional Review Act
This final regulation is subject to the Congressional Review Act provisions of the Small Business Regulatory Enforcement Fairness Act of 1996 (5 U.S.C. 801 et seq.) and has been transmitted to the Congress and the Comptroller General for review.
F. Regulatory Review Costs
If regulations impose administrative costs on private entities, such as the time needed to read and interpret this final rule, we should estimate the cost associated with regulatory review. Due to the uncertainty involved with accurately quantifying the number of entities that will review the rule, we assume that the total number of unique commenters on this year's proposed rule will be the number of reviewers of this final rule. We acknowledge that this assumption may understate or overstate the costs of reviewing this rule. It is possible that not all commenters reviewed this year's proposed rule in detail, and it is also possible that some reviewers chose not to comment on that proposed rule. For these reasons, we believe that the number of commenters on this year's proposed rule is a fair estimate of the number of reviewers of this final rule.
We also recognize that different types of entities are in many cases affected by mutually exclusive sections of the final rule, and therefore, for the purposes of our estimate we assume that each reviewer reads approximately 50 percent of the rule.
Using the national mean hourly wage data from the May 2020 BLS Occupational Employment Statistics (OES) for medical and health service managers (SOC 11-9111), we estimate that the cost of reviewing this rule is $114.24 per hour, including overhead and fringe benefits https://www.bls.gov/oes/current/oes_nat.htm. Assuming an average reading speed, we estimate that it would take approximately 4 hours for the staff to review half of the proposed rule. For each SNF that reviews the rule, the estimated cost is $456.96 (4 hours × $114.24). Therefore, we estimate that the total cost of reviewing this regulation is $156,280.32 ($442.96 × 342 reviewers).
In accordance with the provisions of Executive Order 12866, this final rule was reviewed by the Office of Management and Budget.
I, Chiquita Brooks-LaSure, Administrator of the Centers for Medicare & Medicaid Services, approved this document on July 21, 2021.
Start List of Subjects
List of Subjects
42 CFR Part 411
- Diseases
- Medicare
- Reporting and recordkeeping requirements
42 CFR Part 413
- Principles of reasonable cost reimbursement; payment for end-stage renal disease services; optional prospectively determined payment rates for skilled nursing facilities; payment for acute kidney injury dialysis
42 CFR Part 483
- Grant programs—health
- Health facilities
- Health professions
- Health records
- Medicaid
- Medicare
- Nursing homes
- Nutrition
- Reporting and recordkeeping requirements
- Safety
42 CFR Part 489
- Health facilities
- Medicare
- Reporting and recordkeeping requirements
End List of Subjects
For the reasons set forth in the preamble, the Centers for Medicare & Medicaid Services amends 42 CFR chapter IV as set forth below:
Start Part Start Printed Page 42524
PART 411—EXCLUSIONS FROM MEDICARE AND LIMITATIONS ON MEDICARE PAYMENT
End Part Start Amendment Part
1. The authority citation for part 411 continues to read as follows:
End Amendment Part
42 U.S.C. 1302, 1395w-101 through 1395w-152, 1395hh, and 1395nn.
End Authority Start Amendment Part
2. Amend § 411.15 by—
End Amendment Part Start Amendment Part
a. Revising paragraphs (p)(2)(xiii) through (xvi);
End Amendment Part Start Amendment Part
b. Redesignating paragraph (p)(2)(xvii) as (p)(2)(xviii); and
End Amendment Part Start Amendment Part
c. Adding new paragraph (p)(2)(xvii).
End Amendment Part
The revisions and addition read as follows:
Particular services excluded from coverage.
* * * * *
(p) * * *
(2) * * *
(xiii) Those chemotherapy items identified, as of July 1, 1999, by HCPCS codes J9000-J9020, J9040-J9151, J9170-J9185, J9200-J9201, J9206-J9208, J9211, J9230-J9245, and J9265-J9600, and as of January 1, 2004, by HCPCS codes A9522, A9523, A9533, and A9534 (as subsequently modified by CMS), and any additional chemotherapy items identified by CMS.
(xiv) Those chemotherapy administration services identified, as of July 1, 1999, by HCPCS codes 36260-36262, 36489, 36530-36535, 36640, 36823, and 96405-96542 (as subsequently modified by CMS), and any additional chemotherapy administration services identified by CMS.
(xv) Those radioisotope services identified, as of July 1, 1999, by HCPCS codes 79030-79440 (as subsequently modified by CMS), and any additional radioisotope services identified by CMS.
(xvi) Those customized prosthetic devices (including artificial limbs and their components) identified, as of July 1, 1999, by HCPCS codes L5050-L5340, L5500-L5611, L5613-L5986, L5988, L6050-L6370, L6400-6880, L6920-L7274, and L7362-L7366 (as subsequently modified by CMS) and any additional customized prosthetic devices identified by CMS, which are delivered for a resident's use during a stay in the SNF and intended to be used by the resident after discharge from the SNF.
(xvii) Those blood clotting factors indicated for the treatment of patients with hemophilia and other bleeding disorders identified, as of July 1, 2020, by HCPCS codes J7170, J7175, J7177-J7183, J7185-J7190, J7192-J7195, J7198-J7203, J7205, and J7207-J7211 (as subsequently modified by CMS) and items and services related to the furnishing of such factors, and any additional blood clotting factors identified by CMS and items and services related to the furnishing of such factors.
* * * * *
Start Part
PART 413—PRINCIPLES OF REASONABLE COST REIMBURSEMENT; PAYMENT FOR END-STAGE RENAL DISEASE SERVICES; PROSPECTIVELY DETERMINED PAYMENT RATES FOR SKILLED NURSING FACILITIES; PAYMENT FOR ACUTE KIDNEY INJURY DIALYSIS
End Part Start Amendment Part
3. The authority citation for part 413 continues to read as follows:
End Amendment Part Start Authority
42 U.S.C. 1302, 1395d(d), 1395f(b), 1395g, 1395l(a), (i), and (n), 1395x(v), 1395hh, 1395rr, 1395tt, and 1395ww.
End Authority Start Amendment Part
4. Amend § 413.338 by revising paragraphs (d)(4)(ii) and (e)(1) and adding paragraph (g) to read as follows:
End Amendment Part
Skilled nursing facility value-based purchasing program.
* * * * *
(d) * * *
(4) * * *
(ii) A SNF may request an exception within 90 days of the date that the extraordinary circumstances occurred in the form and manner specified by CMS on the SNF VBP website at https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/SNF-VBP/Extraordinary-Circumstance-Exception-. The request must include a completed Extraordinary Circumstances Request form (available on https://qualitynet.cms.gov/) and any available evidence of the impact of the extraordinary circumstances on the care that the SNF furnished to patients including, but not limited to, photographs and media articles.
* * * * *
(e) * * *
(1) CMS will provide quarterly confidential feedback reports to SNFs on their performance on the SNF readmission measure. Beginning with the baseline period and performance period quality measure quarterly reports issued on or after October 1, 2021, which contain the baseline period and performance period measure rates, respectively, SNFs will have 30 days following the date CMS provides each of these reports to review and submit corrections to the SNF readmission measure rates contained in that report. The administrative claims data used to calculate a SNF's readmission measure rates are not subject to review and correction under this paragraph (e)(1). All correction requests must be accompanied by appropriate evidence showing the basis for the correction to the SNF readmission measure rates.
* * * * *
(g) Special rules for the FY 2022 SNF VBP Program. (1) CMS will calculate a SNF readmission measure rate for each SNF based on its performance on the SNF readmission measure during the performance period specified by CMS for fiscal year 2022, but CMS will not calculate a performance score for any SNF using the methodology described in paragraphs (d)(1) and (2) of this section. CMS will instead assign a performance score of zero to each SNF, with the exception of those SNFs qualifying for the low-volume scoring adjustment described in paragraph (d)(3) of this section.
(2) CMS will calculate the value-based incentive payment adjustment factor for each SNF using a performance score of zero and will then calculate the value-based incentive payment amount for each SNF using the methodology described in paragraph (c)(2)(ii) of this section. CMS will then apply low-volume scoring adjustment described in paragraph (d)(3) of this section.
(3) CMS will provide confidential feedback reports to SNFs on their performance on the SNF readmission measure in accordance with paragraphs (e)(1) and (2) of this section.
(4) CMS will publicly report SNF performance on the SNF readmission measure in accordance with paragraph (e)(3) of this section.
Start Part
PART 483—REQUIREMENTS FOR STATES AND LONG TERM CARE FACILITIES
End Part Start Amendment Part
5. The authority citation for part 483 continues to read as follows:
End Amendment Part Start Authority
42 U.S.C. 1302, 1320a-7, 1395i, 1395hh and 1396r.
End Authority Start Amendment Part
6. Amend § 483.90 by revising paragraph (d) to read as follows:
End Amendment Part
Physical environment.
* * * * *
(d) Space and equipment. The facility must—
(1) Provide sufficient space and equipment in dining, health services, recreation, living, and program areas to enable staff to provide residents with needed services as required by these standards and as identified in each resident's assessment and plan of care;
(2) Maintain all mechanical, electrical, and patient care equipment in safe operating condition; and Start Printed Page 42525
(3) Conduct regular inspection of all bed frames, mattresses, and bed rails, if any, as part of a regular maintenance program to identify areas of possible entrapment. When bed rails and mattresses are used and purchased separately from the bed frame, the facility must ensure that the bed rails, mattress, and bed frame are compatible.
* * * * *
Start Part
PART 489—PROVIDER AGREEMENTS AND SUPPLIER APPROVAL
End Part Start Amendment Part
7. The authority citation for part 489 is revised to read as follows:
End Amendment Part Start Authority
42 U.S.C. 1302, 1395i-3, 1395x, 1395aa(m), 1395cc, 1395ff, and 1395hh.
End Authority Start Amendment Part
8. Amend § 489.20 by—
End Amendment Part Start Amendment Part
a. Revising paragraphs (s)(13) through (16);
End Amendment Part Start Amendment Part
b. Redesignating paragraph (s)(17) as paragraph (s)(18); and
End Amendment Part Start Amendment Part
c. Adding new paragraph (s)(17).
End Amendment Part
The revisions and addition read as follows:
Basis commitments.
* * * * *
(s) * * *
(13) Those chemotherapy items identified, as of July 1, 1999, by HCPCS codes J9000-J9020, J9040-J9151, J9170-J9185, J9200-J9201, J9206-J9208, J9211, J9230-J9245, and J9265-J9600, and as of January 1, 2004, by HCPCS codes A9522, A9523, A9533, and A9534 (as subsequently modified by CMS), and any additional chemotherapy items identified by CMS.
(14) Those chemotherapy administration services identified, as of July 1, 1999, by HCPCS codes 36260-36262, 36489, 36530-36535, 36640, 36823, and 96405-96542 (as subsequently modified by CMS), and any additional chemotherapy administration services identified by CMS.
(15) Those radioisotope services identified, as of July 1, 1999, by HCPCS codes 79030-79440 (as subsequently modified by CMS), and any additional radioisotope services identified by CMS.
(16) Those customized prosthetic devices (including artificial limbs and their components) identified, as of July 1, 1999, by HCPCS codes L5050-L5340, L5500-L5611, L5613-L5986, L5988, L6050-L6370, L6400-6880, L6920-L7274, and L7362-L7366 (as subsequently modified by CMS) and any additional customized prosthetic devices identified by CMS, which are delivered for a resident's use during a stay in the SNF and intended to be used by the resident after discharge from the SNF.
(17) Those blood clotting factors indicated for the treatment of patients with hemophilia and other bleeding disorders identified, as of July 1, 2020, by HCPCS codes J7170, J7175, J7177-J7183, J7185-J7190, J7192-J7195, J7198-J7203, J7205, and J7207-J7211 (as subsequently modified by CMS) and items and services related to the furnishing of such factors, and any additional blood clotting factors identified by CMS and items and services related to the furnishing of such factors.
* * * * *
Start Signature
Dated: July 27, 2021.
Xavier Becerra,
Secretary, Department of Health and Human Services.
End Signature
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4120-01-P
BILLING CODE 4120-01-C
BILLING CODE 4210-01-P
BILLING CODE 4120-01-C
[FR Doc. 2021-16309 Filed 7-29-21; 4:15 pm]
BILLING CODE 4120-01-P
What Services Are Included In The Consolidated Billing Of The Snf Pps?
Source: https://www.federalregister.gov/documents/2021/08/04/2021-16309/medicare-program-prospective-payment-system-and-consolidated-billing-for-skilled-nursing-facilities
Posted by: reyeswherestants1985.blogspot.com

0 Response to "What Services Are Included In The Consolidated Billing Of The Snf Pps?"
Post a Comment